Monday Poster Session
Category: IBD
Fecal Calprotectin as a Predictor of <i>Clostridioides difficile</i> Infection in Inflammatory Bowel Disease: A Retrospective Cohort Study
P3290 - Fecal Calprotectin as a Predictor of Clostridioides difficile Infection in Inflammatory Bowel Disease: A Retrospective Cohort Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Parul Berry, MBBS (she/her/hers)
Mayo Clinic
Rochester, MN
Presenting Author(s)
Parul Berry, MBBS1, Vishwesh Bharadiya, MBBS2, Edward V.. Loftus, MD3, Darrell Pardi, MD, MS, FACG1, Sahil Khanna, MBBS, MD, MS4
1Mayo Clinic, Rochester, MN; 2Mayo Clinic School of Graduate Medical Education, Rochester, MN; 3Mayo Clinic College of Medicine and Science and Mayo Clinic, Rochester, MN; 4Mayo Clinic Rochester, Rochester, MN
Introduction: Fecal calprotectin (FC) is a widely used, non-invasive marker of intestinal inflammation in people with inflammatory bowel disease (IBD). Its role in predicting Clostridioides difficile infection (CDI), a significant complication in this population, is unclear. This study aimed to evaluate whether elevated FC levels are associated with an increased risk of CDI in IBD patients within 90-days.
Methods: We performed a retrospective cohort study of adult IBD patients with no history of CDI who had fecal calprotectin testing followed by evaluation for CDI within 90 days. Those testing positive for CDI were cases, while those testing negative were controls. Receiver operating characteristic analysis was performed, and the optimal fecal calprotectin threshold was identified using the Youden Index. This cut-off was used to dichotomize FC for subsequent analyses. FC was assessed as a binary variable ( >250 µg/g) . Logistic regression was used to analyze the risk of CDI, while Kaplan-Meier curves and Cox proportional hazards models evaluated time to infection, with FC as the primary predictor.
Results: Of 1,675 patients with IBD, 230 (13.7%) developed CDI within 90 days of fecal calprotectin FC testing. The cohort had a mean age of 47.3 years (SD: 19.7). Median FC levels were higher among those who developed CDI (415 µg/g) compared to those who did not (236 µg/g). A threshold of 250 µg/g maximized the Youden Index and was used to dichotomize FC. On logistic regression, FC > 250 µg/g was significantly associated with increased CDI risk (OR 1.73; 95% CI, 1.30–2.31). In our cohort, 16.3% of high-FC patients developed CDI versus 10.6% of those with lower FC. Cox proportional hazards modeling confirmed this association (HR 2.08; 95% CI, 1.59–2.72), indicating more than double the hazard of CDI in the high-FC group. Kaplan-Meier analysis showed significantly earlier CDI onset in the elevated FC group (log-rank P = 0.0002), with median CDI-free survival of 29.2 days (95% CI: 26.1–33.0) compared to 37.5 days (95% CI: 35.0–40.8) in the lower FC group.
Discussion: Higher fecal calprotectin levels were strongly associated with an elevated risk and earlier onset of CDI infection in IBD patients. These results highlight FC’s potential as a clinical tool for identifying individuals at higher risk of CDI. Integrating FC into routine risk stratification may enhance CDI monitoring, support antimicrobial stewardship, and guide timely intervention strategies in the IBD population.
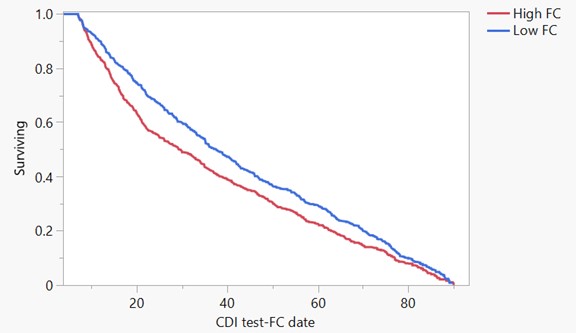
Figure: Time to CDI stratified by FC > 250 µg/g (red) vs ≤ 250 (blue). FC > 250 was linked to shorter CDI-free survival (p =0.0002).
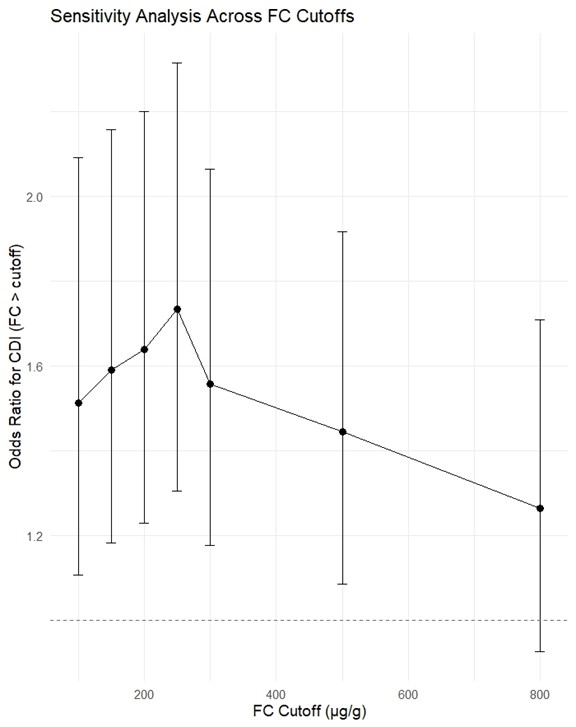
Figure: Odds ratios (95% CI) for CDI across various FC cutoffs. The strongest association was at ~250 µg/g. Association weakened at higher cutoffs.
Disclosures:
Parul Berry indicated no relevant financial relationships.
Vishwesh Bharadiya indicated no relevant financial relationships.
Edward Loftus: AbbVie – Consultant, Grant/Research Support. Abivax – Consultant. Astellas – Consultant. Avalo – Consultant. Biocon – Consultant. Celltrion – Consultant. Eli Lilly – Advisory Committee/Board Member, Consultant. Exact Sciences – Stock Options. Fresenius Kabi – Consultant. Genentech – Advisory Committee/Board Member. Gilead – Consultant, Grant/Research Support. Iota Biosciences – Consultant. Iterative Health – Consultant. Johnson & Johnson – Consultant, Grant/Research Support. Merck – Consultant, Grant/Research Support. Moderna – Stock Options. Morphic – Consultant. Ono Pharma – Consultant. Spyre – Advisory Committee/Board Member. Takeda – Consultant, Grant/Research Support. TR1X Bio – Consultant.
Darrell Pardi: Applied Molecular Transport – Consultant. ExeGI Pharma LC – Grant/Research Support. Janssen – Advisory Committee/Board Member. Lilly Medical – Consultant. Pfizer – Consultant. Rise Therapeutics – Grant/Research Support. Takeda – Consultant. Vedanta Bio Sciences INC – Grant/Research Support.
Sahil Khanna: Ferring Pharmaceuticals – Advisor or Review Panel Member. Finch Therapeutics – Grant/Research Support. Immuron Limited – Consultant. Jetson Probiotics – Stock Options. Niche Pharmaceuticals – Consultant. Rebiotix – Grant/Research Support. Seres Therapeutics – Grant/Research Support. Vedanta BioSciences – Grant/Research Support.
Parul Berry, MBBS1, Vishwesh Bharadiya, MBBS2, Edward V.. Loftus, MD3, Darrell Pardi, MD, MS, FACG1, Sahil Khanna, MBBS, MD, MS4. P3290 - Fecal Calprotectin as a Predictor of <i>Clostridioides difficile</i> Infection in Inflammatory Bowel Disease: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Rochester, MN; 2Mayo Clinic School of Graduate Medical Education, Rochester, MN; 3Mayo Clinic College of Medicine and Science and Mayo Clinic, Rochester, MN; 4Mayo Clinic Rochester, Rochester, MN
Introduction: Fecal calprotectin (FC) is a widely used, non-invasive marker of intestinal inflammation in people with inflammatory bowel disease (IBD). Its role in predicting Clostridioides difficile infection (CDI), a significant complication in this population, is unclear. This study aimed to evaluate whether elevated FC levels are associated with an increased risk of CDI in IBD patients within 90-days.
Methods: We performed a retrospective cohort study of adult IBD patients with no history of CDI who had fecal calprotectin testing followed by evaluation for CDI within 90 days. Those testing positive for CDI were cases, while those testing negative were controls. Receiver operating characteristic analysis was performed, and the optimal fecal calprotectin threshold was identified using the Youden Index. This cut-off was used to dichotomize FC for subsequent analyses. FC was assessed as a binary variable ( >250 µg/g) . Logistic regression was used to analyze the risk of CDI, while Kaplan-Meier curves and Cox proportional hazards models evaluated time to infection, with FC as the primary predictor.
Results: Of 1,675 patients with IBD, 230 (13.7%) developed CDI within 90 days of fecal calprotectin FC testing. The cohort had a mean age of 47.3 years (SD: 19.7). Median FC levels were higher among those who developed CDI (415 µg/g) compared to those who did not (236 µg/g). A threshold of 250 µg/g maximized the Youden Index and was used to dichotomize FC. On logistic regression, FC > 250 µg/g was significantly associated with increased CDI risk (OR 1.73; 95% CI, 1.30–2.31). In our cohort, 16.3% of high-FC patients developed CDI versus 10.6% of those with lower FC. Cox proportional hazards modeling confirmed this association (HR 2.08; 95% CI, 1.59–2.72), indicating more than double the hazard of CDI in the high-FC group. Kaplan-Meier analysis showed significantly earlier CDI onset in the elevated FC group (log-rank P = 0.0002), with median CDI-free survival of 29.2 days (95% CI: 26.1–33.0) compared to 37.5 days (95% CI: 35.0–40.8) in the lower FC group.
Discussion: Higher fecal calprotectin levels were strongly associated with an elevated risk and earlier onset of CDI infection in IBD patients. These results highlight FC’s potential as a clinical tool for identifying individuals at higher risk of CDI. Integrating FC into routine risk stratification may enhance CDI monitoring, support antimicrobial stewardship, and guide timely intervention strategies in the IBD population.
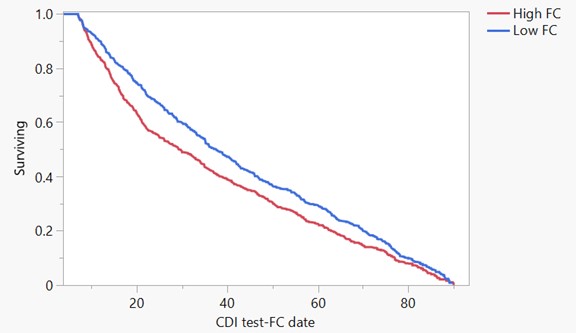
Figure: Time to CDI stratified by FC > 250 µg/g (red) vs ≤ 250 (blue). FC > 250 was linked to shorter CDI-free survival (p =0.0002).
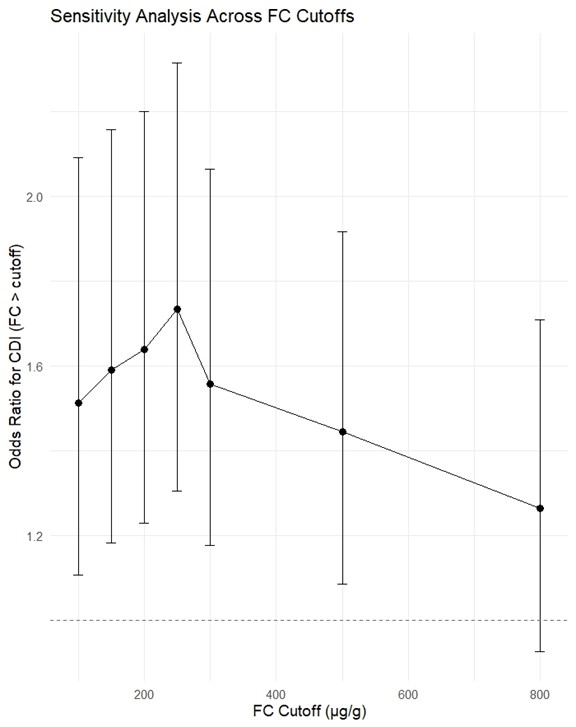
Figure: Odds ratios (95% CI) for CDI across various FC cutoffs. The strongest association was at ~250 µg/g. Association weakened at higher cutoffs.
Disclosures:
Parul Berry indicated no relevant financial relationships.
Vishwesh Bharadiya indicated no relevant financial relationships.
Edward Loftus: AbbVie – Consultant, Grant/Research Support. Abivax – Consultant. Astellas – Consultant. Avalo – Consultant. Biocon – Consultant. Celltrion – Consultant. Eli Lilly – Advisory Committee/Board Member, Consultant. Exact Sciences – Stock Options. Fresenius Kabi – Consultant. Genentech – Advisory Committee/Board Member. Gilead – Consultant, Grant/Research Support. Iota Biosciences – Consultant. Iterative Health – Consultant. Johnson & Johnson – Consultant, Grant/Research Support. Merck – Consultant, Grant/Research Support. Moderna – Stock Options. Morphic – Consultant. Ono Pharma – Consultant. Spyre – Advisory Committee/Board Member. Takeda – Consultant, Grant/Research Support. TR1X Bio – Consultant.
Darrell Pardi: Applied Molecular Transport – Consultant. ExeGI Pharma LC – Grant/Research Support. Janssen – Advisory Committee/Board Member. Lilly Medical – Consultant. Pfizer – Consultant. Rise Therapeutics – Grant/Research Support. Takeda – Consultant. Vedanta Bio Sciences INC – Grant/Research Support.
Sahil Khanna: Ferring Pharmaceuticals – Advisor or Review Panel Member. Finch Therapeutics – Grant/Research Support. Immuron Limited – Consultant. Jetson Probiotics – Stock Options. Niche Pharmaceuticals – Consultant. Rebiotix – Grant/Research Support. Seres Therapeutics – Grant/Research Support. Vedanta BioSciences – Grant/Research Support.
Parul Berry, MBBS1, Vishwesh Bharadiya, MBBS2, Edward V.. Loftus, MD3, Darrell Pardi, MD, MS, FACG1, Sahil Khanna, MBBS, MD, MS4. P3290 - Fecal Calprotectin as a Predictor of <i>Clostridioides difficile</i> Infection in Inflammatory Bowel Disease: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
