Monday Poster Session
Category: GI Bleeding
P3132 - Life-Threatening Variceal Hemorrhage in MASLD Cirrhosis: A Case for Variant Mesocaval Shunt Placement
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ivan Mogollon, MD
University of Texas Rio Grande Valley
Edinburg, TX
Presenting Author(s)
Ivan Mogollon, MD1, Taiwo Ajani, MD2, Jorge Aboytes Trevino, MD2, Kuang-Wei Chang, MD2
1University of Texas Rio Grande Valley, Edinburg, TX; 2University of Texas Rio Grande Valley, McAllen, TX
Introduction: Variceal hemorrhage is a life-threatening complication of portal hypertension in patients with liver cirrhosis. While transjugular intrahepatic portosystemic shunt (TIPS) is a standard intervention for refractory portal hypertension, chronic portal vein thrombosis can render TIPS technically infeasible. In such complex scenarios, alternative approaches like a variant mesocaval shunt, though rarely performed, may offer a life-saving option by providing portal decompression via an extrahepatic route.
Case Description/
Methods: A 36-year-old woman with MASLD/MASH cirrhosis and known esophageal varices presented to the emergency department with multiple episodes of hematemesis, followed by rapid clinical deterioration and hemorrhagic shock. Her hemoglobin was 6 g/dL, prompting activation of a massive transfusion protocol. While in the emergency department, she had ongoing hematemesis and hematochezia. An emergent EGD revealed large Grade IV esophageal varices, which were partially banded. Additional findings included portal hypertensive gastropathy and gastric varices (Fig. 1). Despite aggressive resuscitation, her bleeding persisted. CT imaging revealed chronic portal vein thrombosis with cavernous transformation, extensive gastric and esophageal varices, along with marked splenomegaly. These findings underscored the severity of portal hypertension and excluded her from TIPS candidacy due to chronic thrombosis and anatomy distorsion of portal vein (Fig. 2).
Discussion: Given her anatomy and clinical instability, she underwent an emergent variant mesocaval shunt procedure, in which a direct extrahepatic connection was created between a short residual segment of the thrombosed main portal vein and the inferior vena cava (IVC), using an 8 cm VIATORR stent. This procedure differs from standard TIPS in that it bypasses the liver entirely, functioning as a mesocaval shunt rather than a portosystemic intrahepatic shunt (Fig. 2). Additionally, she underwent splenic pedicle embolization and coil embolization of portogastric and esophageal varices. Post-procedure, the patient stabilized with no further bleeding and a hemoglobin of 11.2 g/dL.
This case highlights the utility of variant mesocaval shunt placement as a viable rescue therapy in select patients with portal hypertension and chronic portal vein thrombosis, when standard interventions like TIPS are not an option. Early recognition and multidisciplinary coordination are critical in the successful management of such high-risk cases.
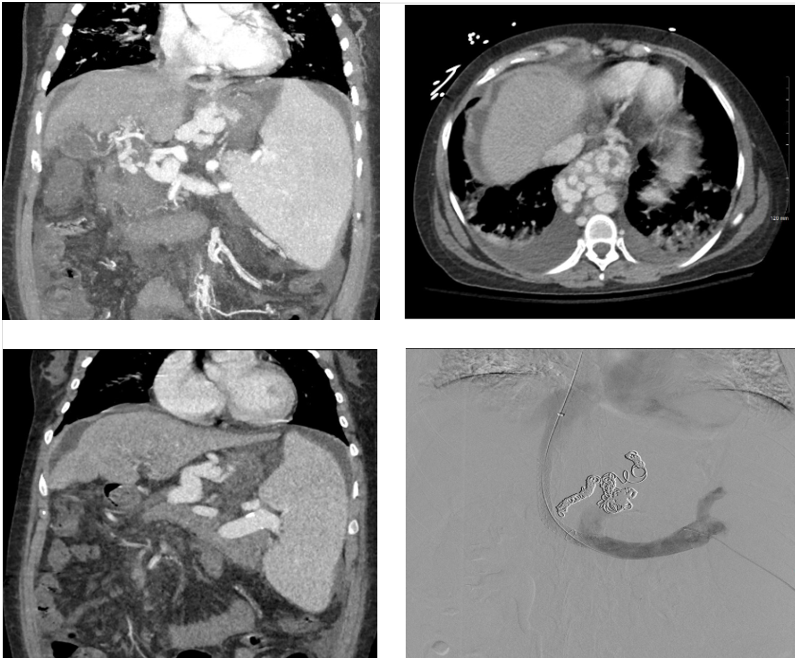
Figure: Fig1. Upper endoscopy consistent with findings of grade IV esophageal varices, gastric varices, and congestive gastropathy in the fundus and body.
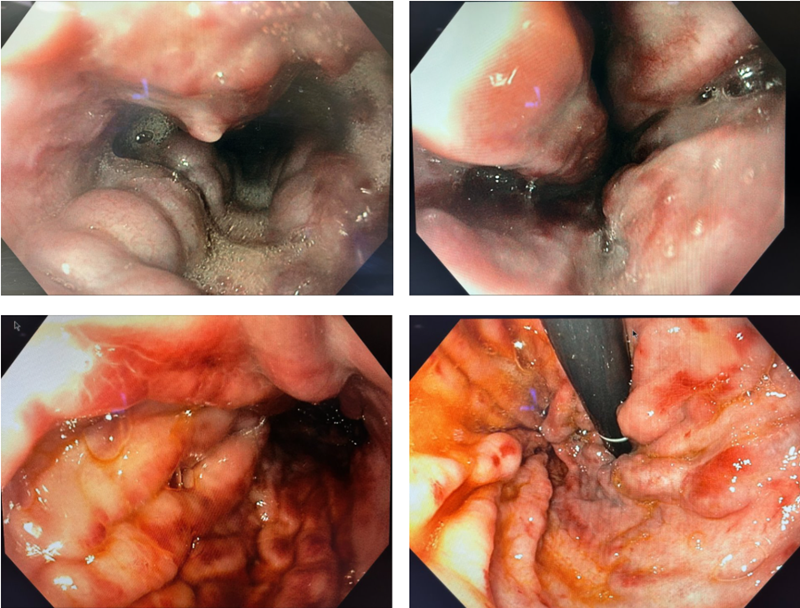
Figure: Fig 2. Coronal and axial contrast-enhanced CT images reveal prominent gastroesophageal varices, marked splenomegaly and cavernous transformation of the portal vein is evident, characterized by multiple serpiginous collateral vessels replacing the expected course of the portal vein. The final image shows a mesocaval shunt, which connects the inferior vena cava (IVC) to the superior mesenteric vein (SMV).
Disclosures:
Ivan Mogollon indicated no relevant financial relationships.
Taiwo Ajani indicated no relevant financial relationships.
Jorge Aboytes Trevino indicated no relevant financial relationships.
Kuang-Wei Chang indicated no relevant financial relationships.
Ivan Mogollon, MD1, Taiwo Ajani, MD2, Jorge Aboytes Trevino, MD2, Kuang-Wei Chang, MD2. P3132 - Life-Threatening Variceal Hemorrhage in MASLD Cirrhosis: A Case for Variant Mesocaval Shunt Placement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Rio Grande Valley, Edinburg, TX; 2University of Texas Rio Grande Valley, McAllen, TX
Introduction: Variceal hemorrhage is a life-threatening complication of portal hypertension in patients with liver cirrhosis. While transjugular intrahepatic portosystemic shunt (TIPS) is a standard intervention for refractory portal hypertension, chronic portal vein thrombosis can render TIPS technically infeasible. In such complex scenarios, alternative approaches like a variant mesocaval shunt, though rarely performed, may offer a life-saving option by providing portal decompression via an extrahepatic route.
Case Description/
Methods: A 36-year-old woman with MASLD/MASH cirrhosis and known esophageal varices presented to the emergency department with multiple episodes of hematemesis, followed by rapid clinical deterioration and hemorrhagic shock. Her hemoglobin was 6 g/dL, prompting activation of a massive transfusion protocol. While in the emergency department, she had ongoing hematemesis and hematochezia. An emergent EGD revealed large Grade IV esophageal varices, which were partially banded. Additional findings included portal hypertensive gastropathy and gastric varices (Fig. 1). Despite aggressive resuscitation, her bleeding persisted. CT imaging revealed chronic portal vein thrombosis with cavernous transformation, extensive gastric and esophageal varices, along with marked splenomegaly. These findings underscored the severity of portal hypertension and excluded her from TIPS candidacy due to chronic thrombosis and anatomy distorsion of portal vein (Fig. 2).
Discussion: Given her anatomy and clinical instability, she underwent an emergent variant mesocaval shunt procedure, in which a direct extrahepatic connection was created between a short residual segment of the thrombosed main portal vein and the inferior vena cava (IVC), using an 8 cm VIATORR stent. This procedure differs from standard TIPS in that it bypasses the liver entirely, functioning as a mesocaval shunt rather than a portosystemic intrahepatic shunt (Fig. 2). Additionally, she underwent splenic pedicle embolization and coil embolization of portogastric and esophageal varices. Post-procedure, the patient stabilized with no further bleeding and a hemoglobin of 11.2 g/dL.
This case highlights the utility of variant mesocaval shunt placement as a viable rescue therapy in select patients with portal hypertension and chronic portal vein thrombosis, when standard interventions like TIPS are not an option. Early recognition and multidisciplinary coordination are critical in the successful management of such high-risk cases.
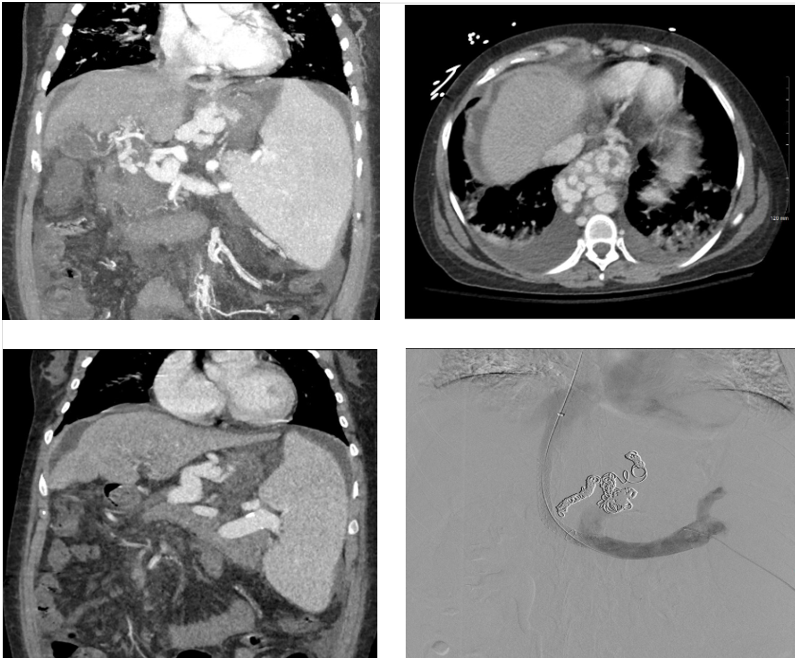
Figure: Fig1. Upper endoscopy consistent with findings of grade IV esophageal varices, gastric varices, and congestive gastropathy in the fundus and body.
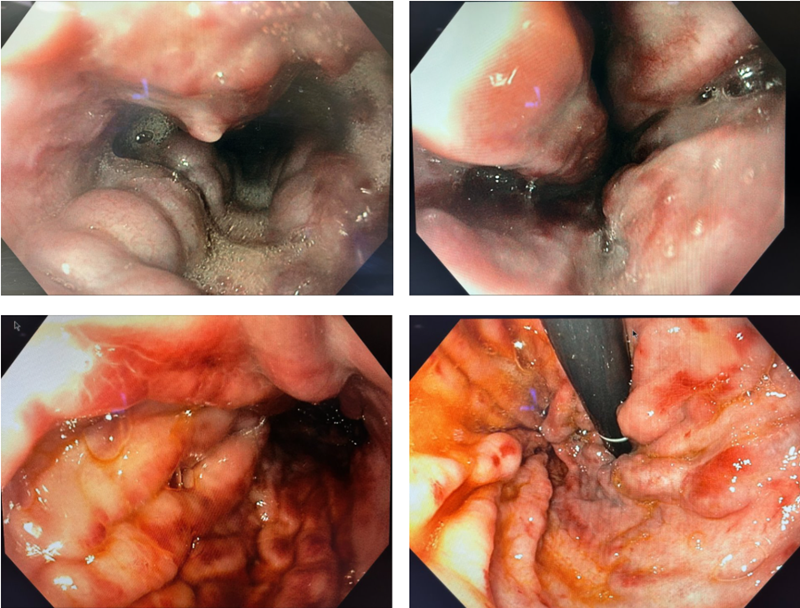
Figure: Fig 2. Coronal and axial contrast-enhanced CT images reveal prominent gastroesophageal varices, marked splenomegaly and cavernous transformation of the portal vein is evident, characterized by multiple serpiginous collateral vessels replacing the expected course of the portal vein. The final image shows a mesocaval shunt, which connects the inferior vena cava (IVC) to the superior mesenteric vein (SMV).
Disclosures:
Ivan Mogollon indicated no relevant financial relationships.
Taiwo Ajani indicated no relevant financial relationships.
Jorge Aboytes Trevino indicated no relevant financial relationships.
Kuang-Wei Chang indicated no relevant financial relationships.
Ivan Mogollon, MD1, Taiwo Ajani, MD2, Jorge Aboytes Trevino, MD2, Kuang-Wei Chang, MD2. P3132 - Life-Threatening Variceal Hemorrhage in MASLD Cirrhosis: A Case for Variant Mesocaval Shunt Placement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
