Monday Poster Session
Category: IBD
P3204 - Is IBD a Predictor of Poor Outcomes in Acute Mesenteric Ischemia?
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- UB
Umesh Bhagat, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Umesh Bhagat, MD1, Ankit Agrawal, 2, Archana Kharel, MD2, Shalini Tripathi, MD2, Mohamed Abdelbaky, MD3, Archit Garg, MD4, Sukul Khanna, MBBS5, Prabhat Kumar, MD6, Luisa Recinos, MD7
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic, Cleveland, OH; 3Presbyterian Health care, Albuquerque, NM; 4Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 5University College of Medical Sciences and Guru Teg Bahadur Hospital, New Delhi, Delhi, India; 6Virginia Commonwealth University, Richmond, VA; 7Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, Somerset, NJ
Introduction: Inflammatory bowel disease (IBD) is a chronic inflammatory condition of the gastrointestinal tract that is associated with increased risk of thromboembolic events, both venous and arterial. While this prothrombotic state is well documented, the risk of acute intestinal ischemia (AMI) in this group of patients has not been studied extensively. In this study, we aim to investigate the association and risk of AMI in patients with IBD and their outcomes.
Methods: We utilized data from the National Inpatient Sample (NIS) database from 2016 to 2021 to identify adult patients ( >18 years) with a primary diagnosis of IBD and a secondary diagnosis of AMI. The patients were stratified into two cohorts: those with AMI and those without. The primary outcome was all cause mortality. Secondary outcome included adverse events, ICU stay and respiratory failure. Statistical analysis was performed using StataCorp. 2021
Results: Out of 1.9 million patients admitted with IBD, 7,405 were diagnosed with AMI. Patients with AMI and IBD were older (61.20 vs 54.28 years) had hypertension (54.05% vs 45.70%) and CAD (18.02% vs 14.27%). They also experienced worse outcomes including higher mortality (13.23% vs 1.71%), AKI (34.95% vs 17.02%), shock (23.41% vs 3.63%), respiratory failure (25.84% vs 9.35%), ICU admission (17.68% vs 3.00%) and GI bleeding (11.47% vs 5.20%). Multivariate analysis confirmed that AMI in IBD was associated with increased odds of mortality (aOR 6.07), AKI (aOR 2.57), shock (aOR 6.26), respiratory failure (aOR 2.84), ICU admission (aOR 5.25) and GI bleed (aOR 2.01). They also had higher odds of intestinal perforation (aOR 12.79) and surgical resection (aOR 5.24). IBD itself was independently associated with increased risk of AMI (2.34). All values were statistically significant (P< 0.001).
Discussion: Our analysis demonstrates that patients with IBD have increased risk of developing AMI. This association is likely due to a combination of chronic inflammation, hypercoagulable state, endothelial dysfunction and increased mesenteric metabolic demand. It is associated with increased morbidity and mortality, clinicians should maintain a high index of suspicion for AMI in patients with IBD patients, particularly in patients with comorbid cardiovascular risk factors. Early recognition and intervention may be critical to improving outcomes.
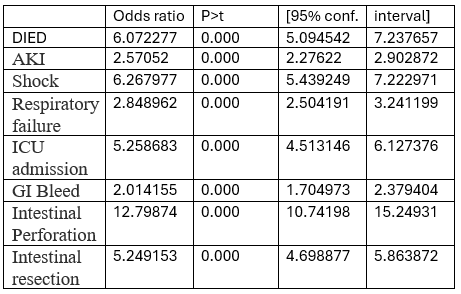
Figure: Multivariate analysis
Disclosures:
Umesh Bhagat indicated no relevant financial relationships.
Ankit Agrawal indicated no relevant financial relationships.
Archana Kharel indicated no relevant financial relationships.
Shalini Tripathi indicated no relevant financial relationships.
Mohamed Abdelbaky indicated no relevant financial relationships.
Archit Garg indicated no relevant financial relationships.
Sukul Khanna indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Luisa Recinos indicated no relevant financial relationships.
Umesh Bhagat, MD1, Ankit Agrawal, 2, Archana Kharel, MD2, Shalini Tripathi, MD2, Mohamed Abdelbaky, MD3, Archit Garg, MD4, Sukul Khanna, MBBS5, Prabhat Kumar, MD6, Luisa Recinos, MD7. P3204 - Is IBD a Predictor of Poor Outcomes in Acute Mesenteric Ischemia?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic, Cleveland, OH; 3Presbyterian Health care, Albuquerque, NM; 4Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 5University College of Medical Sciences and Guru Teg Bahadur Hospital, New Delhi, Delhi, India; 6Virginia Commonwealth University, Richmond, VA; 7Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, Somerset, NJ
Introduction: Inflammatory bowel disease (IBD) is a chronic inflammatory condition of the gastrointestinal tract that is associated with increased risk of thromboembolic events, both venous and arterial. While this prothrombotic state is well documented, the risk of acute intestinal ischemia (AMI) in this group of patients has not been studied extensively. In this study, we aim to investigate the association and risk of AMI in patients with IBD and their outcomes.
Methods: We utilized data from the National Inpatient Sample (NIS) database from 2016 to 2021 to identify adult patients ( >18 years) with a primary diagnosis of IBD and a secondary diagnosis of AMI. The patients were stratified into two cohorts: those with AMI and those without. The primary outcome was all cause mortality. Secondary outcome included adverse events, ICU stay and respiratory failure. Statistical analysis was performed using StataCorp. 2021
Results: Out of 1.9 million patients admitted with IBD, 7,405 were diagnosed with AMI. Patients with AMI and IBD were older (61.20 vs 54.28 years) had hypertension (54.05% vs 45.70%) and CAD (18.02% vs 14.27%). They also experienced worse outcomes including higher mortality (13.23% vs 1.71%), AKI (34.95% vs 17.02%), shock (23.41% vs 3.63%), respiratory failure (25.84% vs 9.35%), ICU admission (17.68% vs 3.00%) and GI bleeding (11.47% vs 5.20%). Multivariate analysis confirmed that AMI in IBD was associated with increased odds of mortality (aOR 6.07), AKI (aOR 2.57), shock (aOR 6.26), respiratory failure (aOR 2.84), ICU admission (aOR 5.25) and GI bleed (aOR 2.01). They also had higher odds of intestinal perforation (aOR 12.79) and surgical resection (aOR 5.24). IBD itself was independently associated with increased risk of AMI (2.34). All values were statistically significant (P< 0.001).
Discussion: Our analysis demonstrates that patients with IBD have increased risk of developing AMI. This association is likely due to a combination of chronic inflammation, hypercoagulable state, endothelial dysfunction and increased mesenteric metabolic demand. It is associated with increased morbidity and mortality, clinicians should maintain a high index of suspicion for AMI in patients with IBD patients, particularly in patients with comorbid cardiovascular risk factors. Early recognition and intervention may be critical to improving outcomes.
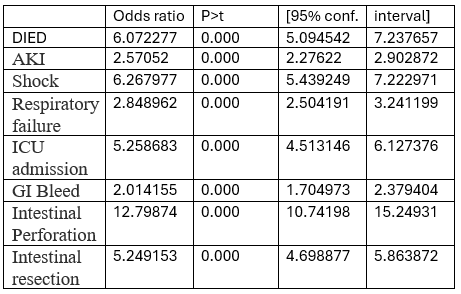
Figure: Multivariate analysis
Disclosures:
Umesh Bhagat indicated no relevant financial relationships.
Ankit Agrawal indicated no relevant financial relationships.
Archana Kharel indicated no relevant financial relationships.
Shalini Tripathi indicated no relevant financial relationships.
Mohamed Abdelbaky indicated no relevant financial relationships.
Archit Garg indicated no relevant financial relationships.
Sukul Khanna indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Luisa Recinos indicated no relevant financial relationships.
Umesh Bhagat, MD1, Ankit Agrawal, 2, Archana Kharel, MD2, Shalini Tripathi, MD2, Mohamed Abdelbaky, MD3, Archit Garg, MD4, Sukul Khanna, MBBS5, Prabhat Kumar, MD6, Luisa Recinos, MD7. P3204 - Is IBD a Predictor of Poor Outcomes in Acute Mesenteric Ischemia?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
