Monday Poster Session
Category: IBD
P3213 - Enhancing Fecal Calprotectin Utilization for IBD Management in Veterans: A Quality Improvement Initiative at the G.V. (Sonny) Montgomery VA Medical Center
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- NP
Namrata Paladugu, MD (she/her/hers)
University of Mississippi Medical Center
Jackson, MS
Presenting Author(s)
Namrata Paladugu, MD1, Christopher G. Moody, DO2, Aneeq Muhammad Yousuf, MD1, Kaitlyn Cronk, MD1, Jeremy Morgan, MD1, Elizabeth Paine, MD3
1University of Mississippi Medical Center, Jackson, MS; 2University of Mississippi Medical Center - - Jackson, MS, Brandon, MS; 3G.V. (Sonny) Montgomery VA Medical Center; University of Mississippi Medical Center, Jackson, MS
Introduction: Fecal calprotectin (FC), a protein secreted from inflamed intestinal mucosa, is a valuable biomarker for monitoring disease activity in patients with inflammatory bowel disease (IBD). At the G.V (Sonny) Montgomery VA Medical Center, there was difficulty with obtaining baseline FC levels. Veterans were required to turn in a paper miscellaneous lab slip with their stool sample, but often, the sample did not get submitted or the lab slip was lost. We hypothesized that if we gave patients the slip while they were in the infusion clinic receiving their biologic infusions, they were more likely to collect the sample and take it and the slip to the lab while still in the VA, thereby establishing baseline FC levels for these patients.
Methods: An intervention was implemented wherein veterans receiving biologic infusions between April 1 and June 30, 2023 (Mid 2023), were given FC lab slips during their infusion appointments and instructed to submit stool samples. This approach aimed to capitalize on the patients’ presence at the facility to hopefully enhance compliance and utilization of the FC lab. Veterans who received infusions between January 1 and March 31, 2023 (Early 2023) were identified to see how many had a baseline fecal calprotectin level. A retrospective chart review was done to compare the rates of baseline FC testing before and after the intervention (Figure 1).
Results: In the Early 2023 group, only 3.45% had baseline FC levels recorded. Post-intervention, in the Mid 2023 group, this rate surged to 83.33%, marking a significant increase of 79.88% (p< 1.001) (Figure 2).
Discussion: We provided patients with a lab slip at the time of biologic infusion to establish baseline FC levels in veterans with IBD. Notably, 40% of patients with established baseline FC levels during Mid 2023 had subsequent admissions for IBD. Having baseline data during remission proved valuable in assessing for disease flares. As utilization of the FC lab dramatically increased during the intervention, the VA Medical Center incorporated FC testing into the Gastroenterology order set, facilitating easier access during symptom recurrence. Guidelines have included normalization of inflammatory markers such as FC as a treatment goal in management of IBD. Moving forward, baseline fecal calprotectin levels should be established for all patients with biopsy proven IBD to provide additional data when making treatment decisions.
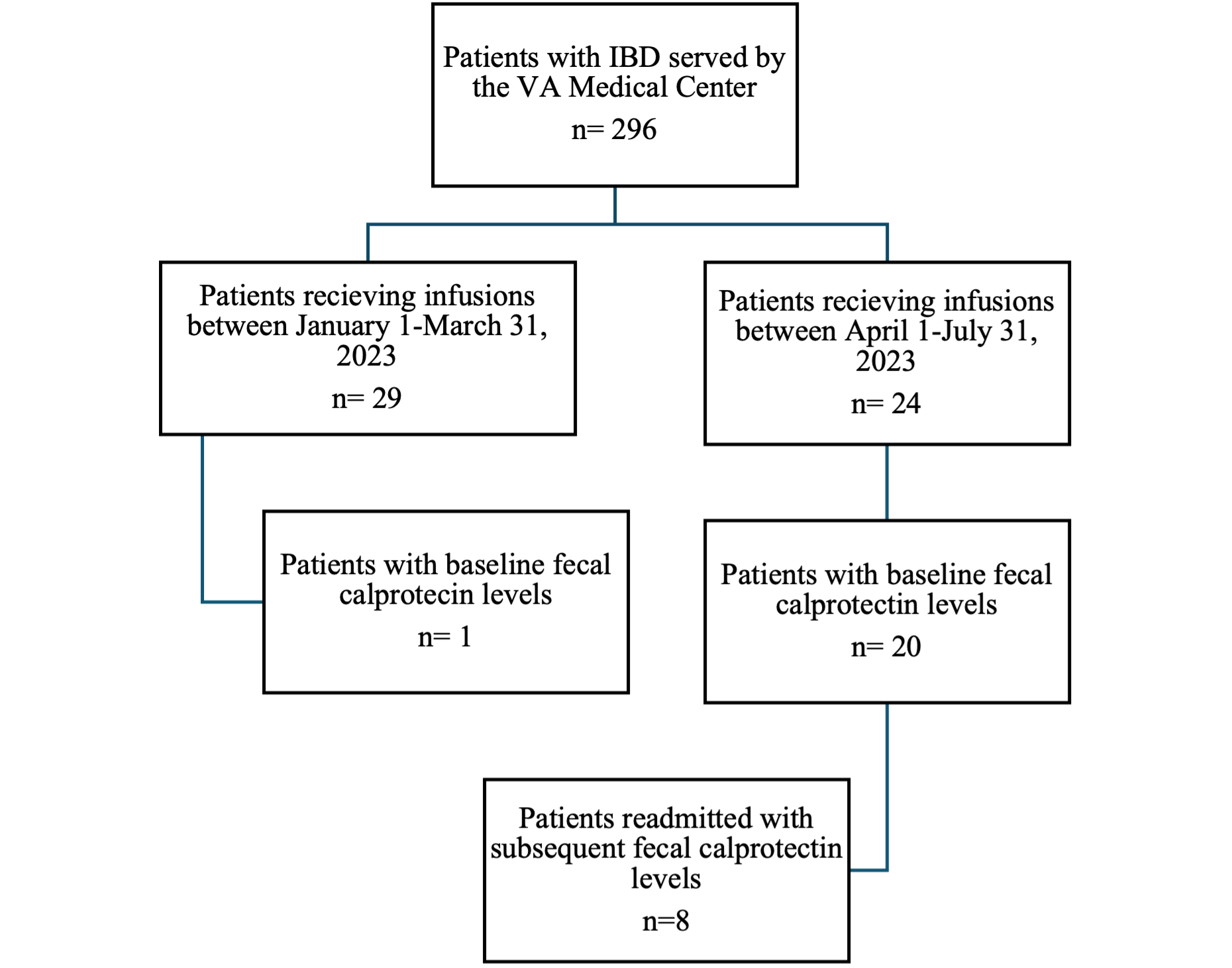
Figure: Figure 1. Diagram of patients included in the study
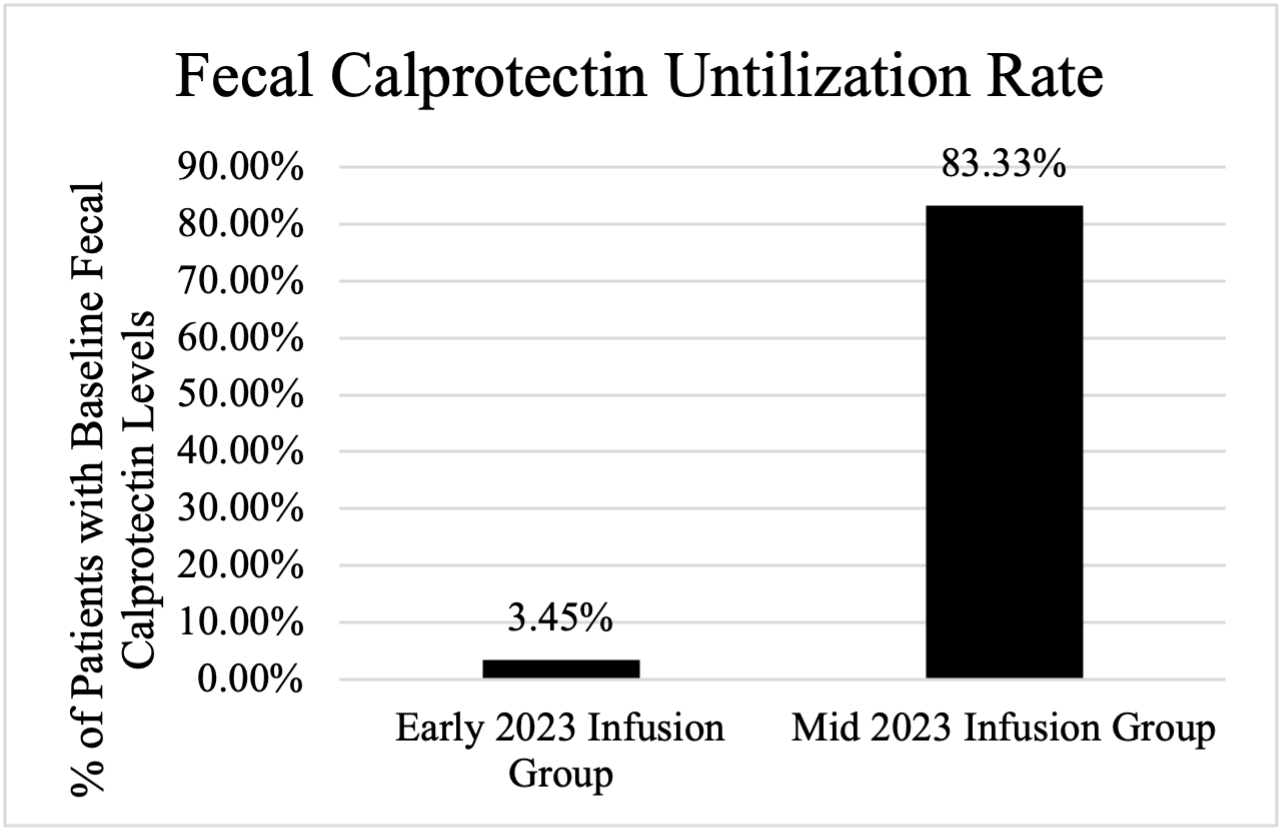
Figure: Figure 2. The utilization rate of fecal calprotectin labs, demonstrating a 79.88% increase in the utilization of FC after the intervention
Disclosures:
Namrata Paladugu indicated no relevant financial relationships.
Christopher Moody indicated no relevant financial relationships.
Aneeq Muhammad Yousuf indicated no relevant financial relationships.
Kaitlyn Cronk indicated no relevant financial relationships.
Jeremy Morgan indicated no relevant financial relationships.
Elizabeth Paine indicated no relevant financial relationships.
Namrata Paladugu, MD1, Christopher G. Moody, DO2, Aneeq Muhammad Yousuf, MD1, Kaitlyn Cronk, MD1, Jeremy Morgan, MD1, Elizabeth Paine, MD3. P3213 - Enhancing Fecal Calprotectin Utilization for IBD Management in Veterans: A Quality Improvement Initiative at the G.V. (Sonny) Montgomery VA Medical Center, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Mississippi Medical Center, Jackson, MS; 2University of Mississippi Medical Center - - Jackson, MS, Brandon, MS; 3G.V. (Sonny) Montgomery VA Medical Center; University of Mississippi Medical Center, Jackson, MS
Introduction: Fecal calprotectin (FC), a protein secreted from inflamed intestinal mucosa, is a valuable biomarker for monitoring disease activity in patients with inflammatory bowel disease (IBD). At the G.V (Sonny) Montgomery VA Medical Center, there was difficulty with obtaining baseline FC levels. Veterans were required to turn in a paper miscellaneous lab slip with their stool sample, but often, the sample did not get submitted or the lab slip was lost. We hypothesized that if we gave patients the slip while they were in the infusion clinic receiving their biologic infusions, they were more likely to collect the sample and take it and the slip to the lab while still in the VA, thereby establishing baseline FC levels for these patients.
Methods: An intervention was implemented wherein veterans receiving biologic infusions between April 1 and June 30, 2023 (Mid 2023), were given FC lab slips during their infusion appointments and instructed to submit stool samples. This approach aimed to capitalize on the patients’ presence at the facility to hopefully enhance compliance and utilization of the FC lab. Veterans who received infusions between January 1 and March 31, 2023 (Early 2023) were identified to see how many had a baseline fecal calprotectin level. A retrospective chart review was done to compare the rates of baseline FC testing before and after the intervention (Figure 1).
Results: In the Early 2023 group, only 3.45% had baseline FC levels recorded. Post-intervention, in the Mid 2023 group, this rate surged to 83.33%, marking a significant increase of 79.88% (p< 1.001) (Figure 2).
Discussion: We provided patients with a lab slip at the time of biologic infusion to establish baseline FC levels in veterans with IBD. Notably, 40% of patients with established baseline FC levels during Mid 2023 had subsequent admissions for IBD. Having baseline data during remission proved valuable in assessing for disease flares. As utilization of the FC lab dramatically increased during the intervention, the VA Medical Center incorporated FC testing into the Gastroenterology order set, facilitating easier access during symptom recurrence. Guidelines have included normalization of inflammatory markers such as FC as a treatment goal in management of IBD. Moving forward, baseline fecal calprotectin levels should be established for all patients with biopsy proven IBD to provide additional data when making treatment decisions.
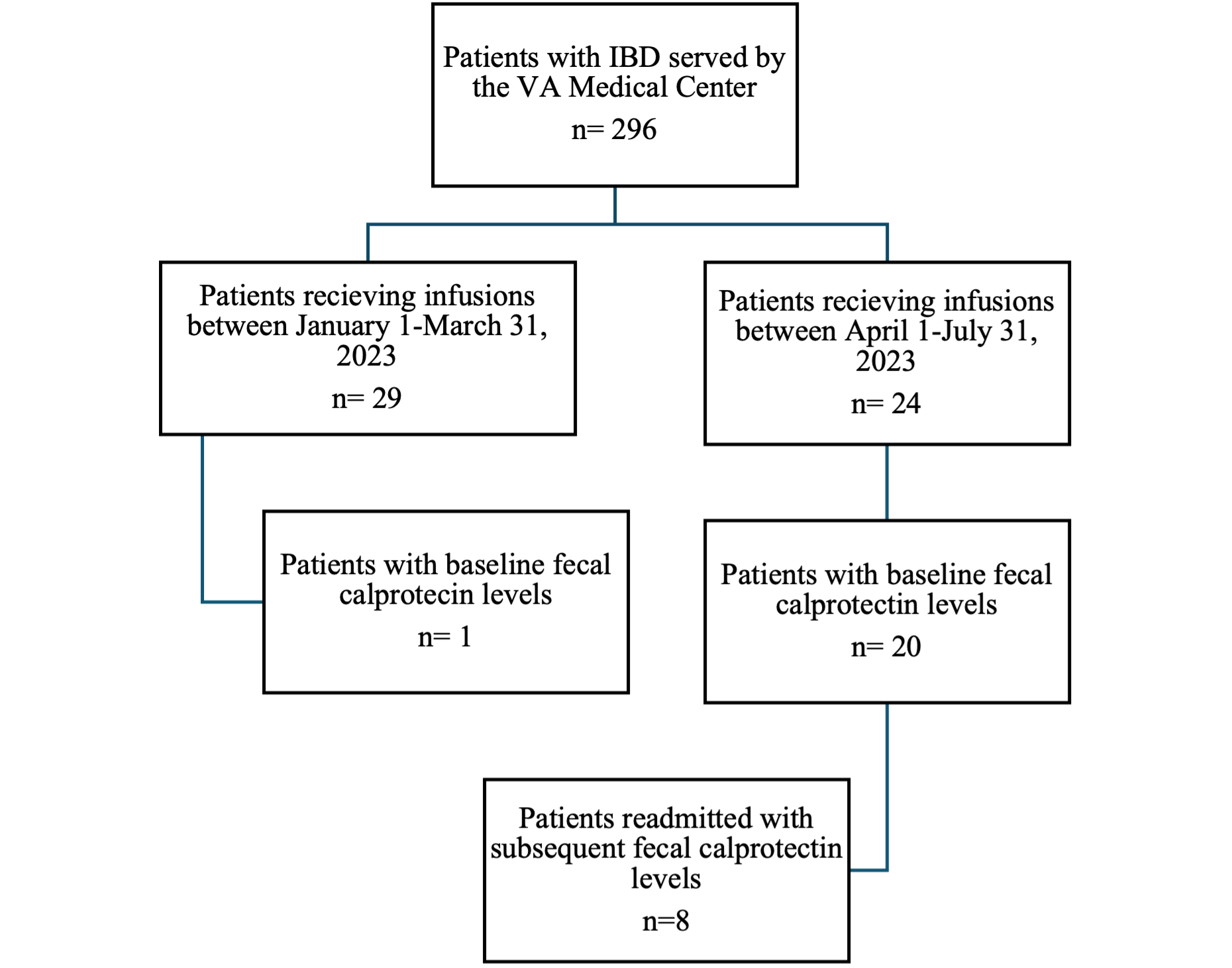
Figure: Figure 1. Diagram of patients included in the study
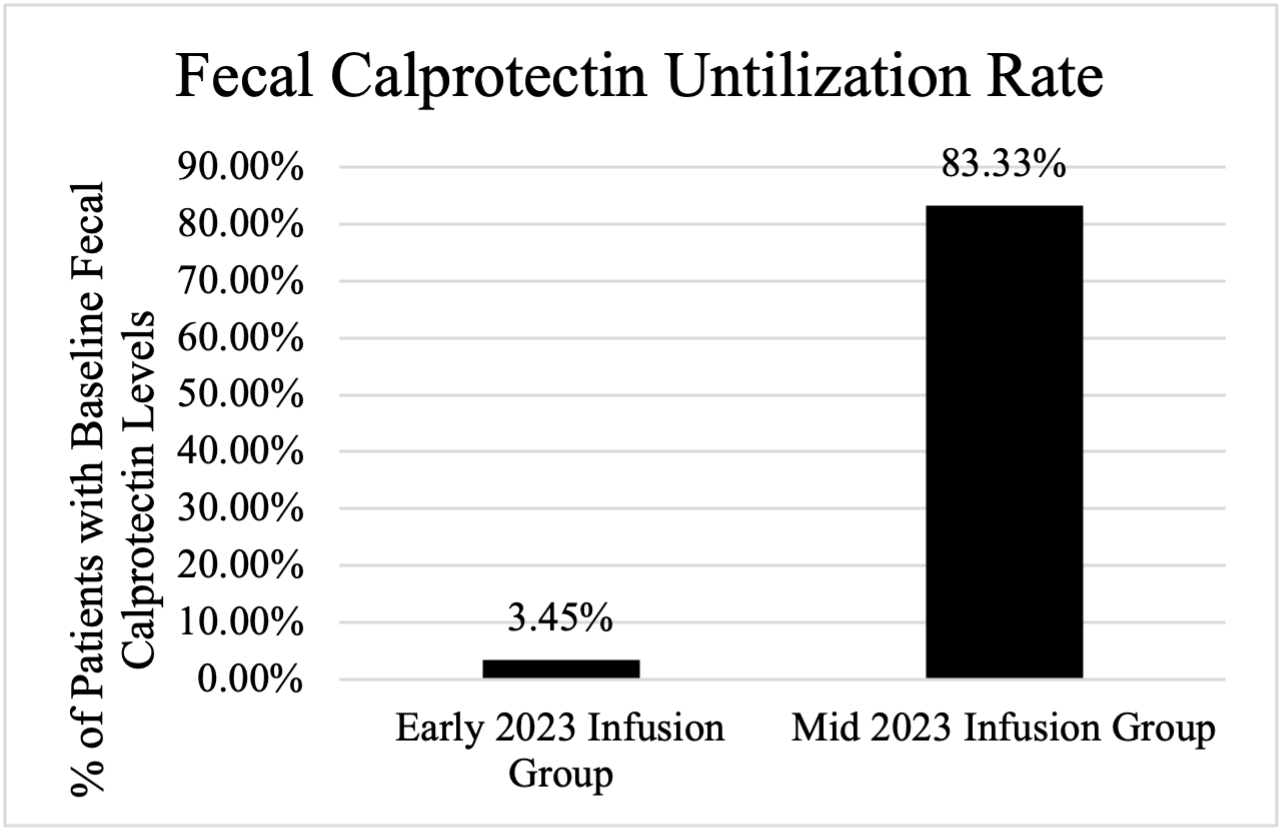
Figure: Figure 2. The utilization rate of fecal calprotectin labs, demonstrating a 79.88% increase in the utilization of FC after the intervention
Disclosures:
Namrata Paladugu indicated no relevant financial relationships.
Christopher Moody indicated no relevant financial relationships.
Aneeq Muhammad Yousuf indicated no relevant financial relationships.
Kaitlyn Cronk indicated no relevant financial relationships.
Jeremy Morgan indicated no relevant financial relationships.
Elizabeth Paine indicated no relevant financial relationships.
Namrata Paladugu, MD1, Christopher G. Moody, DO2, Aneeq Muhammad Yousuf, MD1, Kaitlyn Cronk, MD1, Jeremy Morgan, MD1, Elizabeth Paine, MD3. P3213 - Enhancing Fecal Calprotectin Utilization for IBD Management in Veterans: A Quality Improvement Initiative at the G.V. (Sonny) Montgomery VA Medical Center, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
