Monday Poster Session
Category: GI Bleeding
P3126 - Cecal Dieulafoy’s Lesion Presenting as Post-Polypectomy Hematochezia: A Rare and Overlooked Cause of Lower GI Bleeding
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Leith Ghani, DO (he/him/his)
University of Arizona College of Medicine, Phoenix VA Medical Center
Phoenix, AZ
Presenting Author(s)
Leith Ghani, DO1, Majd Aboona, MD2, Diwanshu Soni, DO3, Dayna Telken, 2, Hugo L.. Pinillos, MD, FACG4
1University of Arizona College of Medicine, Phoenix VA Medical Center, Phoenix, AZ; 2University of Arizona College of Medicine - Phoenix, Phoenix, AZ; 3University of Arizona College of Medicine, Phoenix, Phoenix, AZ; 4Phoenix VA Health Care System, Phoenix, AZ
Introduction: Dieulafoy’s lesions (DLs) are a rare but life-threatening source of gastrointestinal hemorrhage, caused by a large-caliber submucosal artery that erodes through a small mucosal defect without associated ulceration. While typically gastric, colonic DLs are rare, comprising < 2% of cases. We report a case of a 70-year-old male who presented with hematochezia eight days after screening colonoscopy with polypectomy. A cecal DL was identified on endoscopy and successfully managed with hemoclipping and epinephrine injection.
Case Description/
Methods: A 70-year-old male with HTN, T2DM, HLD, CKD stage 2, MASLD, diverticulosis, and internal hemorrhoids presented with three episodes of bright red blood per rectum and associated lightheadedness. Eight days earlier, he had a screening colonoscopy with cold snare removal of two 3 mm hyperplastic polyps in the cecum and descending colon.
On arrival, he was tachycardic (126 bpm) and hypotensive. Labs revealed hemoglobin of 13.8 g/dL, later falling to 10.6 g/dL, and then to ~8 g/dL during a syncopal episode. CT angiography showed no active extravasation but was limited by hip prosthesis artifact.
Colonoscopy on hospital day 2 revealed active bleeding from a DL near the appendiceal orifice (Figures 1A and 1B), distinct from the previous polypectomy site (Figure 1C). Three hemoclips were placed (Figure 1D), and epinephrine was injected to achieve hemostasis. The patient remained stable with no further bleeding. He was discharged in stable condition with plans for outpatient follow-up.
Discussion: Colonic DLs are rare and often underrecognized causes of lower GI bleeding. These lesions involve a dilated submucosal artery that can cause significant hemorrhage through a small mucosal defect. While gastric DLs are well documented, cecal lesions may be mistaken for more common causes like diverticulosis or post-polypectomy bleeding.
This case is notable for its temporal proximity to colonoscopy, which initially led to suspicion of post-polypectomy bleeding. However, endoscopy localized the DL near the appendiceal orifice, far from the prior polypectomy site, emphasizing the need for careful mucosal inspection.
CTA was inconclusive illustrating the limits of radiographic imaging. Colonoscopy remains the diagnostic and therapeutic gold standard. Endoscopic treatment using epinephrine and hemoclips is highly effective in achieving hemostasis and preventing rebleeding. Prompt recognition and intervention can be lifesaving and may prevent surgical approaches.
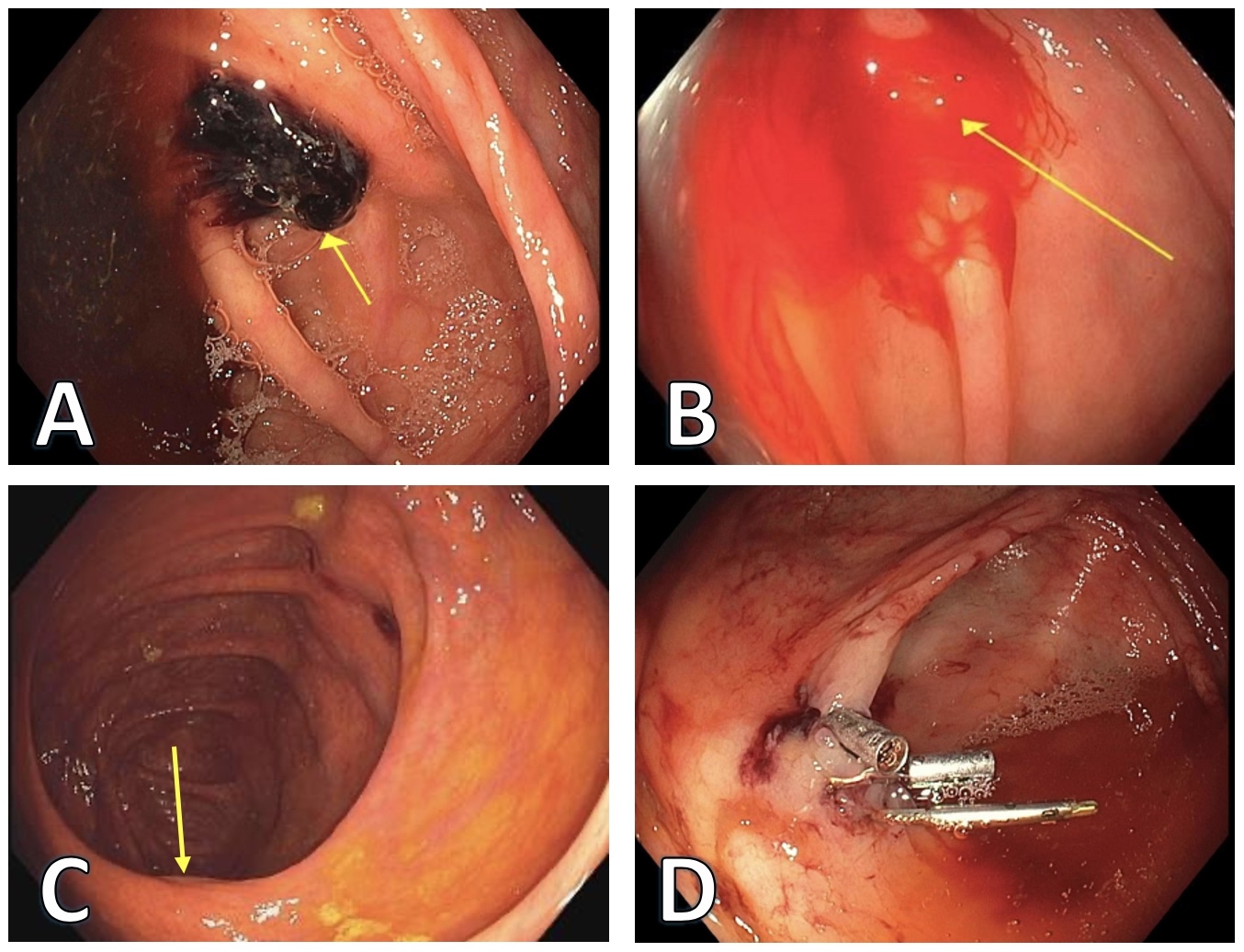
Figure: Figure 1. A: Blood Clot overlying cecal Dieulafoy’s lesion adjacent to the appendiceal orifice just proximal from the IC Valve. B: Active bleeding from cecal Dieulafoy’s lesion. C: Polypectomy site, opposite to the IC valve at the border between cecum and AC. D: 3 Hemoclips placed on the Dieulafoy’s lesion.
Disclosures:
Leith Ghani indicated no relevant financial relationships.
Majd Aboona indicated no relevant financial relationships.
Diwanshu Soni indicated no relevant financial relationships.
Dayna Telken indicated no relevant financial relationships.
Hugo Pinillos indicated no relevant financial relationships.
Leith Ghani, DO1, Majd Aboona, MD2, Diwanshu Soni, DO3, Dayna Telken, 2, Hugo L.. Pinillos, MD, FACG4. P3126 - Cecal Dieulafoy’s Lesion Presenting as Post-Polypectomy Hematochezia: A Rare and Overlooked Cause of Lower GI Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Arizona College of Medicine, Phoenix VA Medical Center, Phoenix, AZ; 2University of Arizona College of Medicine - Phoenix, Phoenix, AZ; 3University of Arizona College of Medicine, Phoenix, Phoenix, AZ; 4Phoenix VA Health Care System, Phoenix, AZ
Introduction: Dieulafoy’s lesions (DLs) are a rare but life-threatening source of gastrointestinal hemorrhage, caused by a large-caliber submucosal artery that erodes through a small mucosal defect without associated ulceration. While typically gastric, colonic DLs are rare, comprising < 2% of cases. We report a case of a 70-year-old male who presented with hematochezia eight days after screening colonoscopy with polypectomy. A cecal DL was identified on endoscopy and successfully managed with hemoclipping and epinephrine injection.
Case Description/
Methods: A 70-year-old male with HTN, T2DM, HLD, CKD stage 2, MASLD, diverticulosis, and internal hemorrhoids presented with three episodes of bright red blood per rectum and associated lightheadedness. Eight days earlier, he had a screening colonoscopy with cold snare removal of two 3 mm hyperplastic polyps in the cecum and descending colon.
On arrival, he was tachycardic (126 bpm) and hypotensive. Labs revealed hemoglobin of 13.8 g/dL, later falling to 10.6 g/dL, and then to ~8 g/dL during a syncopal episode. CT angiography showed no active extravasation but was limited by hip prosthesis artifact.
Colonoscopy on hospital day 2 revealed active bleeding from a DL near the appendiceal orifice (Figures 1A and 1B), distinct from the previous polypectomy site (Figure 1C). Three hemoclips were placed (Figure 1D), and epinephrine was injected to achieve hemostasis. The patient remained stable with no further bleeding. He was discharged in stable condition with plans for outpatient follow-up.
Discussion: Colonic DLs are rare and often underrecognized causes of lower GI bleeding. These lesions involve a dilated submucosal artery that can cause significant hemorrhage through a small mucosal defect. While gastric DLs are well documented, cecal lesions may be mistaken for more common causes like diverticulosis or post-polypectomy bleeding.
This case is notable for its temporal proximity to colonoscopy, which initially led to suspicion of post-polypectomy bleeding. However, endoscopy localized the DL near the appendiceal orifice, far from the prior polypectomy site, emphasizing the need for careful mucosal inspection.
CTA was inconclusive illustrating the limits of radiographic imaging. Colonoscopy remains the diagnostic and therapeutic gold standard. Endoscopic treatment using epinephrine and hemoclips is highly effective in achieving hemostasis and preventing rebleeding. Prompt recognition and intervention can be lifesaving and may prevent surgical approaches.
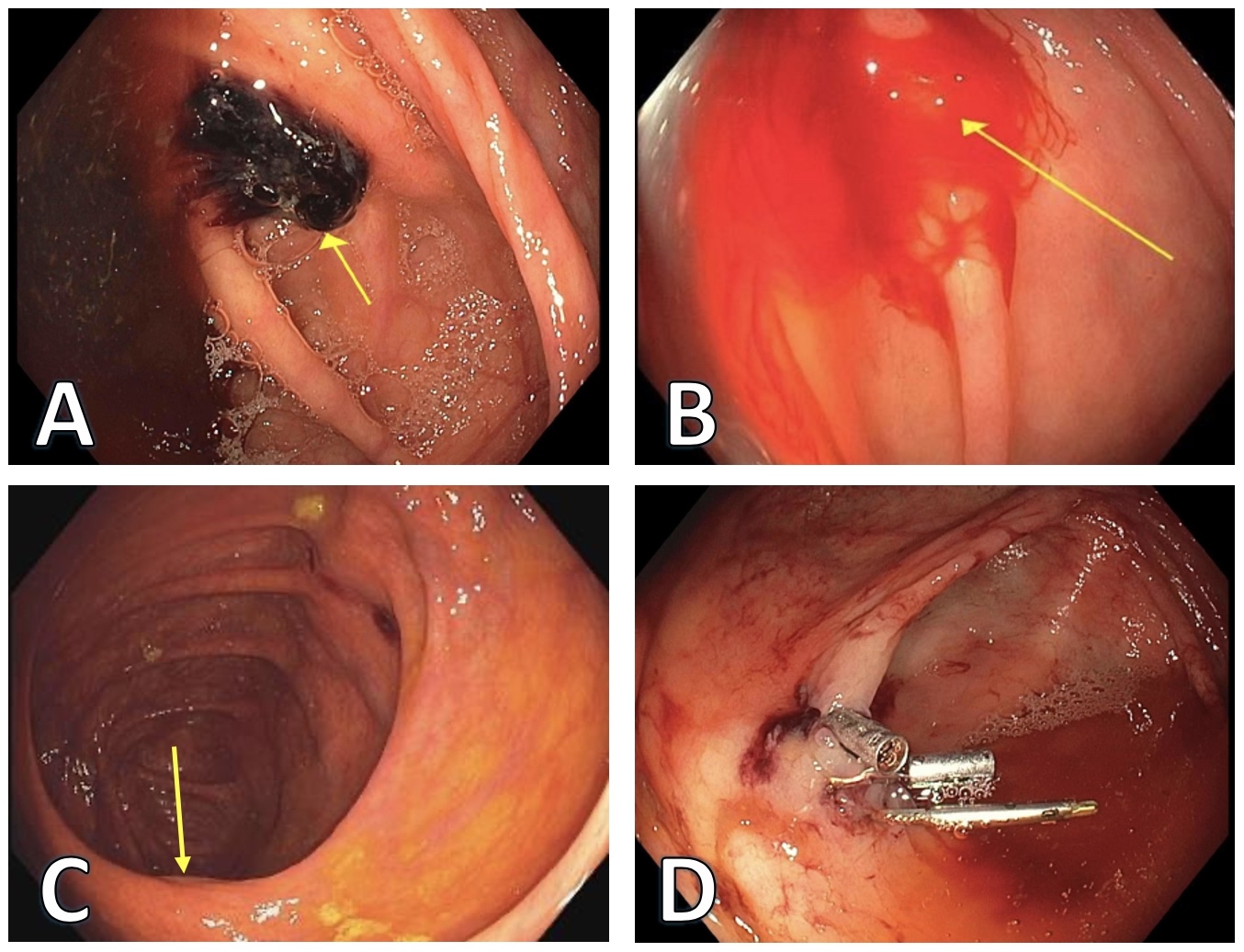
Figure: Figure 1. A: Blood Clot overlying cecal Dieulafoy’s lesion adjacent to the appendiceal orifice just proximal from the IC Valve. B: Active bleeding from cecal Dieulafoy’s lesion. C: Polypectomy site, opposite to the IC valve at the border between cecum and AC. D: 3 Hemoclips placed on the Dieulafoy’s lesion.
Disclosures:
Leith Ghani indicated no relevant financial relationships.
Majd Aboona indicated no relevant financial relationships.
Diwanshu Soni indicated no relevant financial relationships.
Dayna Telken indicated no relevant financial relationships.
Hugo Pinillos indicated no relevant financial relationships.
Leith Ghani, DO1, Majd Aboona, MD2, Diwanshu Soni, DO3, Dayna Telken, 2, Hugo L.. Pinillos, MD, FACG4. P3126 - Cecal Dieulafoy’s Lesion Presenting as Post-Polypectomy Hematochezia: A Rare and Overlooked Cause of Lower GI Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
