Monday Poster Session
Category: General Endoscopy
P2973 - Evaluating the Role of Trainees and AI in Colonoscopy: A Review of Quality Metrics and Departmental Benchmarks
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

John Thesing, DO
University of Kansas School of Medicine - Wichita
Wichita, KS
Presenting Author(s)
John Thesing, DO1, Meagan H. Phox, DO2, Lawerence Zhou, MD3, Kyle Rowe, MD2
1University of Kansas School of Medicine - Wichita, Wichita, KS; 2University of Kansas School of Medicine, Wichita, KS; 3University of Kansas School of Medicine, Park City, KS
Introduction: Colonoscopy quality indicators are measured and monitored to ensure high quality procedures are completed. With new data and enhancement in technology, benchmarks are often changed, and new indicators are measured. When incorporating new indicators into practice, measurement of other factors that may play a role into the established quality measurements, should also be monitored. While not part of the updated 2024 colonoscopy metric guidelines we aimed to monitor the effect of trainee involvement and use of computer aided detection (CADe) artificial intelligence (AI) on our core metrics.
Methods: The project began with a comprehensive review of the 2024 guideline updates, followed by staff education and training on new benchmark metrics. Revised indicators were implemented with ongoing monthly tracking and analysis using descriptive statistics. Measured metrics included Adenoma Detection Rate (ADR), Adenomas Per Colonoscopy (APC), Sessile Serrated Lesion Detection Rate (SSLDR), and Withdrawal Time. We then assessed the influence of trainee (fellow/resident) presence and use of AI on these metrics.
Results: A total of 860 colonoscopies performed from October 2024 to April 2025 were reviewed. The quality indicator metrics were then compared to procedures performed with trainee involvement and without. Furthermore, the same measurements were compared with the use of CADe and without. Trainees were involved in 58.8% of procedures. When trainees were present, ADR was higher (67.0% vs. 60.5%), as were APC (2.29 vs. 1.86) and SSLDR (13.2% vs. 11.1%). Withdrawal time was also longer with trainees (19.88 vs. 10.00 minutes). When CADe was used, ADR was higher (72% vs. 59.5%), as was APC (2.79 vs 1.72) and SSLDR (14.3% vs 11.1%) (Table 1).
Discussion: The 2024 guideline updates broaden the scope of colonoscopy quality metrics to include all indications (with select exceptions). Integration of these metrics into our practice demonstrates improved detection outcomes and highlights the value of continuous monitoring. Trainee participation and the use of CADe was associated with improved quality metrics and longer procedure times, potentially reflecting both enhanced lesion recognition and the time allocated for teaching. Additionally, increased use of CADe during trainee-involved procedures may have contributed to these findings. These differences, however, did not affect whether benchmarks were met.
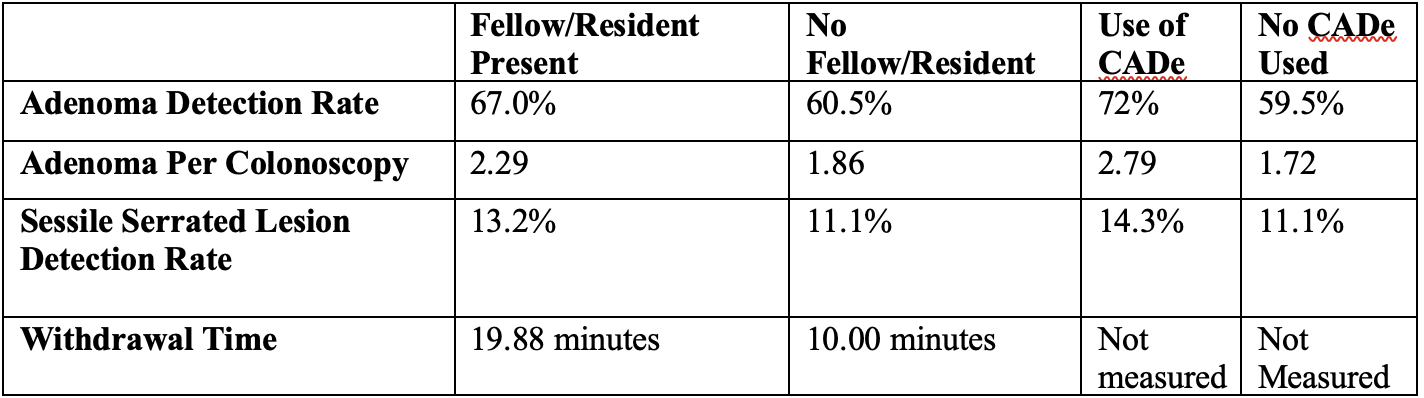
Figure: Table 1: Comparison of Trainee and Use of AI during colonoscopies performed from October 2024 to April 2025.
Disclosures:
John Thesing indicated no relevant financial relationships.
Meagan Phox indicated no relevant financial relationships.
Lawerence Zhou indicated no relevant financial relationships.
Kyle Rowe indicated no relevant financial relationships.
John Thesing, DO1, Meagan H. Phox, DO2, Lawerence Zhou, MD3, Kyle Rowe, MD2. P2973 - Evaluating the Role of Trainees and AI in Colonoscopy: A Review of Quality Metrics and Departmental Benchmarks, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Kansas School of Medicine - Wichita, Wichita, KS; 2University of Kansas School of Medicine, Wichita, KS; 3University of Kansas School of Medicine, Park City, KS
Introduction: Colonoscopy quality indicators are measured and monitored to ensure high quality procedures are completed. With new data and enhancement in technology, benchmarks are often changed, and new indicators are measured. When incorporating new indicators into practice, measurement of other factors that may play a role into the established quality measurements, should also be monitored. While not part of the updated 2024 colonoscopy metric guidelines we aimed to monitor the effect of trainee involvement and use of computer aided detection (CADe) artificial intelligence (AI) on our core metrics.
Methods: The project began with a comprehensive review of the 2024 guideline updates, followed by staff education and training on new benchmark metrics. Revised indicators were implemented with ongoing monthly tracking and analysis using descriptive statistics. Measured metrics included Adenoma Detection Rate (ADR), Adenomas Per Colonoscopy (APC), Sessile Serrated Lesion Detection Rate (SSLDR), and Withdrawal Time. We then assessed the influence of trainee (fellow/resident) presence and use of AI on these metrics.
Results: A total of 860 colonoscopies performed from October 2024 to April 2025 were reviewed. The quality indicator metrics were then compared to procedures performed with trainee involvement and without. Furthermore, the same measurements were compared with the use of CADe and without. Trainees were involved in 58.8% of procedures. When trainees were present, ADR was higher (67.0% vs. 60.5%), as were APC (2.29 vs. 1.86) and SSLDR (13.2% vs. 11.1%). Withdrawal time was also longer with trainees (19.88 vs. 10.00 minutes). When CADe was used, ADR was higher (72% vs. 59.5%), as was APC (2.79 vs 1.72) and SSLDR (14.3% vs 11.1%) (Table 1).
Discussion: The 2024 guideline updates broaden the scope of colonoscopy quality metrics to include all indications (with select exceptions). Integration of these metrics into our practice demonstrates improved detection outcomes and highlights the value of continuous monitoring. Trainee participation and the use of CADe was associated with improved quality metrics and longer procedure times, potentially reflecting both enhanced lesion recognition and the time allocated for teaching. Additionally, increased use of CADe during trainee-involved procedures may have contributed to these findings. These differences, however, did not affect whether benchmarks were met.
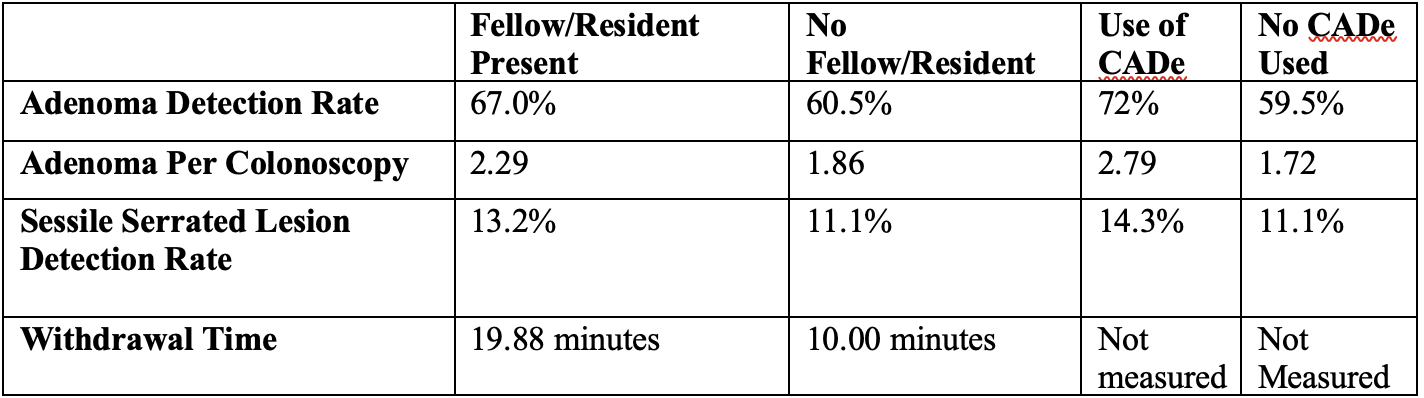
Figure: Table 1: Comparison of Trainee and Use of AI during colonoscopies performed from October 2024 to April 2025.
Disclosures:
John Thesing indicated no relevant financial relationships.
Meagan Phox indicated no relevant financial relationships.
Lawerence Zhou indicated no relevant financial relationships.
Kyle Rowe indicated no relevant financial relationships.
John Thesing, DO1, Meagan H. Phox, DO2, Lawerence Zhou, MD3, Kyle Rowe, MD2. P2973 - Evaluating the Role of Trainees and AI in Colonoscopy: A Review of Quality Metrics and Departmental Benchmarks, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
