Monday Poster Session
Category: IBD
P3206 - Endoscopic Balloon Dilation of Inflammatory Crohn’s Disease Strictures Is Safe and Effective: A Retrospective Case Control Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Solomon Sasson, MD
University of British Columbia
Vancouver, BC, Canada
Presenting Author(s)
Solomon Sasson, MD1, David Di Fonzo, MD1, Itay Kalisky, MD1, Adedamola Bello, MD2, Sundeep Singh, MD3, Gregory Rosenfeld, MD, MHSc4
1University of British Columbia, Vancouver, BC, Canada; 2University of Saskatchewan, Saskatoon, SK, Canada; 3UBC Department of Medicine, Vancouver, BC, Canada; 4UBC Department of Medicine/IBD Centre of BC, Vancouver, BC, Canada
Introduction: Crohn’s disease (CD) is a chronic inflammatory condition often of a progressive nature. It can lead to strictures, which can be inflammatory, fibrostenotic, or a combination both. For short intestinal strictures, endoscopic balloon dilation (EBD) offers a less invasive alternative to surgical resection or stricturoplasty. However, concern remains amongst endoscopists around performing EBD in intestinal inflammatory strictures due to risk of perforation. We evaluated the efficacy and complication rates of endoscopic balloon dilation performed in Crohn’s disease strictures, with emphasis on ulcerated strictures.
Methods: We conducted a retrospective cohort study of CD patients undergoing EBD at large hospital centers in Vancouver, BC, Canada. Data were extracted on demographics, age at CD diagnosis, smoking status, medication use, ulceration status at the stricture site, anastomotic strictures, and fluoroscopy use. Complications, all-cause hospitalizations within 30 days, and need for surgery were recorded. Descriptive statistics summarized demographics and procedure characteristics. Fisher’s exact test assessed the association between ulceration status and adverse events. Logistic regression modeling could not be performed due to low event counts.
Results: A total of 377 balloon dilations were performed on 74 CD patients (44 males, 30 females), with an average of 5.1 dilations per patient. Each procedure achieved an average stricture dilation of 3 mm. Ulcerations at the stricture site were documented in 80 procedures, and anastomotic strictures were noted in 133 procedures. Eight complications (2.1%) occurred, including post-procedural bleeding (n=5), postprocedural abscess (n=1), mucosal trauma (n=1), and perforation (n=1). All-cause 30-day hospitalization occurred in 21 patients (5.6%). Twenty-two patients (29.7%) required surgery. Ulceration at the stricture site was not a significant predictor of adverse events (OR 1.61, 95% CI 0.66–3.91, p=0.36).
Discussion: EBD is a safe and effective therapy for CD strictures. Despite theoretical concerns, ulceration at the stricture site did not significantly increase complications or postprocedural hospitalizations. Overall complication rates were low. Nearly one-third of patients ultimately required surgery, underscoring the progressive nature of Crohn’s Disease, thereby highlighting appropriate treatment at an earlier stage of the disease.
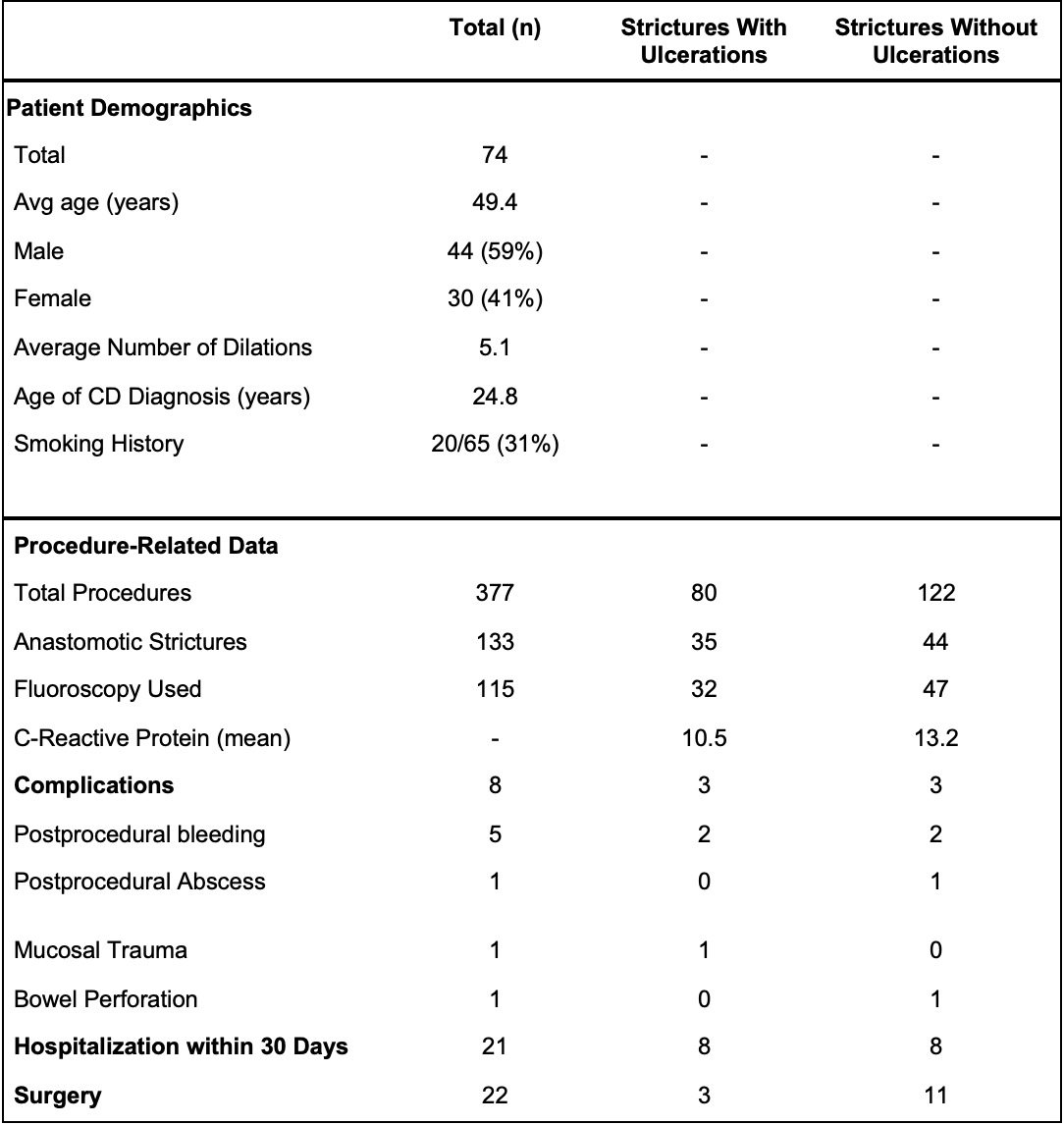
Figure: Patient Demographics and Procedure-Related Data Stratified by Ulceration Status
Disclosures:
Solomon Sasson indicated no relevant financial relationships.
David Di Fonzo indicated no relevant financial relationships.
Itay Kalisky indicated no relevant financial relationships.
Adedamola Bello indicated no relevant financial relationships.
Sundeep Singh indicated no relevant financial relationships.
Gregory Rosenfeld indicated no relevant financial relationships.
Solomon Sasson, MD1, David Di Fonzo, MD1, Itay Kalisky, MD1, Adedamola Bello, MD2, Sundeep Singh, MD3, Gregory Rosenfeld, MD, MHSc4. P3206 - Endoscopic Balloon Dilation of Inflammatory Crohn’s Disease Strictures Is Safe and Effective: A Retrospective Case Control Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of British Columbia, Vancouver, BC, Canada; 2University of Saskatchewan, Saskatoon, SK, Canada; 3UBC Department of Medicine, Vancouver, BC, Canada; 4UBC Department of Medicine/IBD Centre of BC, Vancouver, BC, Canada
Introduction: Crohn’s disease (CD) is a chronic inflammatory condition often of a progressive nature. It can lead to strictures, which can be inflammatory, fibrostenotic, or a combination both. For short intestinal strictures, endoscopic balloon dilation (EBD) offers a less invasive alternative to surgical resection or stricturoplasty. However, concern remains amongst endoscopists around performing EBD in intestinal inflammatory strictures due to risk of perforation. We evaluated the efficacy and complication rates of endoscopic balloon dilation performed in Crohn’s disease strictures, with emphasis on ulcerated strictures.
Methods: We conducted a retrospective cohort study of CD patients undergoing EBD at large hospital centers in Vancouver, BC, Canada. Data were extracted on demographics, age at CD diagnosis, smoking status, medication use, ulceration status at the stricture site, anastomotic strictures, and fluoroscopy use. Complications, all-cause hospitalizations within 30 days, and need for surgery were recorded. Descriptive statistics summarized demographics and procedure characteristics. Fisher’s exact test assessed the association between ulceration status and adverse events. Logistic regression modeling could not be performed due to low event counts.
Results: A total of 377 balloon dilations were performed on 74 CD patients (44 males, 30 females), with an average of 5.1 dilations per patient. Each procedure achieved an average stricture dilation of 3 mm. Ulcerations at the stricture site were documented in 80 procedures, and anastomotic strictures were noted in 133 procedures. Eight complications (2.1%) occurred, including post-procedural bleeding (n=5), postprocedural abscess (n=1), mucosal trauma (n=1), and perforation (n=1). All-cause 30-day hospitalization occurred in 21 patients (5.6%). Twenty-two patients (29.7%) required surgery. Ulceration at the stricture site was not a significant predictor of adverse events (OR 1.61, 95% CI 0.66–3.91, p=0.36).
Discussion: EBD is a safe and effective therapy for CD strictures. Despite theoretical concerns, ulceration at the stricture site did not significantly increase complications or postprocedural hospitalizations. Overall complication rates were low. Nearly one-third of patients ultimately required surgery, underscoring the progressive nature of Crohn’s Disease, thereby highlighting appropriate treatment at an earlier stage of the disease.
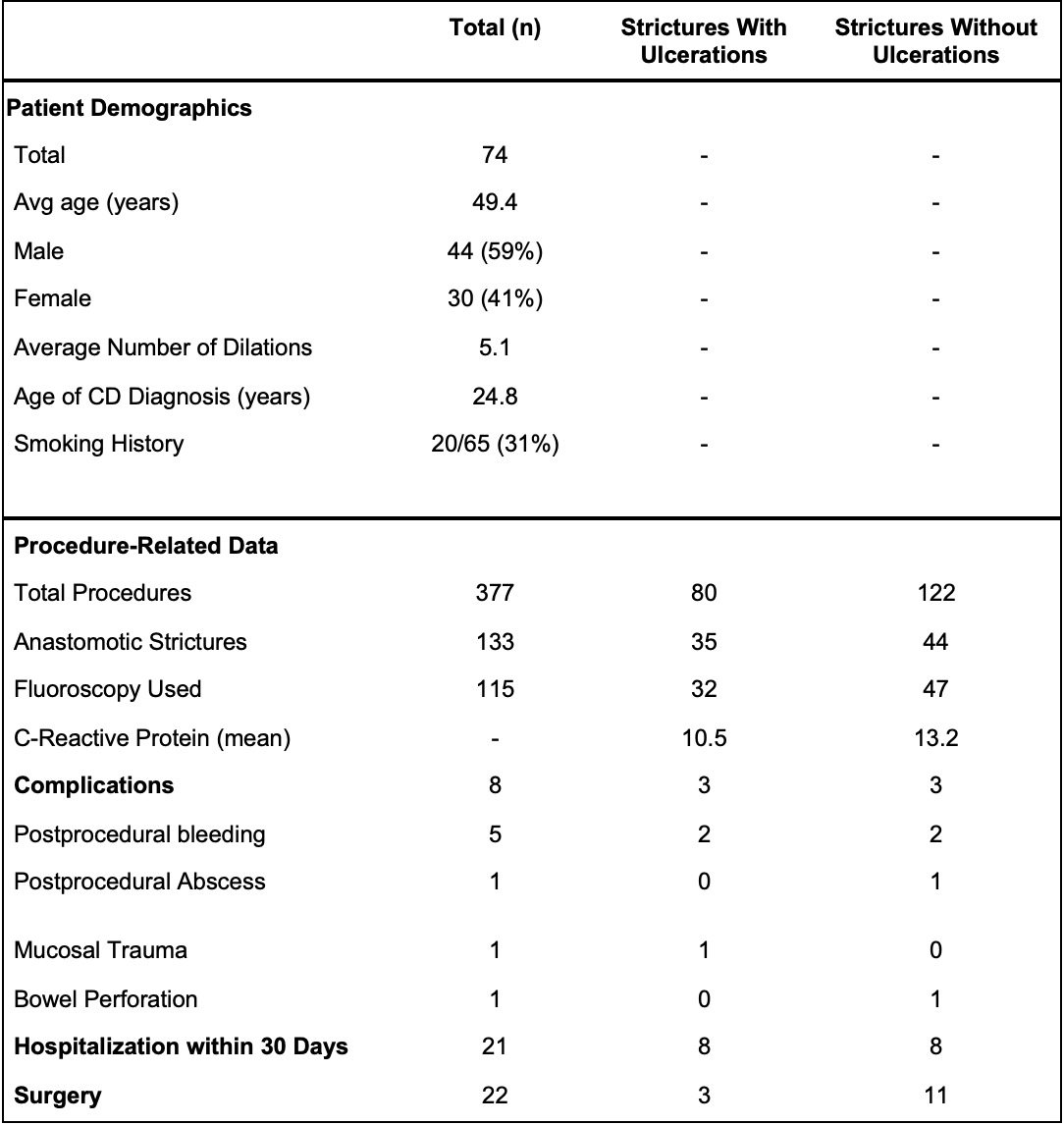
Figure: Patient Demographics and Procedure-Related Data Stratified by Ulceration Status
Disclosures:
Solomon Sasson indicated no relevant financial relationships.
David Di Fonzo indicated no relevant financial relationships.
Itay Kalisky indicated no relevant financial relationships.
Adedamola Bello indicated no relevant financial relationships.
Sundeep Singh indicated no relevant financial relationships.
Gregory Rosenfeld indicated no relevant financial relationships.
Solomon Sasson, MD1, David Di Fonzo, MD1, Itay Kalisky, MD1, Adedamola Bello, MD2, Sundeep Singh, MD3, Gregory Rosenfeld, MD, MHSc4. P3206 - Endoscopic Balloon Dilation of Inflammatory Crohn’s Disease Strictures Is Safe and Effective: A Retrospective Case Control Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
