Monday Poster Session
Category: General Endoscopy
P3023 - A Second Exit: Double Pylorus as a Complication of NSAID-Induced Peptic Ulcer Disease
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Kimberline Chew, MD
Montefiore Medical Center, Albert Einstein College of Medicine
Bronx, NY
Presenting Author(s)
Kimberline Chew, MD, Jennifer Asotibe, MD, Erica Chung, MD
Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY
Introduction: Double pylorus (DP) is a rare endoscopic finding characterized by a fistulous communication between the gastric antrum and duodenal bulb, typically resulting from peptic ulcer disease (PUD). Recognizing DP is key to guiding appropriate management and avoiding unnecessary interventions. We present a case of an NSAID-induced gastroduodenal fistula – an unusual complication of a common drug.
Case Description/
Methods: An 80-year-old woman with recent NSAID use presented with epigastric pain. She was found to have circumferential antral wall thickening on CT. EGD showed a 2cm cratered ulcer in the duodenal bulb and a mucosal defect at the pylorus creating two channels into the duodenum, consistent with DP (Fig 1). Biopsies of the ulcer and stomach showed chronic gastritis and duodenitis, but were negative for H pylori or malignancy. She was started on acid suppression therapy with pantoprazole, and a follow up EGD 8 weeks later showed a deformity at the pylorus consistent with resolution of DP (Fig 2), with complete healing of the duodenal ulcer.
Discussion: DP refers to an abnormal gastroduodenal fistula that can develop in the setting of penetrating PUD, where an ulcer in the antrum or proximal duodenum erodes through the wall to create a fistulous communication between the two lumens. Common contributing factors include NSAIDs and H pylori infection.
Most cases of DP are found incidentally during EGD, though patients can present with abdominal pain or bleeding related to PUD. Management involves addressing the underlying etiology – discontinuation of NSAIDs, acid suppression therapy, and H pylori eradication. Surgical intervention is rarely required unless complications such as persistent bleeding or obstruction occur.
DP is typically considered a permanent anatomical change, but spontaneous resolution, as in our patient, has been reported in few case reports. It is important to recognize DP as a rare but endoscopically striking complication of PUD to avoid misdiagnoses (e.g. neoplastic fistulas or duplication anomalies) and unnecessary interventions. Our case also serves as a reminder of the mucosal injury potential of NSAIDs and reinforces the need for cautious prescribing, particularly in older and other high-risk populations.
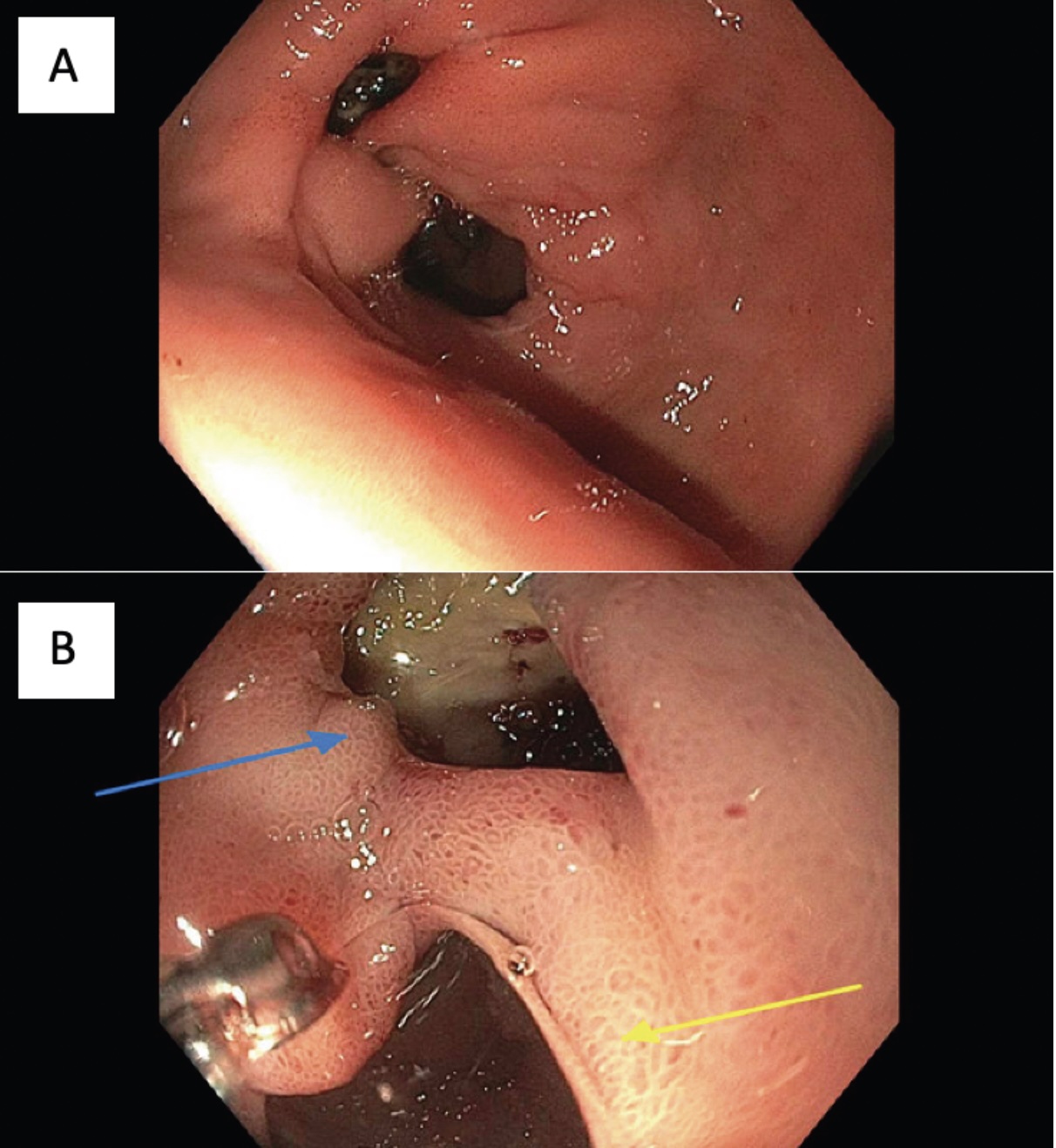
Figure: Figure 1: A. View of the double pylorus from the antrum. B. True pylorus (yellow arrow) and abnormal gastroduodenal fistula (blue arrow), with the duodenal bulb ulcer seen through the gastroduodenal fistula
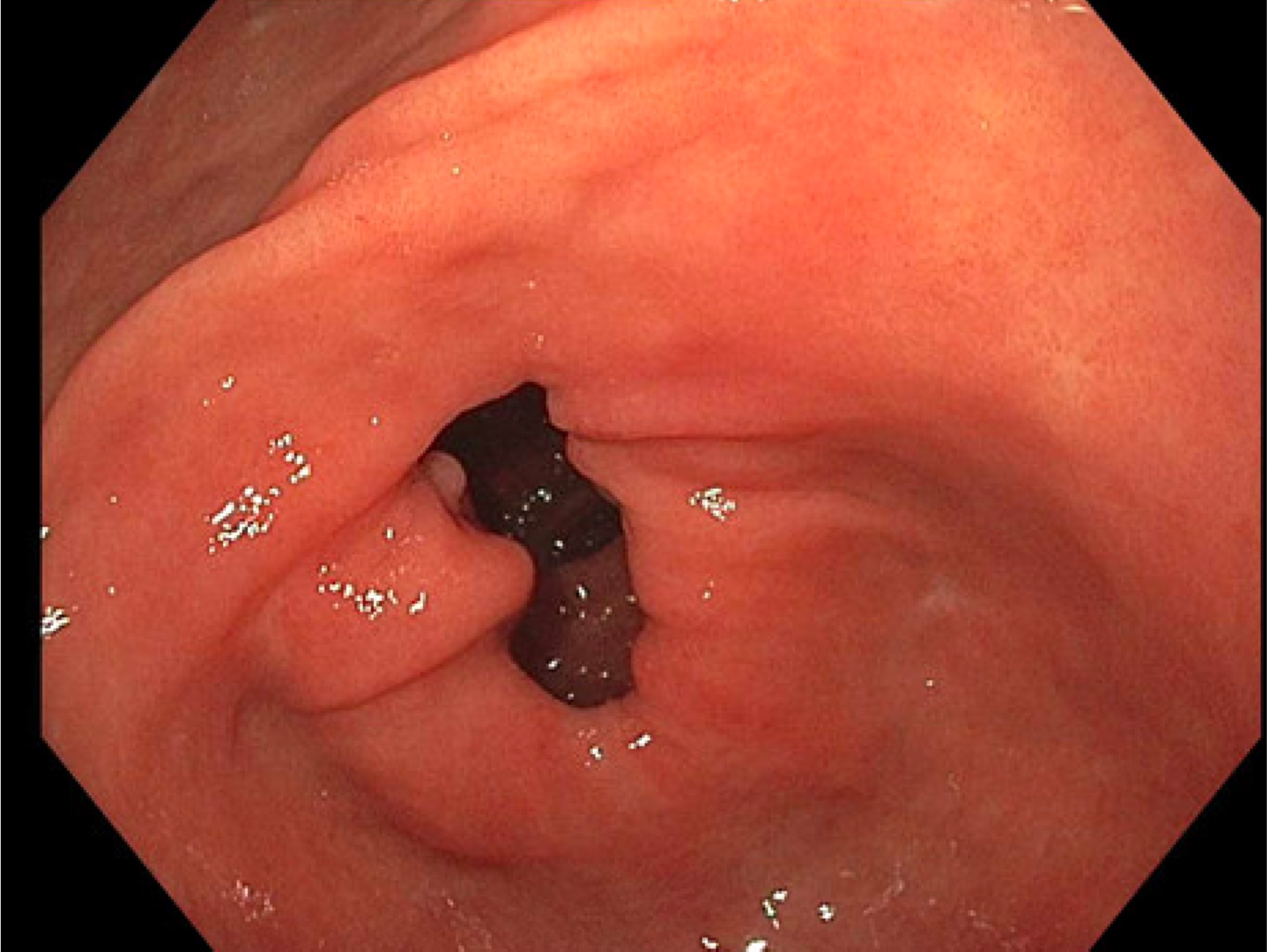
Figure: Figure 2: Follow up EGD 8 weeks later showing deformity at the pylorus consistent with resolution of DP
Disclosures:
Kimberline Chew indicated no relevant financial relationships.
Jennifer Asotibe indicated no relevant financial relationships.
Erica Chung indicated no relevant financial relationships.
Kimberline Chew, MD, Jennifer Asotibe, MD, Erica Chung, MD. P3023 - A Second Exit: Double Pylorus as a Complication of NSAID-Induced Peptic Ulcer Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY
Introduction: Double pylorus (DP) is a rare endoscopic finding characterized by a fistulous communication between the gastric antrum and duodenal bulb, typically resulting from peptic ulcer disease (PUD). Recognizing DP is key to guiding appropriate management and avoiding unnecessary interventions. We present a case of an NSAID-induced gastroduodenal fistula – an unusual complication of a common drug.
Case Description/
Methods: An 80-year-old woman with recent NSAID use presented with epigastric pain. She was found to have circumferential antral wall thickening on CT. EGD showed a 2cm cratered ulcer in the duodenal bulb and a mucosal defect at the pylorus creating two channels into the duodenum, consistent with DP (Fig 1). Biopsies of the ulcer and stomach showed chronic gastritis and duodenitis, but were negative for H pylori or malignancy. She was started on acid suppression therapy with pantoprazole, and a follow up EGD 8 weeks later showed a deformity at the pylorus consistent with resolution of DP (Fig 2), with complete healing of the duodenal ulcer.
Discussion: DP refers to an abnormal gastroduodenal fistula that can develop in the setting of penetrating PUD, where an ulcer in the antrum or proximal duodenum erodes through the wall to create a fistulous communication between the two lumens. Common contributing factors include NSAIDs and H pylori infection.
Most cases of DP are found incidentally during EGD, though patients can present with abdominal pain or bleeding related to PUD. Management involves addressing the underlying etiology – discontinuation of NSAIDs, acid suppression therapy, and H pylori eradication. Surgical intervention is rarely required unless complications such as persistent bleeding or obstruction occur.
DP is typically considered a permanent anatomical change, but spontaneous resolution, as in our patient, has been reported in few case reports. It is important to recognize DP as a rare but endoscopically striking complication of PUD to avoid misdiagnoses (e.g. neoplastic fistulas or duplication anomalies) and unnecessary interventions. Our case also serves as a reminder of the mucosal injury potential of NSAIDs and reinforces the need for cautious prescribing, particularly in older and other high-risk populations.
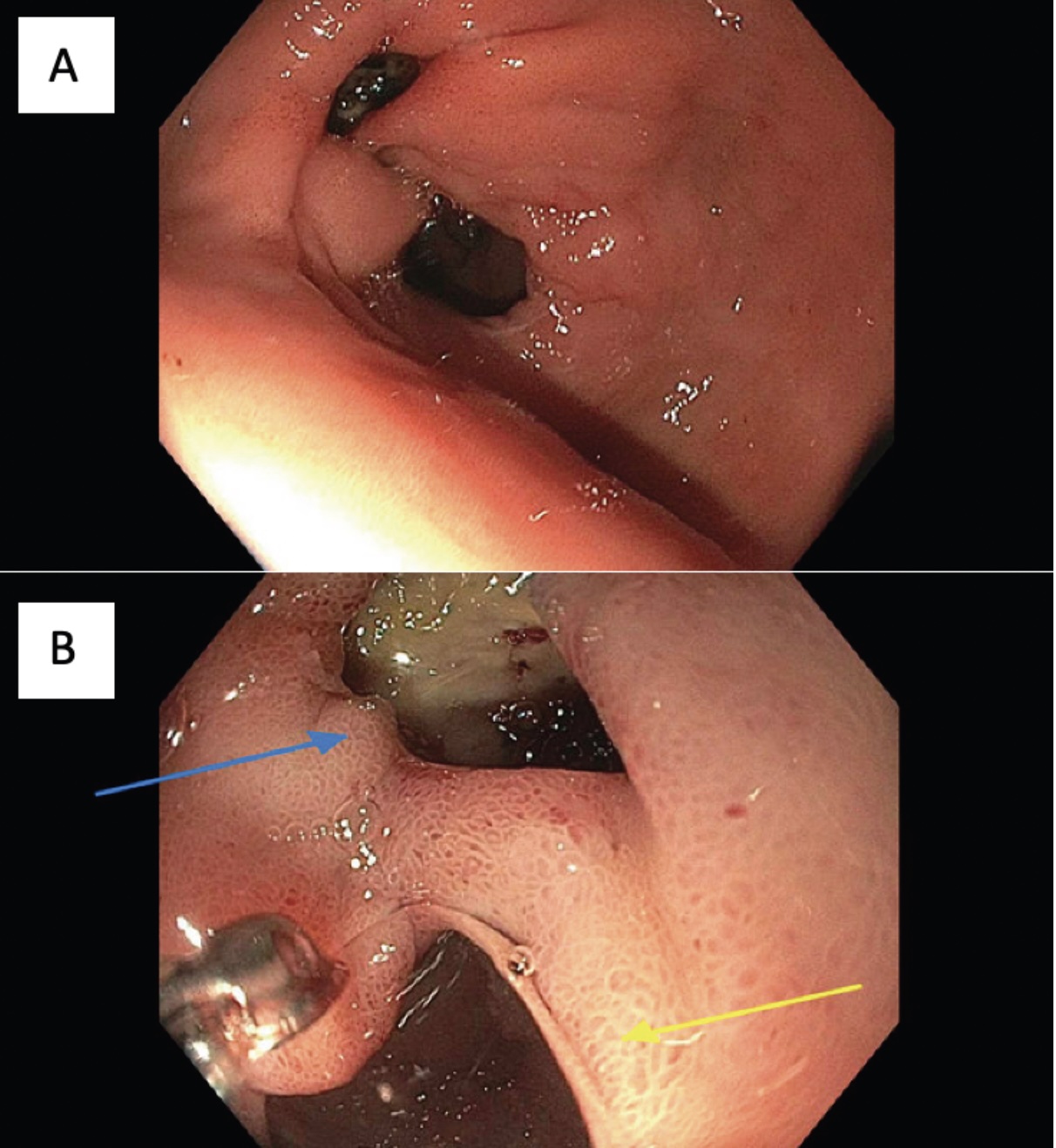
Figure: Figure 1: A. View of the double pylorus from the antrum. B. True pylorus (yellow arrow) and abnormal gastroduodenal fistula (blue arrow), with the duodenal bulb ulcer seen through the gastroduodenal fistula
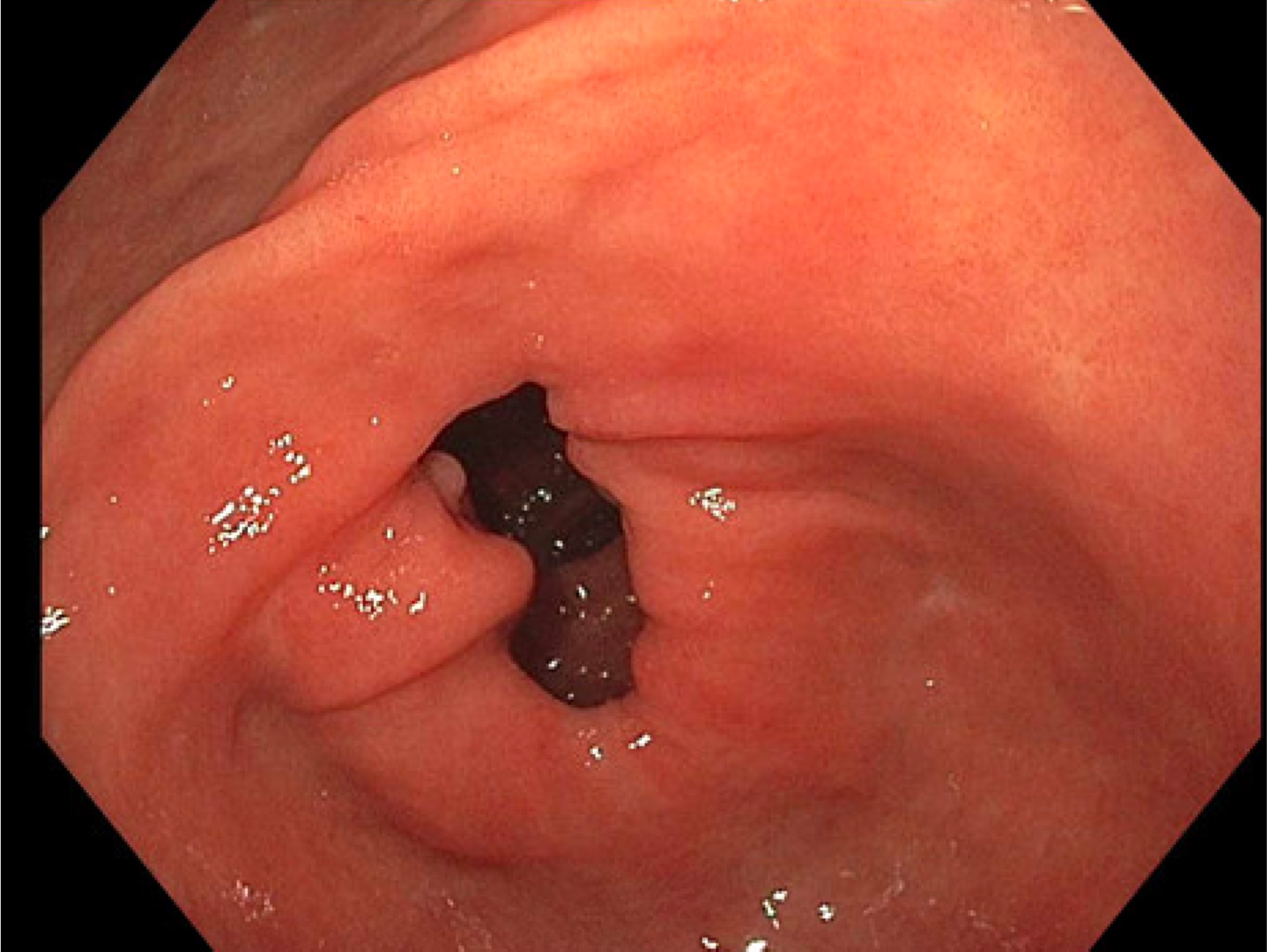
Figure: Figure 2: Follow up EGD 8 weeks later showing deformity at the pylorus consistent with resolution of DP
Disclosures:
Kimberline Chew indicated no relevant financial relationships.
Jennifer Asotibe indicated no relevant financial relationships.
Erica Chung indicated no relevant financial relationships.
Kimberline Chew, MD, Jennifer Asotibe, MD, Erica Chung, MD. P3023 - A Second Exit: Double Pylorus as a Complication of NSAID-Induced Peptic Ulcer Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
