Monday Poster Session
Category: IBD
P3358 - Anticipating the Unseen: Foreign Body Ingestion Complicating Penetrating Crohn's Disease in a Non-Verbal Adolescent With Autism Spectrum Disorder
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Meredith R. Kline, MD (she/her/hers)
University of Chicago Medicine, Inflammatory Bowel Disease Center
Chicago, IL
Presenting Author(s)
Meredith R. Kline, MD1, Baddr Shakhsheer, MD2, Tessa George, BSc1, Amelia Kellar, MD, MSc1
1University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL; 2University of Chicago Pritzker School of Medicine, Chicago, IL
Introduction: Penetrating Crohn’s disease (CD) frequently necessitates coordinated medical and surgical management. In individuals with autism spectrum disorder (ASD), diagnostic and disease monitoring challenges arise due to communication limitations, atypical symptom presentation, and adherence. This case presents a rare complication of penetrating CD in an adolescent with ASD, marked by recurrent symptoms following initial clinical improvement.
Case Description/
Methods: A 17-year-old male with ASD presented with two weeks of abdominal pain, diarrhea, and weight loss. Computed tomography (CT) demonstrated terminal ileitis, a 15 cm stricture, ileosigmoid fistula, and abscess. Inflammatory markers (IMs) were elevated (C-reactive protein (CRP) 30 mg/L, fecal calprotectin 272 μg/g). He improved clinically on intravenous antibiotics and was discharged on oral antibiotics and exclusive enteral nutrition (EEN).
Three weeks later, he re-presented with worsening abdominal pain and emesis. Colonoscopy demonstrated severe inflammation in the terminal ileum (TI), and biopsies were confirmatory for CD. Infliximab (IFX) was initiated [10mg/kg standard induction dosing at 0,2,6 weeks, then q8week maintenance dosing], and he reached therapeutic trough drug levels [44ug/mL at week 2, 38ug/mL at week 6] with a robust clinical response. He achieved symptom control, but had difficulty complying with EEN at home, and five months later presented with recurrent abdominal pain. CRP increased to 109 mg/L), and repeat CT revealed progression of inflammation in the TI and cecum with persistence of ileosigmoid fistula. After one month of bowel rest and total parenteral nutrition (TPN), he underwent laparoscopic ileocecectomy with removal of 20.5 cm ileum and 3.2 cm proximal colon.
Intraoperatively, adhesions and a persistent fistula were identified (Figure 1), along with a foreign body- the extremity of an action figure embedded in the TI (Figure 2). He recovered well after surgery, experiencing no disruptions to IFX regimen, and has remained in clinical and endoscopic remission.
Discussion: This case provides important insights into the management of penetrating Crohn’s disease and comorbid ASD. A foreign body, initially suspected to be a loculated abscess on preoperative imaging was identified intraoperatively. This finding highlights the unique diagnostic challenges in this population and underscores the importance of maintaining a broad differential when interpreting symptoms and imaging in the setting of acute clinical change.
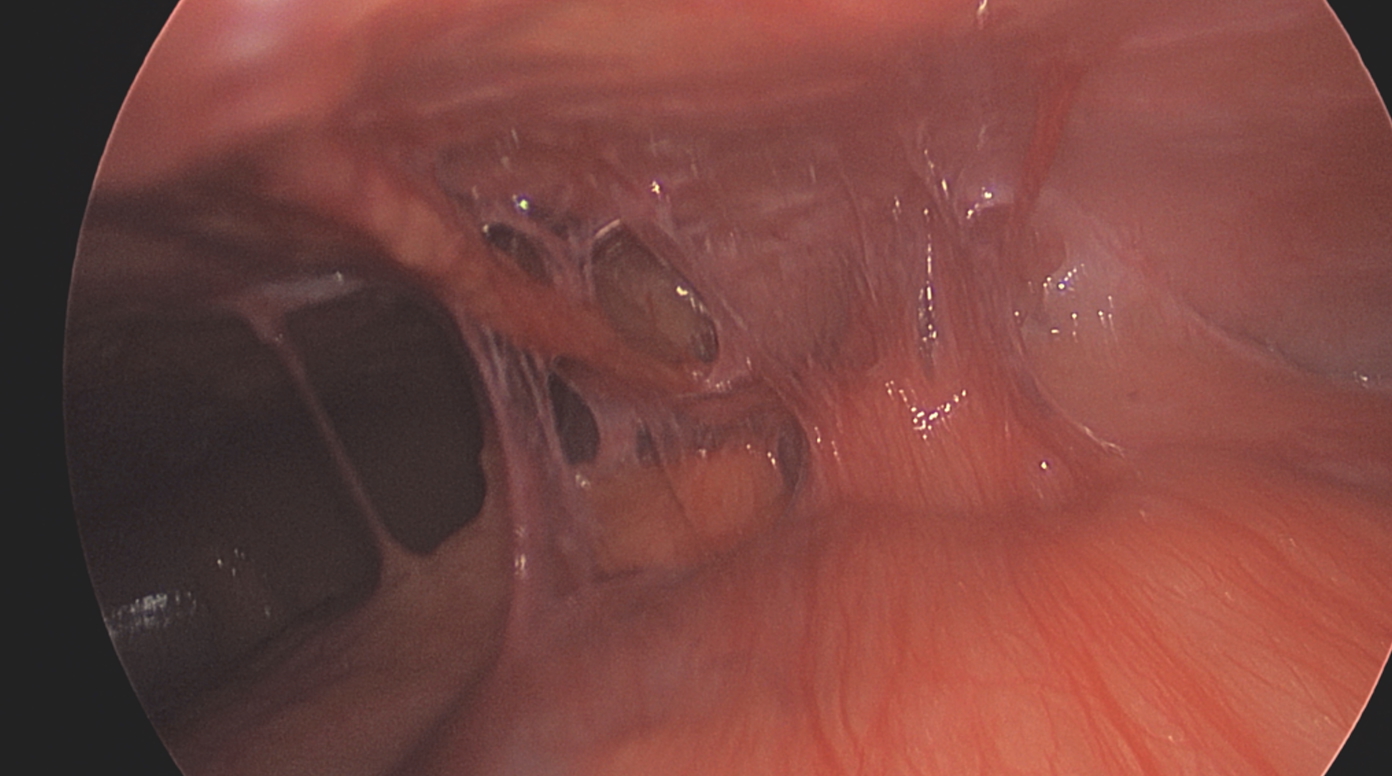
Figure: Figure 1- Adhesion to Anterior Abdominal Wall

Figure: Figure 2- Intraluminal Foreign Body
Disclosures:
Meredith Kline indicated no relevant financial relationships.
Baddr Shakhsheer indicated no relevant financial relationships.
Tessa George indicated no relevant financial relationships.
Amelia Kellar indicated no relevant financial relationships.
Meredith R. Kline, MD1, Baddr Shakhsheer, MD2, Tessa George, BSc1, Amelia Kellar, MD, MSc1. P3358 - Anticipating the Unseen: Foreign Body Ingestion Complicating Penetrating Crohn's Disease in a Non-Verbal Adolescent With Autism Spectrum Disorder, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL; 2University of Chicago Pritzker School of Medicine, Chicago, IL
Introduction: Penetrating Crohn’s disease (CD) frequently necessitates coordinated medical and surgical management. In individuals with autism spectrum disorder (ASD), diagnostic and disease monitoring challenges arise due to communication limitations, atypical symptom presentation, and adherence. This case presents a rare complication of penetrating CD in an adolescent with ASD, marked by recurrent symptoms following initial clinical improvement.
Case Description/
Methods: A 17-year-old male with ASD presented with two weeks of abdominal pain, diarrhea, and weight loss. Computed tomography (CT) demonstrated terminal ileitis, a 15 cm stricture, ileosigmoid fistula, and abscess. Inflammatory markers (IMs) were elevated (C-reactive protein (CRP) 30 mg/L, fecal calprotectin 272 μg/g). He improved clinically on intravenous antibiotics and was discharged on oral antibiotics and exclusive enteral nutrition (EEN).
Three weeks later, he re-presented with worsening abdominal pain and emesis. Colonoscopy demonstrated severe inflammation in the terminal ileum (TI), and biopsies were confirmatory for CD. Infliximab (IFX) was initiated [10mg/kg standard induction dosing at 0,2,6 weeks, then q8week maintenance dosing], and he reached therapeutic trough drug levels [44ug/mL at week 2, 38ug/mL at week 6] with a robust clinical response. He achieved symptom control, but had difficulty complying with EEN at home, and five months later presented with recurrent abdominal pain. CRP increased to 109 mg/L), and repeat CT revealed progression of inflammation in the TI and cecum with persistence of ileosigmoid fistula. After one month of bowel rest and total parenteral nutrition (TPN), he underwent laparoscopic ileocecectomy with removal of 20.5 cm ileum and 3.2 cm proximal colon.
Intraoperatively, adhesions and a persistent fistula were identified (Figure 1), along with a foreign body- the extremity of an action figure embedded in the TI (Figure 2). He recovered well after surgery, experiencing no disruptions to IFX regimen, and has remained in clinical and endoscopic remission.
Discussion: This case provides important insights into the management of penetrating Crohn’s disease and comorbid ASD. A foreign body, initially suspected to be a loculated abscess on preoperative imaging was identified intraoperatively. This finding highlights the unique diagnostic challenges in this population and underscores the importance of maintaining a broad differential when interpreting symptoms and imaging in the setting of acute clinical change.
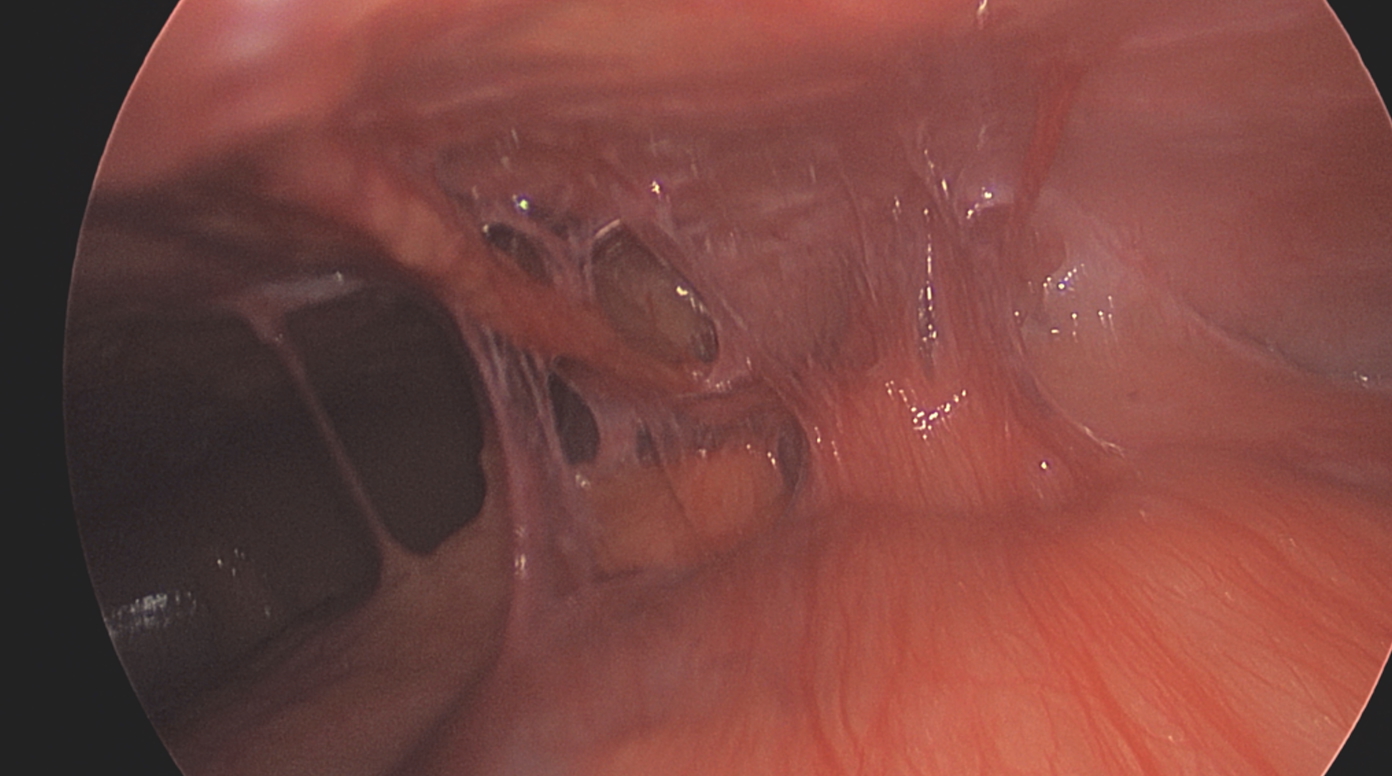
Figure: Figure 1- Adhesion to Anterior Abdominal Wall

Figure: Figure 2- Intraluminal Foreign Body
Disclosures:
Meredith Kline indicated no relevant financial relationships.
Baddr Shakhsheer indicated no relevant financial relationships.
Tessa George indicated no relevant financial relationships.
Amelia Kellar indicated no relevant financial relationships.
Meredith R. Kline, MD1, Baddr Shakhsheer, MD2, Tessa George, BSc1, Amelia Kellar, MD, MSc1. P3358 - Anticipating the Unseen: Foreign Body Ingestion Complicating Penetrating Crohn's Disease in a Non-Verbal Adolescent With Autism Spectrum Disorder, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
