Monday Poster Session
Category: GI Bleeding
P3117 - Upper GI Bleed of Superior Pancreatoduodenal Artery Pseudoaneurysm in an Alcoholic Cirrhotic Patient: A Rare Complication
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Daniel Alejandro Gonzalez Mosquera, MD (he/him/his)
NYC Health + Hospitals/Lincoln
Bronx, NY
Presenting Author(s)
Daniel Alejandro. Gonzalez Mosquera, MD1, Sakina Paracha, MD2, Carla Evangelista, MD2
1NYC Health + Hospitals/Lincoln, Bronx, NY; 2New York Health + Hospitals | Lincoln–Weill Cornell Medical College Affiliate, New York, USA, Bronx, NY
Introduction: Bleeding from a pseudoaneurysm is a rare cause of upper gastrointestinal bleeding (UGIB), with visceral artery pseudoaneurysm (VAAP) occurring in 0.1% to 2% of adults. Pancreatoduodenal arteries account for 5% to 20% of these cases. Symptoms typically include abdominal pain, gastrointestinal hemorrhage, and jaundice. We present a case of a superior pancreatoduodenal artery pseudoaneurysm in a middle-aged adult.
Case Description/
Methods: A 40-year-old male with alcoholic cirrhosis, an indwelling peritoneal catheter for refractory ascites, and end-stage renal disease on thrice-weekly hemodialysis presented from dialysis with severe asymptomatic anemia. He denied prior GI bleeding, reporting only a recent epistaxis. On exam, he had jaundice and bilateral lower extremity edema. Labs showed hemoglobin 5.0 g/dL (baseline 8.3), platelets 54K/µL, creatinine 6.82 mg/dL, PT 26.3 sec, INR 2.3, total bilirubin 10.3 mg/dL, and direct bilirubin 6.6 mg/dL. Two units of PRBCs were transfused.
Chest X-ray revealed massive hepatic hydrothorax, requiring pigtail catheter placement. On hospital day 4, he developed septic shock, likely due to intra-abdominal infection, requiring vasopressors (norepinephrine, later midodrine) and antibiotics.
At day 19th, presented a right and left upper quadrant pain with tenderness. On his 20th day of hospitalization, melena presented which increased his pressors requirements. His hemoglobin dropped from 7.7 g/dL to 6.1 g/dL, requiring another unit of PRBC. A CT Angiogram identified an 18 mm pseudoaneurysm of the superior pancreatoduodenal artery. Interventional radiology performed visceral artery coil embolization of the gastroduodenal and pancreatoduodenal arteries.
Despite intervention, the patient’s melena persisted. Dialysis became intolerable, and hepatic encephalopathy developed. A multidisciplinary team discussed goals-of-care discussion, the patient was transitioned to comfort measures and expired on day 23.
Discussion: VAAPs, though rare, carry high mortality, especially if ruptured, causing intra- or retroperitoneal bleeding and shock. Mortality exceeds 50%, and untreated cases approach 100%. Prompt diagnosis is critical. Endovascular coil embolization is the preferred treatment with >93% success. Surgical, percutaneous, or endoscopic options may be considered in refractory cases. In conclusion, superior pancreatoduodenal pseudoaneurysm is a rare but critical cause of UGIB. Prompt diagnosis and early intervention are vital to improving outcomes and reducing mortality.
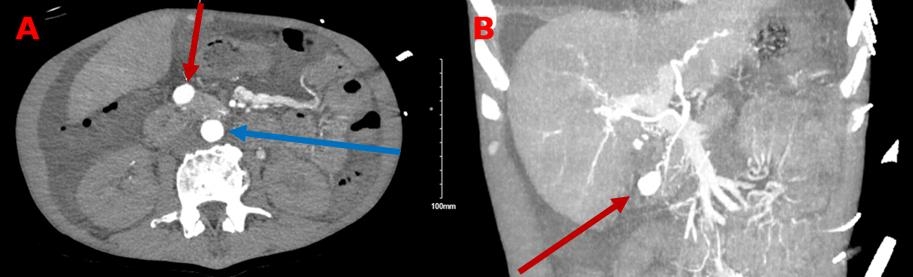
Figure: CT Scan of Abdomen with contrast. Figure 1A: Axial view of the pancreatoduodenal artery pseudoaneurysm (Red arrow) and the abdominal aorta (Blue arrow). Figure 1B: Sagital view, which shows abdomen vasculature and the pseudoaneurysm (Red arrow).
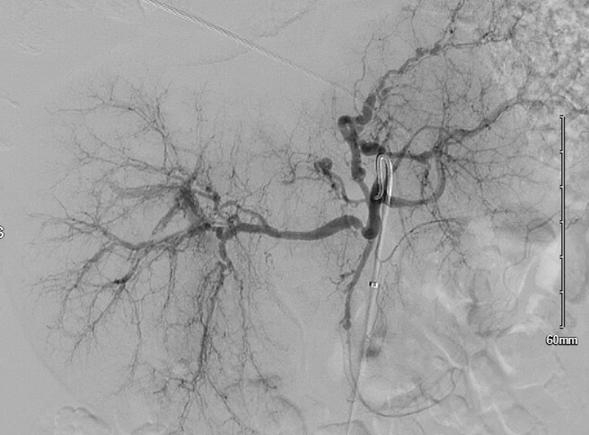
Figure: Angiogram post superselective coil embolization of the gastroduodenal and pancreatoduodenal arteries.
Disclosures:
Daniel Gonzalez Mosquera indicated no relevant financial relationships.
Sakina Paracha indicated no relevant financial relationships.
Carla Evangelista indicated no relevant financial relationships.
Daniel Alejandro. Gonzalez Mosquera, MD1, Sakina Paracha, MD2, Carla Evangelista, MD2. P3117 - Upper GI Bleed of Superior Pancreatoduodenal Artery Pseudoaneurysm in an Alcoholic Cirrhotic Patient: A Rare Complication, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NYC Health + Hospitals/Lincoln, Bronx, NY; 2New York Health + Hospitals | Lincoln–Weill Cornell Medical College Affiliate, New York, USA, Bronx, NY
Introduction: Bleeding from a pseudoaneurysm is a rare cause of upper gastrointestinal bleeding (UGIB), with visceral artery pseudoaneurysm (VAAP) occurring in 0.1% to 2% of adults. Pancreatoduodenal arteries account for 5% to 20% of these cases. Symptoms typically include abdominal pain, gastrointestinal hemorrhage, and jaundice. We present a case of a superior pancreatoduodenal artery pseudoaneurysm in a middle-aged adult.
Case Description/
Methods: A 40-year-old male with alcoholic cirrhosis, an indwelling peritoneal catheter for refractory ascites, and end-stage renal disease on thrice-weekly hemodialysis presented from dialysis with severe asymptomatic anemia. He denied prior GI bleeding, reporting only a recent epistaxis. On exam, he had jaundice and bilateral lower extremity edema. Labs showed hemoglobin 5.0 g/dL (baseline 8.3), platelets 54K/µL, creatinine 6.82 mg/dL, PT 26.3 sec, INR 2.3, total bilirubin 10.3 mg/dL, and direct bilirubin 6.6 mg/dL. Two units of PRBCs were transfused.
Chest X-ray revealed massive hepatic hydrothorax, requiring pigtail catheter placement. On hospital day 4, he developed septic shock, likely due to intra-abdominal infection, requiring vasopressors (norepinephrine, later midodrine) and antibiotics.
At day 19th, presented a right and left upper quadrant pain with tenderness. On his 20th day of hospitalization, melena presented which increased his pressors requirements. His hemoglobin dropped from 7.7 g/dL to 6.1 g/dL, requiring another unit of PRBC. A CT Angiogram identified an 18 mm pseudoaneurysm of the superior pancreatoduodenal artery. Interventional radiology performed visceral artery coil embolization of the gastroduodenal and pancreatoduodenal arteries.
Despite intervention, the patient’s melena persisted. Dialysis became intolerable, and hepatic encephalopathy developed. A multidisciplinary team discussed goals-of-care discussion, the patient was transitioned to comfort measures and expired on day 23.
Discussion: VAAPs, though rare, carry high mortality, especially if ruptured, causing intra- or retroperitoneal bleeding and shock. Mortality exceeds 50%, and untreated cases approach 100%. Prompt diagnosis is critical. Endovascular coil embolization is the preferred treatment with >93% success. Surgical, percutaneous, or endoscopic options may be considered in refractory cases. In conclusion, superior pancreatoduodenal pseudoaneurysm is a rare but critical cause of UGIB. Prompt diagnosis and early intervention are vital to improving outcomes and reducing mortality.
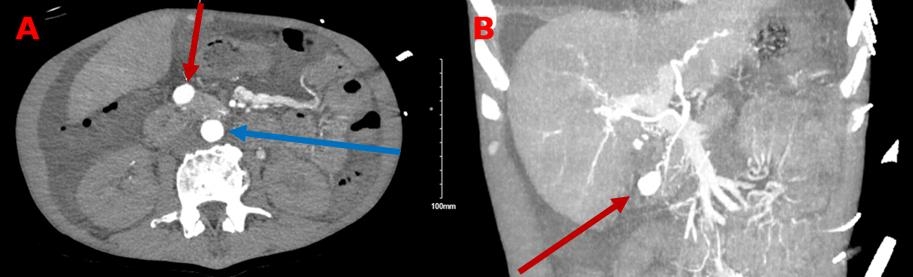
Figure: CT Scan of Abdomen with contrast. Figure 1A: Axial view of the pancreatoduodenal artery pseudoaneurysm (Red arrow) and the abdominal aorta (Blue arrow). Figure 1B: Sagital view, which shows abdomen vasculature and the pseudoaneurysm (Red arrow).
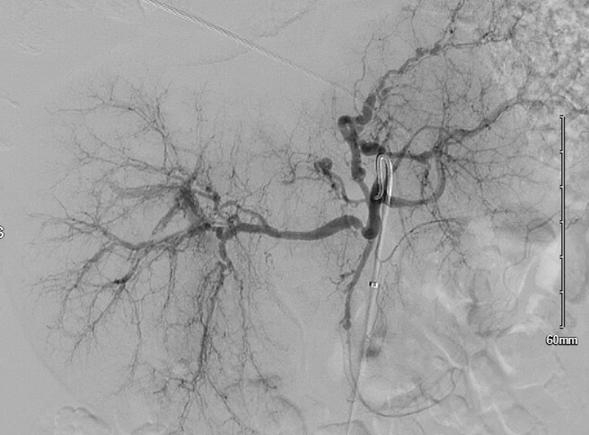
Figure: Angiogram post superselective coil embolization of the gastroduodenal and pancreatoduodenal arteries.
Disclosures:
Daniel Gonzalez Mosquera indicated no relevant financial relationships.
Sakina Paracha indicated no relevant financial relationships.
Carla Evangelista indicated no relevant financial relationships.
Daniel Alejandro. Gonzalez Mosquera, MD1, Sakina Paracha, MD2, Carla Evangelista, MD2. P3117 - Upper GI Bleed of Superior Pancreatoduodenal Artery Pseudoaneurysm in an Alcoholic Cirrhotic Patient: A Rare Complication, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
