Monday Poster Session
Category: GI Bleeding
P3127 - When Hepatocellular Carcinoma Crosses the Line: A Case of Tumor Invasion Causing Gastrointestinal Bleeding
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Vivian P. Nguyen, BSA
John Sealy School of Medicine, University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Vivian P. Nguyen, BSA1, Christo Mathew, MD2, Minh Tran, MD2, Julia Zhang, MD2
1John Sealy School of Medicine, University of Texas Medical Branch, Galveston, TX; 2University of Texas Medical Branch, Department of Gastroenterology and Hepatology, Galveston, TX
Introduction: Over 900,000 people are diagnosed with hepatocellular carcinoma (HCC) annually and HCC remains a leading cause of cancer-related mortality worldwide. It is uncommon however for HCC to metastasize to the stomach or cause direct gastric invasion. When this does occur, patients can present with gastrointestinal bleeding or be misdiagnosed with a primary gastric cancer with liver metastases, complicating diagnosis and treatment. We present a rare case of HCC with direct invasion of the gastric body.
Case Description/
Methods: A 63-year-old man with untreated hepatitis C virus infection initially presented with reports of abdominal pain. A computed tomography scan revealed cirrhosis with signs of portal hypertension including splenomegaly and esophageal varices along with multiple left hepatic lobe masses, the largest measuring 13 cm and causing significant mass effect on the stomach. Laboratory testing showed an alpha-fetoprotein level of 78,400. Magnetic resonance imaging confirmed the 13 cm exophytic left hepatic lobe mass as being compatible with HCC with suspected gastric wall invasion along with a focus of distal portal vein thrombosis. The patient had left against medical advice but re-presented shortly afterwards with reported melena and a significant drop in hemoglobin. Esophagogastroduodenoscopy was done and revealed nonbleeding grade 1 varices and a large, ulcerated mass in the gastric body, consistent with direct invasion from HCC. The mass was not actively bleeding at the time of exam and no acute interventions were needed. The patient was discharged in stable condition with plans to discuss treatment options with Oncology outpatient.
Discussion: Direct gastric invasion by HCC occurs in approximately 0.5% of HCC cases and can commonly present with overt gastrointestinal bleeding. Although rare, bleeding related to direct invasion by tumor should always be considered in addition to more common etiologies like peptic ulcer disease and variceal bleeding, as it can alter prognosis and management. Successful endoscopic hemostasis is rare in these cases and more oftentimes, treatment may require transarterial embolization and surgical measures. Overall, extrahepatic spread of HCC protends poor prognosis. Treatment plans may involve trans-arterial chemoembolization, radiotherapy, systemic chemotherapy, and surgery. This case contributes to the limited literature and underscores the importance of recognizing this uncommon disease process.
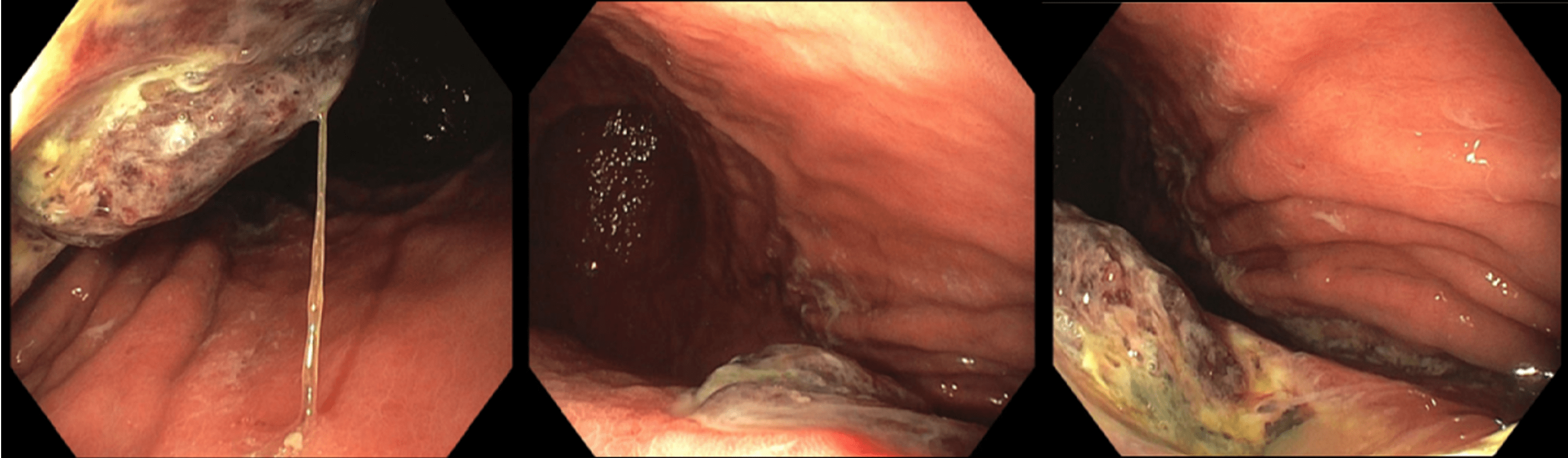
Figure: Figure 1. Ulcerated infiltrating mass on the greater curvature of the gastric body, likely from direct invasion of HCC.
Disclosures:
Vivian Nguyen indicated no relevant financial relationships.
Christo Mathew indicated no relevant financial relationships.
Minh Tran indicated no relevant financial relationships.
Julia Zhang indicated no relevant financial relationships.
Vivian P. Nguyen, BSA1, Christo Mathew, MD2, Minh Tran, MD2, Julia Zhang, MD2. P3127 - When Hepatocellular Carcinoma Crosses the Line: A Case of Tumor Invasion Causing Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1John Sealy School of Medicine, University of Texas Medical Branch, Galveston, TX; 2University of Texas Medical Branch, Department of Gastroenterology and Hepatology, Galveston, TX
Introduction: Over 900,000 people are diagnosed with hepatocellular carcinoma (HCC) annually and HCC remains a leading cause of cancer-related mortality worldwide. It is uncommon however for HCC to metastasize to the stomach or cause direct gastric invasion. When this does occur, patients can present with gastrointestinal bleeding or be misdiagnosed with a primary gastric cancer with liver metastases, complicating diagnosis and treatment. We present a rare case of HCC with direct invasion of the gastric body.
Case Description/
Methods: A 63-year-old man with untreated hepatitis C virus infection initially presented with reports of abdominal pain. A computed tomography scan revealed cirrhosis with signs of portal hypertension including splenomegaly and esophageal varices along with multiple left hepatic lobe masses, the largest measuring 13 cm and causing significant mass effect on the stomach. Laboratory testing showed an alpha-fetoprotein level of 78,400. Magnetic resonance imaging confirmed the 13 cm exophytic left hepatic lobe mass as being compatible with HCC with suspected gastric wall invasion along with a focus of distal portal vein thrombosis. The patient had left against medical advice but re-presented shortly afterwards with reported melena and a significant drop in hemoglobin. Esophagogastroduodenoscopy was done and revealed nonbleeding grade 1 varices and a large, ulcerated mass in the gastric body, consistent with direct invasion from HCC. The mass was not actively bleeding at the time of exam and no acute interventions were needed. The patient was discharged in stable condition with plans to discuss treatment options with Oncology outpatient.
Discussion: Direct gastric invasion by HCC occurs in approximately 0.5% of HCC cases and can commonly present with overt gastrointestinal bleeding. Although rare, bleeding related to direct invasion by tumor should always be considered in addition to more common etiologies like peptic ulcer disease and variceal bleeding, as it can alter prognosis and management. Successful endoscopic hemostasis is rare in these cases and more oftentimes, treatment may require transarterial embolization and surgical measures. Overall, extrahepatic spread of HCC protends poor prognosis. Treatment plans may involve trans-arterial chemoembolization, radiotherapy, systemic chemotherapy, and surgery. This case contributes to the limited literature and underscores the importance of recognizing this uncommon disease process.
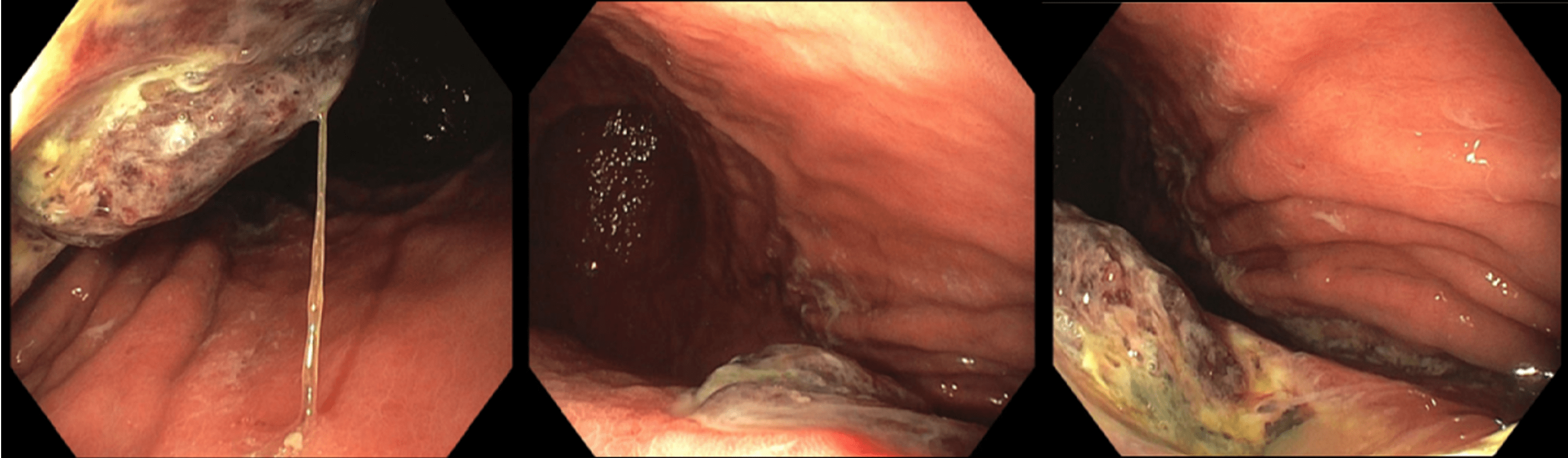
Figure: Figure 1. Ulcerated infiltrating mass on the greater curvature of the gastric body, likely from direct invasion of HCC.
Disclosures:
Vivian Nguyen indicated no relevant financial relationships.
Christo Mathew indicated no relevant financial relationships.
Minh Tran indicated no relevant financial relationships.
Julia Zhang indicated no relevant financial relationships.
Vivian P. Nguyen, BSA1, Christo Mathew, MD2, Minh Tran, MD2, Julia Zhang, MD2. P3127 - When Hepatocellular Carcinoma Crosses the Line: A Case of Tumor Invasion Causing Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

