Monday Poster Session
Category: GI Bleeding
P3118 - Aorto-Esophageal Fistula Secondary to Chronic Esophagitis: An Unusual Cause With a Rare Outcome
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- HK
Hamza I. Khan, MD
Lynda K. and David M. Underwood Center for Digestive Disorders, Houston Methodist Hospital
Houston, TX
Presenting Author(s)
Hamza I. Khan, MD, Frank Meriano, MD
Lynda K. and David M. Underwood Center for Digestive Disorders, Houston Methodist Hospital, Houston, TX
Introduction: Aorto-esophageal fistula (AEF) is a rare but often fatal cause of upper gastrointestinal bleeding, typically associated with thoracic aortic aneurysms or prior aortic interventions. Herein, we present a unique case of spontaneous AEF in a patient without known vascular disease who survived despite being a poor candidate for definitive surgical repair.
Case Description/
Methods: A 66-year-old female with hypertension and GERD initially presented with severe anemia (Hgb 2.9 g/dL), dysphagia, and weight loss. Esophagogastroduodenoscopy (EGD) revealed LA Grade C esophagitis, a diverticulum in the lower third of the esophagus (Image a), and gastric ulcers.
Seven years later, she re-presented at age 73 with hematemesis and syncope. Labs showed Hgb 6.1 g/dL. EGD demonstrated a spurting distal esophageal ulcer. Hemostasis was attempted with epinephrine and a single clip, but bleeding persisted. CT angiography confirmed AEF (Image b), and she underwent emergent thoracic endovascular aortic repair (TEVAR). Post-procedural EGD showed a defect in the esophageal wall (Image c).
The patient was stabilized in the ICU and managed conservatively with total parenteral nutrition (TPN) and prolonged IV antibiotics for a presumed infected aortic stent. She was ultimately discharged home.
Discussion: AEF is classically associated with thoracic aortic aneurysms or prior vascular surgery. Most patients present with a herald bleed followed by exsanguination. Diagnosis is challenging; EGD may miss the tract, while CT angiography is more sensitive.
This case is notable for both its etiology and outcome. The patient had no history of vascular disease or prior instrumentation. Chronic esophageal inflammation from longstanding esophagitis likely contributed to ulcer formation and subsequent fistulization—a mechanism rarely reported. While TEVAR is often used as a bridge to surgery, it provided durable hemostasis in this case.
Clinicians should maintain a high index of suspicion for AEF in patients with upper GI bleeding and esophageal pathology, even in the absence of classic vascular risk factors. Prompt recognition, early imaging, and a multidisciplinary approach remain essential to improving outcomes in this otherwise fatal condition.
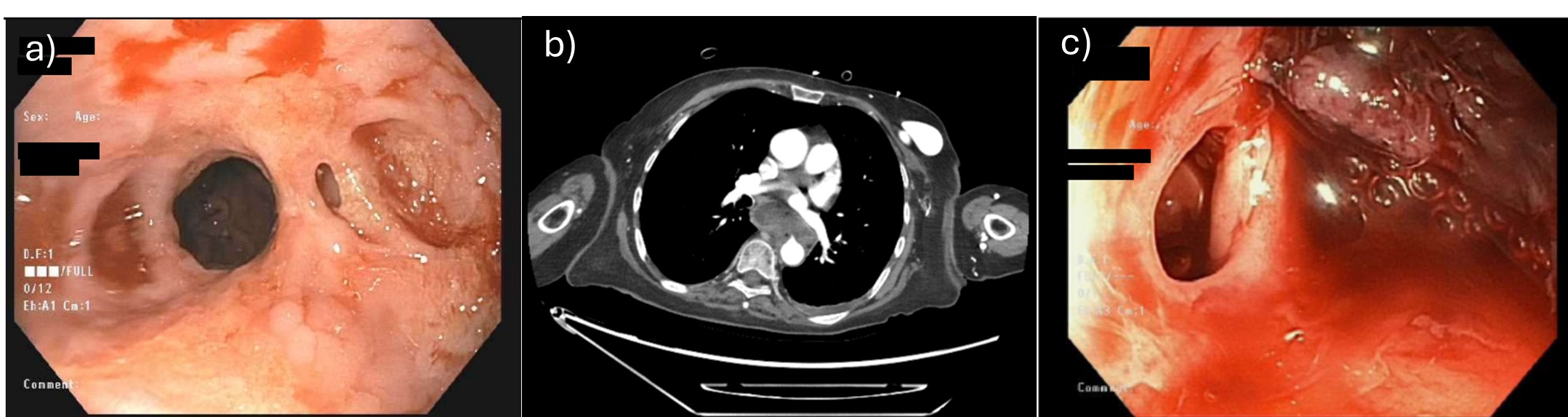
Figure: Image a: Esophgeal diverticulum on initial EGD. Image b: CT scan showing aortoesophageal fistula. Image c: Esophageal defect on EGD.
Disclosures:
Hamza Khan indicated no relevant financial relationships.
Frank Meriano indicated no relevant financial relationships.
Hamza I. Khan, MD, Frank Meriano, MD. P3118 - Aorto-Esophageal Fistula Secondary to Chronic Esophagitis: An Unusual Cause With a Rare Outcome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Lynda K. and David M. Underwood Center for Digestive Disorders, Houston Methodist Hospital, Houston, TX
Introduction: Aorto-esophageal fistula (AEF) is a rare but often fatal cause of upper gastrointestinal bleeding, typically associated with thoracic aortic aneurysms or prior aortic interventions. Herein, we present a unique case of spontaneous AEF in a patient without known vascular disease who survived despite being a poor candidate for definitive surgical repair.
Case Description/
Methods: A 66-year-old female with hypertension and GERD initially presented with severe anemia (Hgb 2.9 g/dL), dysphagia, and weight loss. Esophagogastroduodenoscopy (EGD) revealed LA Grade C esophagitis, a diverticulum in the lower third of the esophagus (Image a), and gastric ulcers.
Seven years later, she re-presented at age 73 with hematemesis and syncope. Labs showed Hgb 6.1 g/dL. EGD demonstrated a spurting distal esophageal ulcer. Hemostasis was attempted with epinephrine and a single clip, but bleeding persisted. CT angiography confirmed AEF (Image b), and she underwent emergent thoracic endovascular aortic repair (TEVAR). Post-procedural EGD showed a defect in the esophageal wall (Image c).
The patient was stabilized in the ICU and managed conservatively with total parenteral nutrition (TPN) and prolonged IV antibiotics for a presumed infected aortic stent. She was ultimately discharged home.
Discussion: AEF is classically associated with thoracic aortic aneurysms or prior vascular surgery. Most patients present with a herald bleed followed by exsanguination. Diagnosis is challenging; EGD may miss the tract, while CT angiography is more sensitive.
This case is notable for both its etiology and outcome. The patient had no history of vascular disease or prior instrumentation. Chronic esophageal inflammation from longstanding esophagitis likely contributed to ulcer formation and subsequent fistulization—a mechanism rarely reported. While TEVAR is often used as a bridge to surgery, it provided durable hemostasis in this case.
Clinicians should maintain a high index of suspicion for AEF in patients with upper GI bleeding and esophageal pathology, even in the absence of classic vascular risk factors. Prompt recognition, early imaging, and a multidisciplinary approach remain essential to improving outcomes in this otherwise fatal condition.
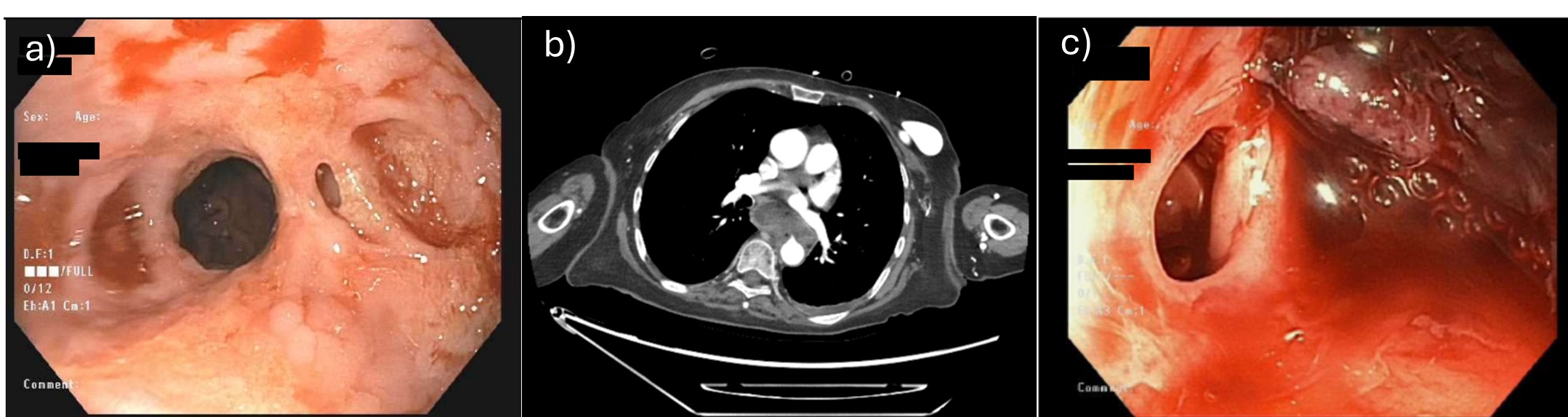
Figure: Image a: Esophgeal diverticulum on initial EGD. Image b: CT scan showing aortoesophageal fistula. Image c: Esophageal defect on EGD.
Disclosures:
Hamza Khan indicated no relevant financial relationships.
Frank Meriano indicated no relevant financial relationships.
Hamza I. Khan, MD, Frank Meriano, MD. P3118 - Aorto-Esophageal Fistula Secondary to Chronic Esophagitis: An Unusual Cause With a Rare Outcome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
