Monday Poster Session
Category: General Endoscopy
P3034 - Pneumoperitoneum Following Argon Plasma Coagulation of Gastric and Small Bowel Angiodysplasias
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Tiana Dodd, DO
Charleston Area Medical Center
Charleston, WV
Presenting Author(s)
Tiana Dodd, DO1, Nisar Amin, MD1, Harleen Chela, MD1, Veysel Tahan, MD, FACG2, Ebubekir Daglilar, MD1
1Charleston Area Medical Center, Charleston, WV; 2Northeast Ohio Medical University & CAMC, Charleston, WV
Introduction: Gastrointestinal tract angiodysplasias are abnormal blood vessel tangles that bypass capillary beds, accounting for roughly 5% of upper GI bleeds. Management includes endoscopic therapies such as argon plasma coagulation (APC), laser therapy, and sclerotherapy. Pneumoperitoneum following APC is rare complication that can mimic perforation. If pneumoperitoneum is suspected after APC, a CT scan is necessary to rule out perforation, which may require surgery, whereas non-perforation cases can be managed conservatively.
Case Description/
Methods: 54-year-old female with medical history significant for peripheral artery disease with stent placement and history of upper and lower gastrointestinal tract angiodysplasias. She presented to the hospital with symptomatic anemia. The patient was hemodynamically stable; hemoglobin was 7.9 gm/dL and was transfused one-unit of packed RBCs. Push enteroscopy was performed showing many non-bleeding angiodysplasias in the gastric body, fundus, and cardia, duodenum and proximal jejunum. All gastric and small bowel angiodysplasias were treated with APC. Post procedure, the patient began complaining of pain that started in her chest that moved to her abdomen. The following day the pain became severe, and a physical exam noted the abdomen was tender to palpation without rigidity or rebound tenderness. CT abdomen demonstrated moderate amount of free intraperitoneal air throughout the upper abdomen. A nasogastric tube (NG) was placed to low intermediate suction for gastric decompression and was started on empiric antibiotics with presumed perforation. General surgery recommended to treat conservatively with close monitoring with serial abdominal exams given lack of peritoneal signs on physical exam and no evidence of perforated hollow viscus. The following day the patient’s pain improved significantly, the NG tube was removed, and a clear liquid diet was started. Repeat CT abdomen with contrast showed pneumoperitoneum improved from prior, pain continued to improve, and she was discharged with close follow up.
Discussion: Diagnosis of pneumoperitoneum following endoscopic or surgical intervention should raise concern for perforated hollow viscus as this can be a surgical emergency. It has been reported roughly 90% of cases with reported free intraperitoneal air is a result of perforated hollow viscus. There are only a few documented cases of pneumoperitoneum following APC that were not a result of perforation and resolved by conservative measures alone.
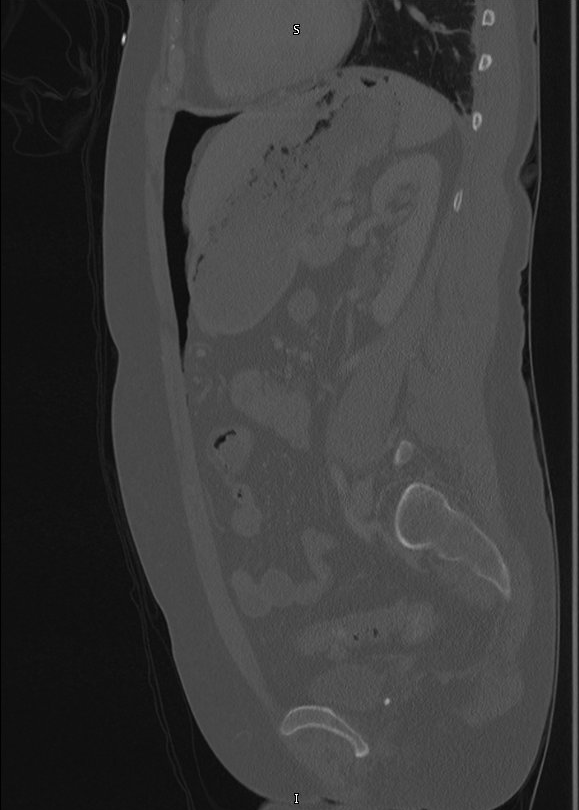
Figure: Figure 1. Small bowel angiodysplasia treated with APC
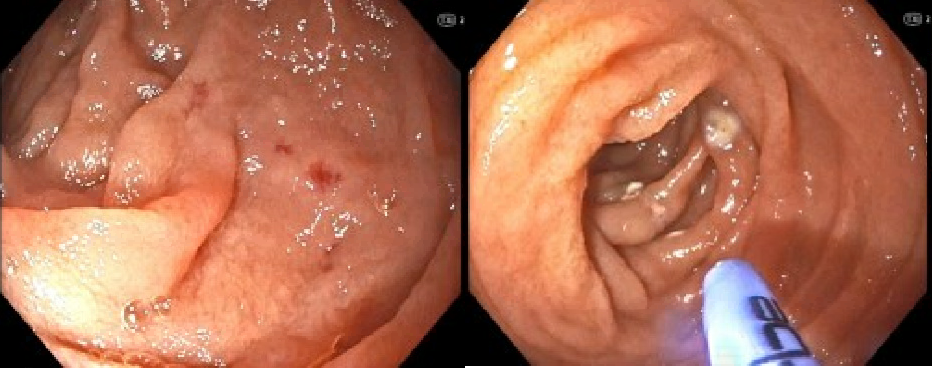
Figure: Figure 2. Moderate amount of free air seen in sagittal views
Disclosures:
Tiana Dodd indicated no relevant financial relationships.
Nisar Amin indicated no relevant financial relationships.
Harleen Chela indicated no relevant financial relationships.
Veysel Tahan indicated no relevant financial relationships.
Ebubekir Daglilar indicated no relevant financial relationships.
Tiana Dodd, DO1, Nisar Amin, MD1, Harleen Chela, MD1, Veysel Tahan, MD, FACG2, Ebubekir Daglilar, MD1. P3034 - Pneumoperitoneum Following Argon Plasma Coagulation of Gastric and Small Bowel Angiodysplasias, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Charleston Area Medical Center, Charleston, WV; 2Northeast Ohio Medical University & CAMC, Charleston, WV
Introduction: Gastrointestinal tract angiodysplasias are abnormal blood vessel tangles that bypass capillary beds, accounting for roughly 5% of upper GI bleeds. Management includes endoscopic therapies such as argon plasma coagulation (APC), laser therapy, and sclerotherapy. Pneumoperitoneum following APC is rare complication that can mimic perforation. If pneumoperitoneum is suspected after APC, a CT scan is necessary to rule out perforation, which may require surgery, whereas non-perforation cases can be managed conservatively.
Case Description/
Methods: 54-year-old female with medical history significant for peripheral artery disease with stent placement and history of upper and lower gastrointestinal tract angiodysplasias. She presented to the hospital with symptomatic anemia. The patient was hemodynamically stable; hemoglobin was 7.9 gm/dL and was transfused one-unit of packed RBCs. Push enteroscopy was performed showing many non-bleeding angiodysplasias in the gastric body, fundus, and cardia, duodenum and proximal jejunum. All gastric and small bowel angiodysplasias were treated with APC. Post procedure, the patient began complaining of pain that started in her chest that moved to her abdomen. The following day the pain became severe, and a physical exam noted the abdomen was tender to palpation without rigidity or rebound tenderness. CT abdomen demonstrated moderate amount of free intraperitoneal air throughout the upper abdomen. A nasogastric tube (NG) was placed to low intermediate suction for gastric decompression and was started on empiric antibiotics with presumed perforation. General surgery recommended to treat conservatively with close monitoring with serial abdominal exams given lack of peritoneal signs on physical exam and no evidence of perforated hollow viscus. The following day the patient’s pain improved significantly, the NG tube was removed, and a clear liquid diet was started. Repeat CT abdomen with contrast showed pneumoperitoneum improved from prior, pain continued to improve, and she was discharged with close follow up.
Discussion: Diagnosis of pneumoperitoneum following endoscopic or surgical intervention should raise concern for perforated hollow viscus as this can be a surgical emergency. It has been reported roughly 90% of cases with reported free intraperitoneal air is a result of perforated hollow viscus. There are only a few documented cases of pneumoperitoneum following APC that were not a result of perforation and resolved by conservative measures alone.
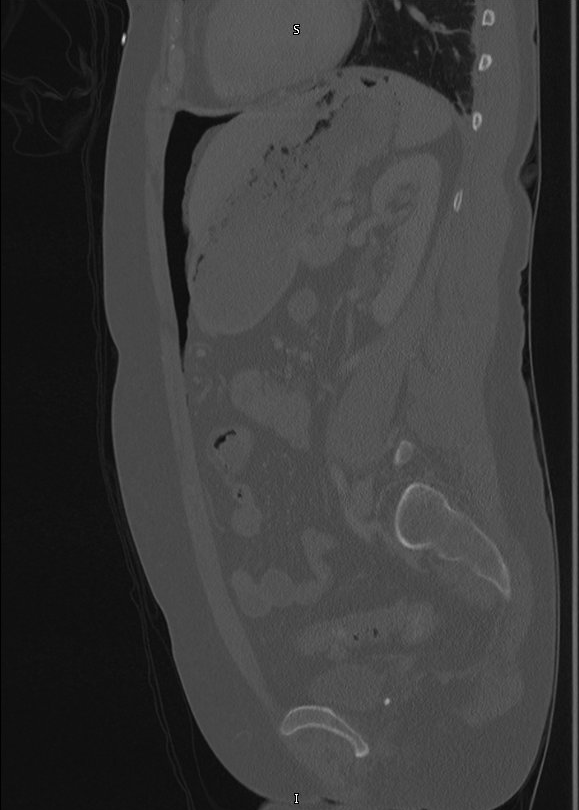
Figure: Figure 1. Small bowel angiodysplasia treated with APC
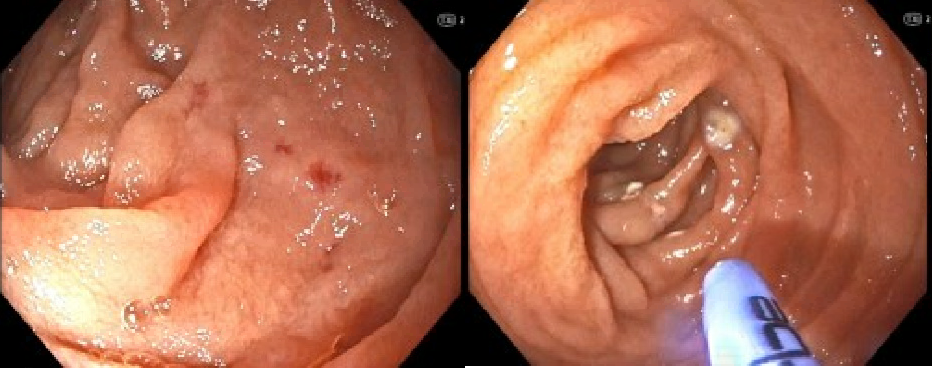
Figure: Figure 2. Moderate amount of free air seen in sagittal views
Disclosures:
Tiana Dodd indicated no relevant financial relationships.
Nisar Amin indicated no relevant financial relationships.
Harleen Chela indicated no relevant financial relationships.
Veysel Tahan indicated no relevant financial relationships.
Ebubekir Daglilar indicated no relevant financial relationships.
Tiana Dodd, DO1, Nisar Amin, MD1, Harleen Chela, MD1, Veysel Tahan, MD, FACG2, Ebubekir Daglilar, MD1. P3034 - Pneumoperitoneum Following Argon Plasma Coagulation of Gastric and Small Bowel Angiodysplasias, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
