Monday Poster Session
Category: Functional Bowel Disease
P2958 - Impact of Socioeconomic Status on Inpatient Outcomes of Gastroparesis in Hospitalized Patients
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ahmed Ali Aziz, MD
INTEGRIS Health Baptist Medical Center
Edmond, OK
Presenting Author(s)
Ahmed Ali Aziz, MD1, Muhammad Ali Aziz, MD2, Rida Zahid, MD3, Muhammad Amir, MD4, Rehan Shah, MD5, Ijlal Akbar. Ali, MD6
1INTEGRIS Health Baptist Medical Center, Edmond, OK; 2University of Kentucky College of Medicine, Lexington, KY; 3Rawalpindi Medical College, Edmond, OK; 4INTEGRIS Health Baptist Medical Center, Oklahoma City, OK; 5CarePoint Health - Bayonne Medical Center, Bayonne, NJ; 6University of Oklahoma, Oklahoma City, OK
Introduction: Gastroparesis (GP) is the delayed gastric emptying in the absence of mechanical obstruction. Evidence suggests that socioeconomic status (SES) may play a critical role in influencing the overall outcomes of GP. Understanding the impact of SES on GP outcomes is essential for addressing healthcare disparities and improving patient care across diverse populations. This study aims to examine the relationship between SES and clinical outcomes of GP in hospitalized patients.
Methods: We used the Nationwide Inpatient Sample (NIS) database from 2020 - 2022 and performed a retrospective analysis of adult patients admitted with GP. Patients with a median income less than $ 66,000 in NIS were classified as low SES (LSES), and those with income greater than $66,000 were classified as high SES (HSES). We compared inpatient outcomes such as in-hospital mortality, hospitalization cost adjusted to the year 2022, length of stay (LOS), odds of sepsis, acute renal failure (ARF), shock and, need for ICU admission. Multivariate regression analysis was used to adjust for confounders.
Results: 31,114 adult patients were admitted for GP, of which 54.5% had LSES and 45.5% had HSES (Table - 1). Patients with LSES had a higher prevalence of CHF (8.49% vs 6.97%), CKD (15.31% vs 11.77 %), DM1 (6.37% vs 5.11%), DM2 (16.02% vs 10.44%), tobacco use (21.68% vs 16.77%) and obesity (18.58% vs 16.6%).
Patients with HSES had longer hospital LOS (aOR: 0.47, 95% CI: -0.24-0.34, P = 0.753), higher total hospitalization costs (+ $1,906.6, 95% CI: -1,664.3 - 5,447.5, P = 0.295) and lesser odds of in-hospital mortality (aOR: 0.57, 95% CI: 0.16-2.05, P = 0.391), shock (aOR: 0.64, 95% CI: 0.26 – 1.61, P = 0.350), sepsis (aOR: 0.77, 95% CI: 0.53 – 1.12, P = 0.181), ARF (aOR: 0.92, 95% CI: 0.79 – 1.08, P = 0.342), and ICU Admission (aOR: 0.88, 95% CI: 0.70 – 1.10, P = 0.279).
Discussion: HSES patients had better GP-related health outcomes likely due to better access to healthcare, better living conditions, higher health literacy, and the ability to seek timely medical care like, earlier diagnosis, and adherence to treatment.
LSES patients had poor GP-related health outcomes likely due to higher prevalence of comorbid conditions, limited access to healthcare, unhealthy living conditions, and lower health literacy.
Resource utilization towards LSES patients can help improve GP-related hospitalization outcomes.
Hospitalized LSES GP patients should receive aggressive treatment to prevent morbidity and mortality.
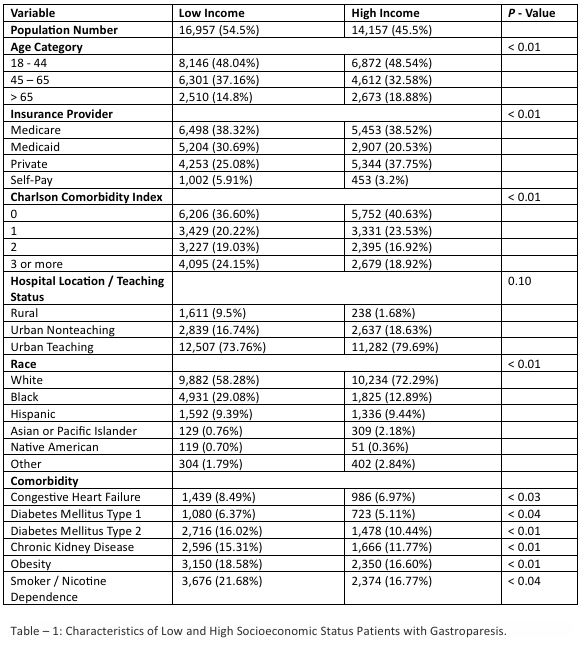
Figure: Table – 1: Characteristics of Low and High Socioeconomic Status Patients with Gastroparesis.
Disclosures:
Ahmed Ali Aziz indicated no relevant financial relationships.
Muhammad Ali Aziz indicated no relevant financial relationships.
Rida Zahid indicated no relevant financial relationships.
Muhammad Amir indicated no relevant financial relationships.
Rehan Shah indicated no relevant financial relationships.
Ijlal Ali indicated no relevant financial relationships.
Ahmed Ali Aziz, MD1, Muhammad Ali Aziz, MD2, Rida Zahid, MD3, Muhammad Amir, MD4, Rehan Shah, MD5, Ijlal Akbar. Ali, MD6. P2958 - Impact of Socioeconomic Status on Inpatient Outcomes of Gastroparesis in Hospitalized Patients, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1INTEGRIS Health Baptist Medical Center, Edmond, OK; 2University of Kentucky College of Medicine, Lexington, KY; 3Rawalpindi Medical College, Edmond, OK; 4INTEGRIS Health Baptist Medical Center, Oklahoma City, OK; 5CarePoint Health - Bayonne Medical Center, Bayonne, NJ; 6University of Oklahoma, Oklahoma City, OK
Introduction: Gastroparesis (GP) is the delayed gastric emptying in the absence of mechanical obstruction. Evidence suggests that socioeconomic status (SES) may play a critical role in influencing the overall outcomes of GP. Understanding the impact of SES on GP outcomes is essential for addressing healthcare disparities and improving patient care across diverse populations. This study aims to examine the relationship between SES and clinical outcomes of GP in hospitalized patients.
Methods: We used the Nationwide Inpatient Sample (NIS) database from 2020 - 2022 and performed a retrospective analysis of adult patients admitted with GP. Patients with a median income less than $ 66,000 in NIS were classified as low SES (LSES), and those with income greater than $66,000 were classified as high SES (HSES). We compared inpatient outcomes such as in-hospital mortality, hospitalization cost adjusted to the year 2022, length of stay (LOS), odds of sepsis, acute renal failure (ARF), shock and, need for ICU admission. Multivariate regression analysis was used to adjust for confounders.
Results: 31,114 adult patients were admitted for GP, of which 54.5% had LSES and 45.5% had HSES (Table - 1). Patients with LSES had a higher prevalence of CHF (8.49% vs 6.97%), CKD (15.31% vs 11.77 %), DM1 (6.37% vs 5.11%), DM2 (16.02% vs 10.44%), tobacco use (21.68% vs 16.77%) and obesity (18.58% vs 16.6%).
Patients with HSES had longer hospital LOS (aOR: 0.47, 95% CI: -0.24-0.34, P = 0.753), higher total hospitalization costs (+ $1,906.6, 95% CI: -1,664.3 - 5,447.5, P = 0.295) and lesser odds of in-hospital mortality (aOR: 0.57, 95% CI: 0.16-2.05, P = 0.391), shock (aOR: 0.64, 95% CI: 0.26 – 1.61, P = 0.350), sepsis (aOR: 0.77, 95% CI: 0.53 – 1.12, P = 0.181), ARF (aOR: 0.92, 95% CI: 0.79 – 1.08, P = 0.342), and ICU Admission (aOR: 0.88, 95% CI: 0.70 – 1.10, P = 0.279).
Discussion: HSES patients had better GP-related health outcomes likely due to better access to healthcare, better living conditions, higher health literacy, and the ability to seek timely medical care like, earlier diagnosis, and adherence to treatment.
LSES patients had poor GP-related health outcomes likely due to higher prevalence of comorbid conditions, limited access to healthcare, unhealthy living conditions, and lower health literacy.
Resource utilization towards LSES patients can help improve GP-related hospitalization outcomes.
Hospitalized LSES GP patients should receive aggressive treatment to prevent morbidity and mortality.
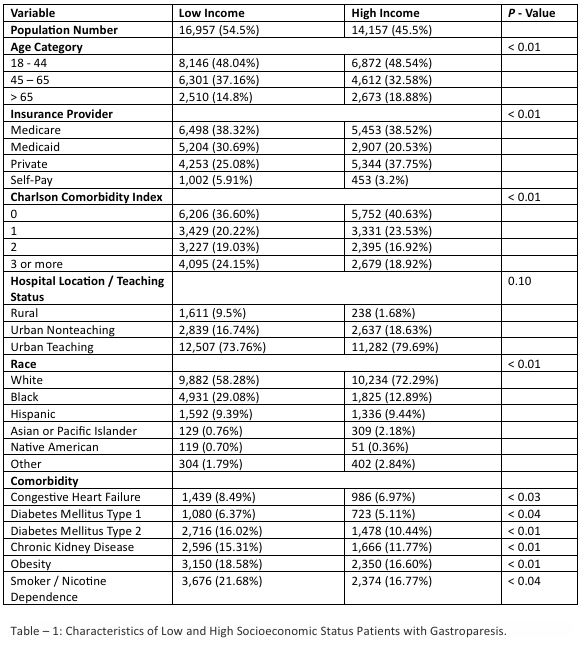
Figure: Table – 1: Characteristics of Low and High Socioeconomic Status Patients with Gastroparesis.
Disclosures:
Ahmed Ali Aziz indicated no relevant financial relationships.
Muhammad Ali Aziz indicated no relevant financial relationships.
Rida Zahid indicated no relevant financial relationships.
Muhammad Amir indicated no relevant financial relationships.
Rehan Shah indicated no relevant financial relationships.
Ijlal Ali indicated no relevant financial relationships.
Ahmed Ali Aziz, MD1, Muhammad Ali Aziz, MD2, Rida Zahid, MD3, Muhammad Amir, MD4, Rehan Shah, MD5, Ijlal Akbar. Ali, MD6. P2958 - Impact of Socioeconomic Status on Inpatient Outcomes of Gastroparesis in Hospitalized Patients, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
