Monday Poster Session
Category: GI Bleeding
P3123 - A Rare Case of Duodenal Diverticular Bleeding: Challenges and Endoscopic Approach
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mark Stasiewicz, MD
Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas
Las Vegas, NV
Presenting Author(s)
Mark Stasiewicz, MD1, Kenneth Chow, MD2, Amrit Narwan, MD1, Jose Aponte-Pieras, MD1
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, Las Vegas, NV
Introduction: Duodenal diverticulosis is a common anatomical finding, however, duodenal diverticular bleeding (DDB) resulting in overt clinical signs and symptoms is exceedingly rare, accounting for less than 1% of upper gastrointestinal bleeding cases. Given its frequently concealed nature, DDB poses significant diagnostic and therapeutic challenges. We report a rare case of DDB in a critically ill patient, outlining the diagnostic complexities and detailing endoscopic strategies employed for management.
Case Description/
Methods: A 68-year-old man with end-stage renal disease on hemodialysis, decompensated cirrhosis, heart failure with preserved ejection fraction, and a recent course of severe COVID-19 presented with melena and profound anemia (Hgb 4.6 g/dL). He arrived by ambulance from a long-term care facility where he had been receiving low-dose norepinephrine for refractory hypotension and was admitted to the ICU. Index esophagogastroduodenoscopy (EGD) revealed multiple duodenal angioectasias which were treated with argon plasma coagulation, and a duodenal diverticulum with an impacted fibrotic mucus plug in the posterior wall of the duodenal bulb. On hospital day 5, recurrent hematochezia necessitated repeat endoscopy, this time with visualization of active bleeding from the diverticulum. Attempts to dislodge the fibrous cap failed, but hemostasis was achieved by means of injection with 5 cc of 1:10,000 epinephrine within and around the diverticulum, subsequently a clip specialized in closure of mucosal defects was used to appose the mouth of the diverticulum with successful tamponade. The patient required a total of 11 units of packed red blood cells and was discharged to a long-term care facility after tracheostomy and feeding tube placement.
Discussion: This case highlights the diagnostic challenges associated with DDB, especially when the culprit vessel is masked by debris, or is located within an endoscopically inaccessible diverticulum. Adequate endoscopic hemostasis may require the use of multiple modalities, including hemoclip placement, epinephrine injection, or thermal cautery. If all other methods fail to identify and treat the source of bleeding, catheter angiography and embolization may be employed to achieve hemostasis. Prompt identification of and intervention against DDB is critical to minimize prolonged hospitalization, transfusion burden, and mortality. More case reports are needed to raise awareness of techniques shown to provide satisfactory hemostasis in complex cases of DDB.
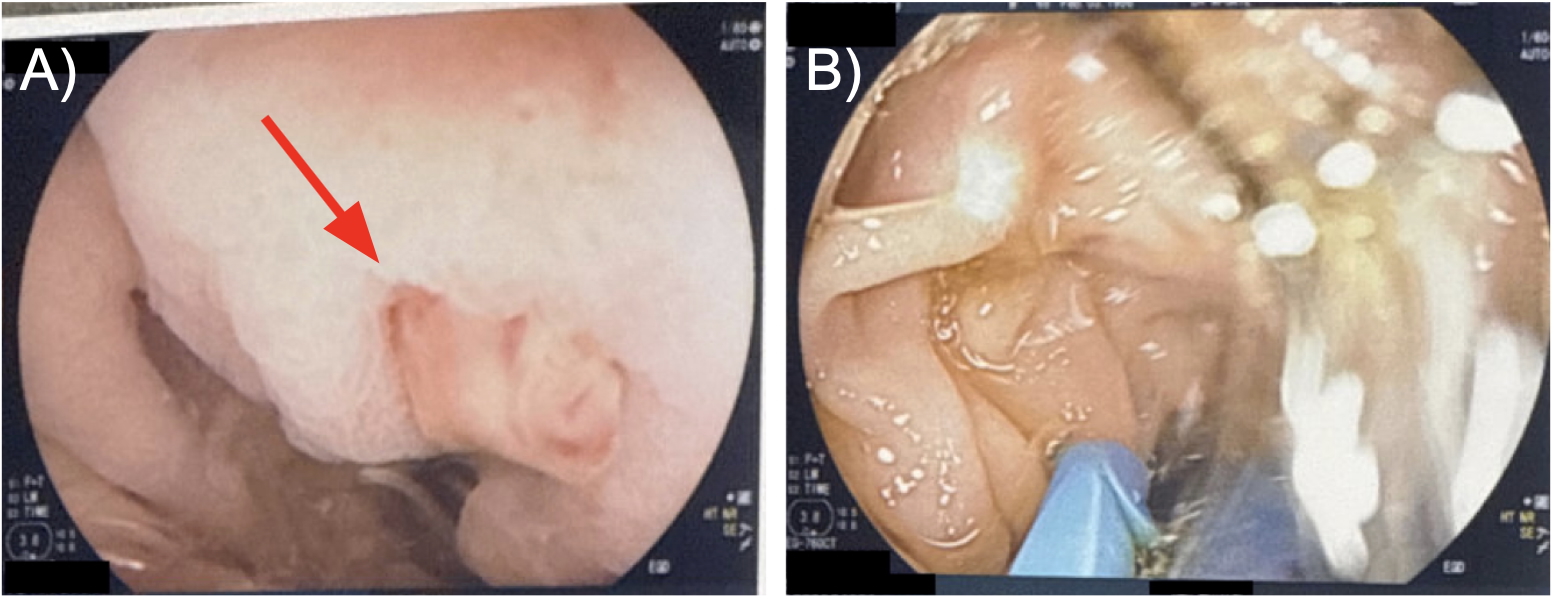
Figure: Figure 1. Findings from index EGD on hospital day 1. A) Fibrous cap (red arrow) noted obstructing view of the duodenal diverticulum. B) Attempt at mechanical dislodgment of fibrous cap from duodenal diverticulum.
Disclosures:
Mark Stasiewicz indicated no relevant financial relationships.
Kenneth Chow indicated no relevant financial relationships.
Amrit Narwan indicated no relevant financial relationships.
Jose Aponte-Pieras indicated no relevant financial relationships.
Mark Stasiewicz, MD1, Kenneth Chow, MD2, Amrit Narwan, MD1, Jose Aponte-Pieras, MD1. P3123 - A Rare Case of Duodenal Diverticular Bleeding: Challenges and Endoscopic Approach, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, Las Vegas, NV
Introduction: Duodenal diverticulosis is a common anatomical finding, however, duodenal diverticular bleeding (DDB) resulting in overt clinical signs and symptoms is exceedingly rare, accounting for less than 1% of upper gastrointestinal bleeding cases. Given its frequently concealed nature, DDB poses significant diagnostic and therapeutic challenges. We report a rare case of DDB in a critically ill patient, outlining the diagnostic complexities and detailing endoscopic strategies employed for management.
Case Description/
Methods: A 68-year-old man with end-stage renal disease on hemodialysis, decompensated cirrhosis, heart failure with preserved ejection fraction, and a recent course of severe COVID-19 presented with melena and profound anemia (Hgb 4.6 g/dL). He arrived by ambulance from a long-term care facility where he had been receiving low-dose norepinephrine for refractory hypotension and was admitted to the ICU. Index esophagogastroduodenoscopy (EGD) revealed multiple duodenal angioectasias which were treated with argon plasma coagulation, and a duodenal diverticulum with an impacted fibrotic mucus plug in the posterior wall of the duodenal bulb. On hospital day 5, recurrent hematochezia necessitated repeat endoscopy, this time with visualization of active bleeding from the diverticulum. Attempts to dislodge the fibrous cap failed, but hemostasis was achieved by means of injection with 5 cc of 1:10,000 epinephrine within and around the diverticulum, subsequently a clip specialized in closure of mucosal defects was used to appose the mouth of the diverticulum with successful tamponade. The patient required a total of 11 units of packed red blood cells and was discharged to a long-term care facility after tracheostomy and feeding tube placement.
Discussion: This case highlights the diagnostic challenges associated with DDB, especially when the culprit vessel is masked by debris, or is located within an endoscopically inaccessible diverticulum. Adequate endoscopic hemostasis may require the use of multiple modalities, including hemoclip placement, epinephrine injection, or thermal cautery. If all other methods fail to identify and treat the source of bleeding, catheter angiography and embolization may be employed to achieve hemostasis. Prompt identification of and intervention against DDB is critical to minimize prolonged hospitalization, transfusion burden, and mortality. More case reports are needed to raise awareness of techniques shown to provide satisfactory hemostasis in complex cases of DDB.
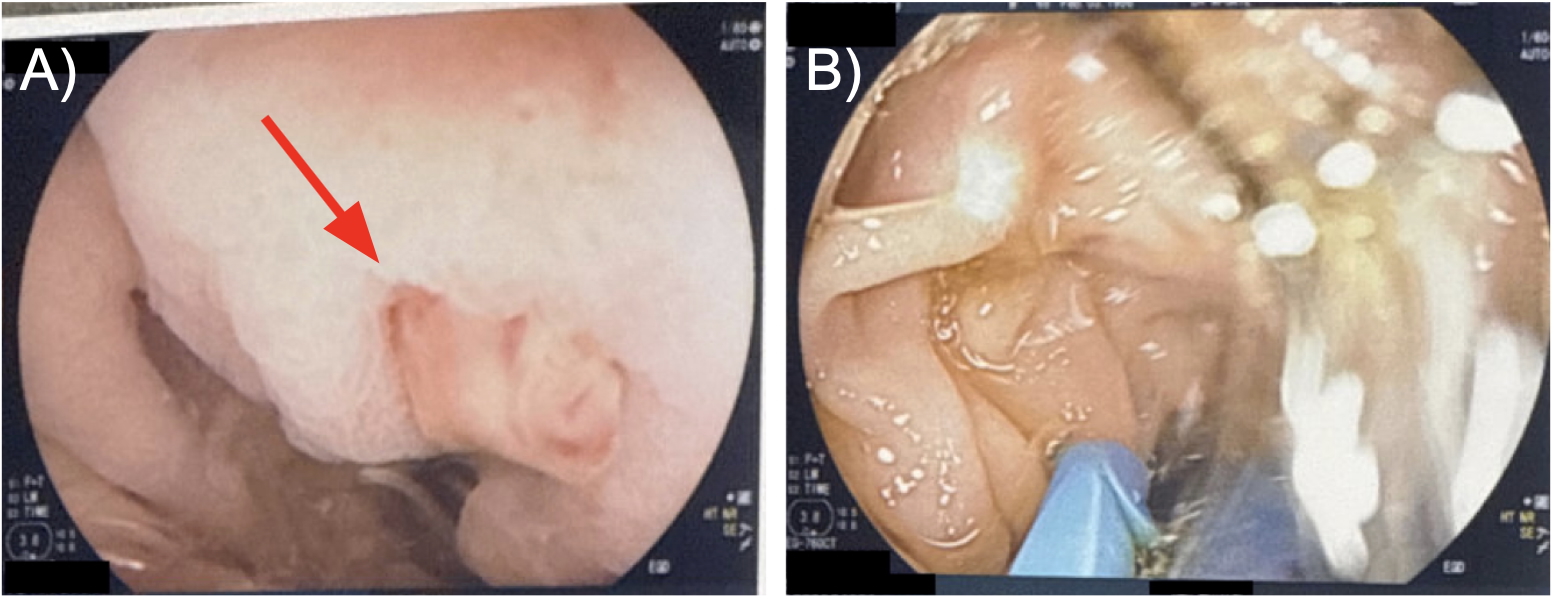
Figure: Figure 1. Findings from index EGD on hospital day 1. A) Fibrous cap (red arrow) noted obstructing view of the duodenal diverticulum. B) Attempt at mechanical dislodgment of fibrous cap from duodenal diverticulum.
Disclosures:
Mark Stasiewicz indicated no relevant financial relationships.
Kenneth Chow indicated no relevant financial relationships.
Amrit Narwan indicated no relevant financial relationships.
Jose Aponte-Pieras indicated no relevant financial relationships.
Mark Stasiewicz, MD1, Kenneth Chow, MD2, Amrit Narwan, MD1, Jose Aponte-Pieras, MD1. P3123 - A Rare Case of Duodenal Diverticular Bleeding: Challenges and Endoscopic Approach, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
