Monday Poster Session
Category: General Endoscopy
P3037 - Persistent Gastro-Gastric Fistula
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Evelyn Inga, MD
University of New Mexico Health Sciences Center
Albuquerque, NM
Presenting Author(s)
Evelyn Inga, MD1, Gregory Grimberg, MD2
1University of New Mexico Hospital, Albuquerque, NM; 2Mercy One North Iowa, Mason City, IA
Introduction: Roux-en-Y Gastric Bypass alters the anatomy of the Gastrointestinal tract and creates a lot of issues with reaching and clearing the biliary tract when choledocholithiasis is noted.
Case Description/
Methods: This is a 60 year old female who underwent a Laparoscopic antegastric antecolic RYGB >15 years ago. Post-operatively she lost >135 lbs. In 2013, she began to have post-prandial pain and persistent nausea and emesis. Workup demonstrated cholelithiasis, elevated bilirubin and transaminitis. Due to the abnormal anatomy post-RYGB, she was sent to the University hospital for an ERCP and a Cholecystectomy. As the Duodenum is now disconnected from the Esophagus, often an advance GI technique called Endoscopic Ultrasound-directed transgastric ERCP (EDGE) involving a lumen-apposing metal stent (LAMS) placement between the gastric pouch and excluded stomach. This then allows for access to the Duodenum from the Esophagus. Usually this is a staged procedure, and the fistula is then closed after the ERCP is performed. After the procedure, the patient had dramatic improvement in post-prandial pain and persistent nausea and emesis. However, several months afterwards, she began feeling malaise, epigastric pain and slowly began regaining some weight. After several months her appetite became voracious and in the last 1.5 years, she has gained >80 lbs so far. She had presented to an ER and a CT Abd/Pelvis (Figure 1a) non-contrast showed a possible GGF. X-ray Upper GI with Small Bowel Follow Through (XR w/ SBFT, Figure 1b) showed: Surgical changes related to Roux-en-Y gastric bypass with most of the contrast opacifying the excluded stomach. Upper Endoscopy showed a large GGF and easy passage of the Gastroscope into the remnant stomach and easy access to the Duodenum without requiring an enteroscope. After realizing that the EDGE technique using a LAMS likely resulted in a persistent fistula, she was sent back to the University Hospital for closure.
Discussion: GGF as a complication of EDGE with LAMS is noted to occur, especially with a prolonged dwelling time of the LAMS ( >89 days), larger diameter (>20 mm), and with Diabetes. After the removal of the LAMS, Argon Plasma Coagulation (APC) of the fistula, followed by endoscopic fistula closure, is performed. Unfortunately, there can be dehiscence or even enlargement that results in a persistent GGF. There are various options to close this persistent GGF: endoscopic full-length suturing or cardiac septal occluder (CSO) placement.
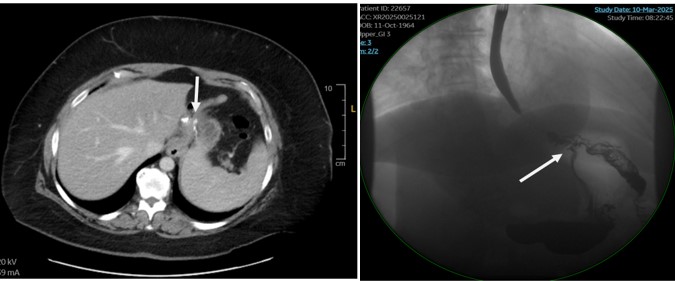
Figure: Figure 1a: CT showing likely GGF indicated by the remnant stomach gastric distention, white arrow indicating breakdown of the staple line.
Figure 1b: UGI w/ SBFT with white arrow showing the GGF .

Figure: Figure 2: Endoscopic visualization. 2A/D showing GGF (white arrow GGF, Black arrow GastroJejunal Anastomosis. 2B showing the Duodenum (which you shouldn’t be able to see after a normal RYGB in an EGD). 2C showing Retroflexion in the remnant stomach (which you shouldn’t be able to see after a normal RYGB in an EGD)
Disclosures:
Evelyn Inga indicated no relevant financial relationships.
Gregory Grimberg indicated no relevant financial relationships.
Evelyn Inga, MD1, Gregory Grimberg, MD2. P3037 - Persistent Gastro-Gastric Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of New Mexico Hospital, Albuquerque, NM; 2Mercy One North Iowa, Mason City, IA
Introduction: Roux-en-Y Gastric Bypass alters the anatomy of the Gastrointestinal tract and creates a lot of issues with reaching and clearing the biliary tract when choledocholithiasis is noted.
Case Description/
Methods: This is a 60 year old female who underwent a Laparoscopic antegastric antecolic RYGB >15 years ago. Post-operatively she lost >135 lbs. In 2013, she began to have post-prandial pain and persistent nausea and emesis. Workup demonstrated cholelithiasis, elevated bilirubin and transaminitis. Due to the abnormal anatomy post-RYGB, she was sent to the University hospital for an ERCP and a Cholecystectomy. As the Duodenum is now disconnected from the Esophagus, often an advance GI technique called Endoscopic Ultrasound-directed transgastric ERCP (EDGE) involving a lumen-apposing metal stent (LAMS) placement between the gastric pouch and excluded stomach. This then allows for access to the Duodenum from the Esophagus. Usually this is a staged procedure, and the fistula is then closed after the ERCP is performed. After the procedure, the patient had dramatic improvement in post-prandial pain and persistent nausea and emesis. However, several months afterwards, she began feeling malaise, epigastric pain and slowly began regaining some weight. After several months her appetite became voracious and in the last 1.5 years, she has gained >80 lbs so far. She had presented to an ER and a CT Abd/Pelvis (Figure 1a) non-contrast showed a possible GGF. X-ray Upper GI with Small Bowel Follow Through (XR w/ SBFT, Figure 1b) showed: Surgical changes related to Roux-en-Y gastric bypass with most of the contrast opacifying the excluded stomach. Upper Endoscopy showed a large GGF and easy passage of the Gastroscope into the remnant stomach and easy access to the Duodenum without requiring an enteroscope. After realizing that the EDGE technique using a LAMS likely resulted in a persistent fistula, she was sent back to the University Hospital for closure.
Discussion: GGF as a complication of EDGE with LAMS is noted to occur, especially with a prolonged dwelling time of the LAMS ( >89 days), larger diameter (>20 mm), and with Diabetes. After the removal of the LAMS, Argon Plasma Coagulation (APC) of the fistula, followed by endoscopic fistula closure, is performed. Unfortunately, there can be dehiscence or even enlargement that results in a persistent GGF. There are various options to close this persistent GGF: endoscopic full-length suturing or cardiac septal occluder (CSO) placement.
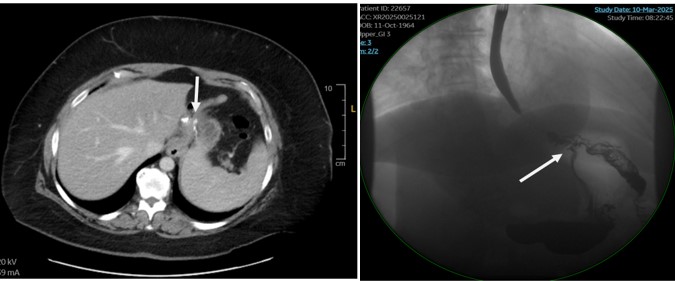
Figure: Figure 1a: CT showing likely GGF indicated by the remnant stomach gastric distention, white arrow indicating breakdown of the staple line.
Figure 1b: UGI w/ SBFT with white arrow showing the GGF .

Figure: Figure 2: Endoscopic visualization. 2A/D showing GGF (white arrow GGF, Black arrow GastroJejunal Anastomosis. 2B showing the Duodenum (which you shouldn’t be able to see after a normal RYGB in an EGD). 2C showing Retroflexion in the remnant stomach (which you shouldn’t be able to see after a normal RYGB in an EGD)
Disclosures:
Evelyn Inga indicated no relevant financial relationships.
Gregory Grimberg indicated no relevant financial relationships.
Evelyn Inga, MD1, Gregory Grimberg, MD2. P3037 - Persistent Gastro-Gastric Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
