Monday Poster Session
Category: GI Bleeding
P3119 - A Rare and Complex Case of Acute Gastrointestinal Bleeding With an Elusive Source: Suspected Hemosuccus Pancreaticus
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Anjo Chacko, MD
Broward Health North
Coral Springs, FL
Presenting Author(s)
Anjo Chacko, MD1, Laura Miranda-Burgos, MD2, Harold Rosen, MD2
1Broward Health North, Coral Springs, FL; 2Broward Health North, Deerfield Beach, FL
Introduction: Hemosuccus pancreaticus is a rare, potentially life-threatening cause of upper GI bleeding characterized by hemorrhage into the pancreatic duct and drainage into the duodenum via the papilla of Vater. It often presents with intermittent, sometimes massive bleeding. Diagnosis is difficult due to its episodic nature and often unremarkable endoscopic findings unless performed during active hemorrhage. The most common etiology is rupture of a splenic artery pseudoaneurysm into the pancreatic duct, frequently associated with chronic pancreatitis.
Case Description/
Methods: We present the case of a 53-year-old female with chronic pancreatitis from alcohol use disorder, complicated by exocrine pancreatic insufficiency and chronic gastritis, who presented with two days of sharp left upper quadrant pain, nausea, and hematemesis following a seizure and fall. On evaluation, she was hemodynamically stable with epigastric and LUQ tenderness. Hemoglobin was 7.3 g/dL. CT angiography showed two splenic artery aneurysms: a 13×10 mm saccular aneurysm in the pancreatic body and a 9×9×13 mm fusiform aneurysm at the splenic hilum, along with an AAST Grade 3 splenic laceration and contained hematoma. Despite initial stability, she developed hemorrhagic shock requiring transfusion. Emergent IR-guided embolization of the ruptured pseudoaneurysm was performed. Post-embolization imaging confirmed bleeding cessation and splenic perfusion via pancreaticoduodenal arcade collaterals. EGD showed a 3 mm gastric ulcer with surrounding edema, managed with clipping, and several nonbleeding antral ulcers. The patient stabilized and had no further bleeding.
Discussion: This case highlights the diagnostic challenge of hemosuccus pancreaticus and underscores the importance of early cross-sectional imaging and angiographic intervention in suspected cases. Embolization is preferred for rapid control while preserving splenic function; surgery is reserved for refractory cases. Clinicians should maintain high suspicion in patients with chronic pancreatitis and obscure GI bleeding. Further research is needed to define diagnostic algorithms, identify predictive markers for aneurysm rupture, and compare long-term outcomes of endovascular versus surgical therapies.

Figure: Figure 1. Axial CT angiography of the abdomen image demonstrating two splenic artery aneurysms: a 13×10 mm saccular aneurysm within the pancreatic body and a 9×9×13 mm fusiform aneurysm at the splenic hilum, with a Grade 3 splenic laceration with a contained hematoma.
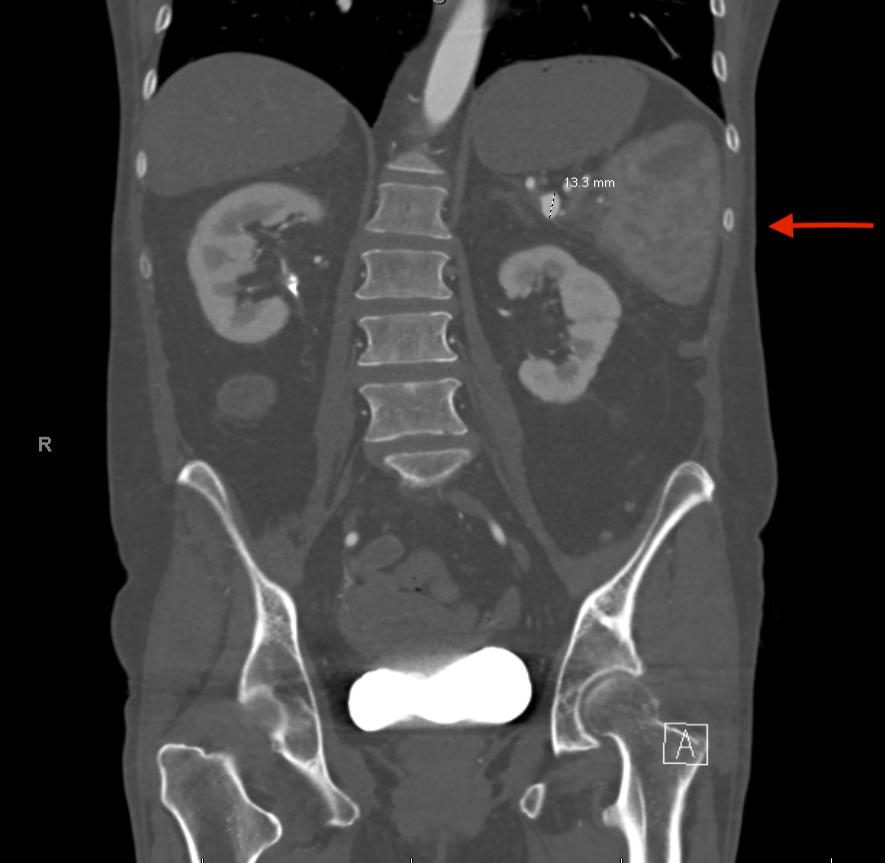
Figure: Figure 2. Coronal CT angiography abdomen image demonstrating a 13×10 mm saccular aneurysm within the pancreatic body.
Disclosures:
Anjo Chacko indicated no relevant financial relationships.
Laura Miranda-Burgos indicated no relevant financial relationships.
Harold Rosen indicated no relevant financial relationships.
Anjo Chacko, MD1, Laura Miranda-Burgos, MD2, Harold Rosen, MD2. P3119 - A Rare and Complex Case of Acute Gastrointestinal Bleeding With an Elusive Source: Suspected Hemosuccus Pancreaticus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Broward Health North, Coral Springs, FL; 2Broward Health North, Deerfield Beach, FL
Introduction: Hemosuccus pancreaticus is a rare, potentially life-threatening cause of upper GI bleeding characterized by hemorrhage into the pancreatic duct and drainage into the duodenum via the papilla of Vater. It often presents with intermittent, sometimes massive bleeding. Diagnosis is difficult due to its episodic nature and often unremarkable endoscopic findings unless performed during active hemorrhage. The most common etiology is rupture of a splenic artery pseudoaneurysm into the pancreatic duct, frequently associated with chronic pancreatitis.
Case Description/
Methods: We present the case of a 53-year-old female with chronic pancreatitis from alcohol use disorder, complicated by exocrine pancreatic insufficiency and chronic gastritis, who presented with two days of sharp left upper quadrant pain, nausea, and hematemesis following a seizure and fall. On evaluation, she was hemodynamically stable with epigastric and LUQ tenderness. Hemoglobin was 7.3 g/dL. CT angiography showed two splenic artery aneurysms: a 13×10 mm saccular aneurysm in the pancreatic body and a 9×9×13 mm fusiform aneurysm at the splenic hilum, along with an AAST Grade 3 splenic laceration and contained hematoma. Despite initial stability, she developed hemorrhagic shock requiring transfusion. Emergent IR-guided embolization of the ruptured pseudoaneurysm was performed. Post-embolization imaging confirmed bleeding cessation and splenic perfusion via pancreaticoduodenal arcade collaterals. EGD showed a 3 mm gastric ulcer with surrounding edema, managed with clipping, and several nonbleeding antral ulcers. The patient stabilized and had no further bleeding.
Discussion: This case highlights the diagnostic challenge of hemosuccus pancreaticus and underscores the importance of early cross-sectional imaging and angiographic intervention in suspected cases. Embolization is preferred for rapid control while preserving splenic function; surgery is reserved for refractory cases. Clinicians should maintain high suspicion in patients with chronic pancreatitis and obscure GI bleeding. Further research is needed to define diagnostic algorithms, identify predictive markers for aneurysm rupture, and compare long-term outcomes of endovascular versus surgical therapies.

Figure: Figure 1. Axial CT angiography of the abdomen image demonstrating two splenic artery aneurysms: a 13×10 mm saccular aneurysm within the pancreatic body and a 9×9×13 mm fusiform aneurysm at the splenic hilum, with a Grade 3 splenic laceration with a contained hematoma.
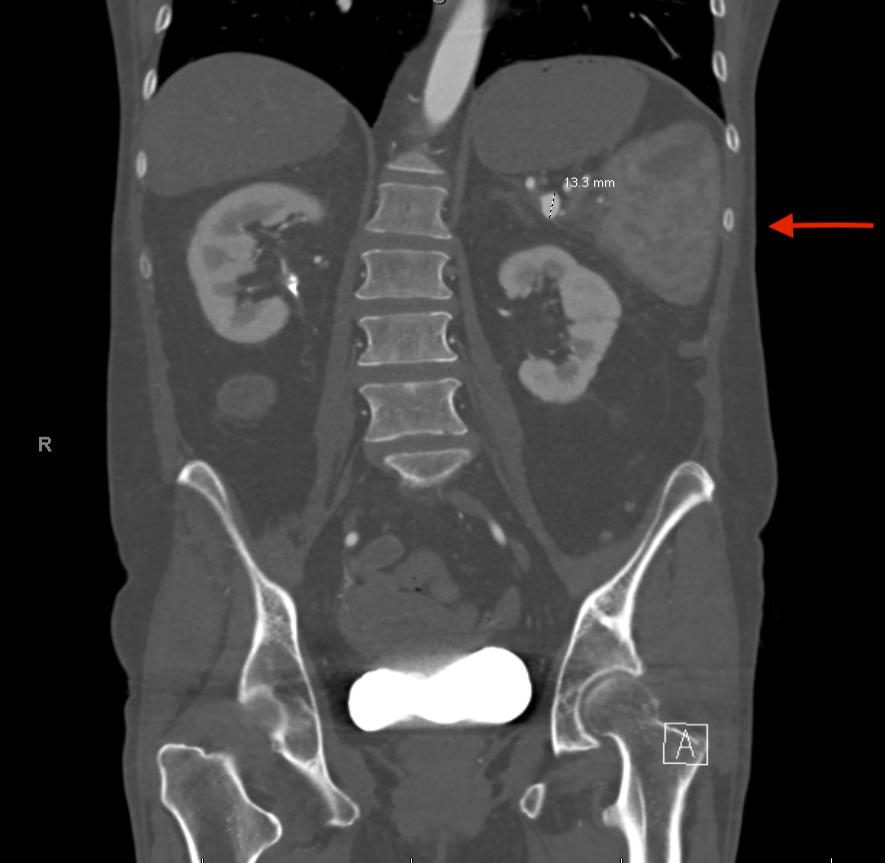
Figure: Figure 2. Coronal CT angiography abdomen image demonstrating a 13×10 mm saccular aneurysm within the pancreatic body.
Disclosures:
Anjo Chacko indicated no relevant financial relationships.
Laura Miranda-Burgos indicated no relevant financial relationships.
Harold Rosen indicated no relevant financial relationships.
Anjo Chacko, MD1, Laura Miranda-Burgos, MD2, Harold Rosen, MD2. P3119 - A Rare and Complex Case of Acute Gastrointestinal Bleeding With an Elusive Source: Suspected Hemosuccus Pancreaticus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
