Monday Poster Session
Category: IBD
P3357 - Smoking Cessation Leading to Ulcerative Colitis and Autoimmune Pancreatitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hetal Patel, MD
University of Illinois College of Medicine
Chicago, IL
Presenting Author(s)
Hetal Patel, MD1, Yousif Esho, MD1, Sean C. Tompkins, MD, PhD2, Itishree Trivedi, MD3
1University of Illinois College of Medicine, Chicago, IL; 2University of Illinois Chicago, Chicago, IL; 3University of Illinois, Chicago, IL
Introduction: Type 2 Autoimmune pancreatitis (AIP), an exceedingly rare diagnosis, is commonly concurrent with a diagnosis of Ulcerative Colitis (UC). The prevalence of UC in patients with known Type 2 AIP can vary from 16-83%, though only 0.5-0.6% of all UC patients develop Type 2 AIP. Here, we present a case of a 37-year-old-male who was newly diagnosed with both pancreatitis and severe pancolonic UC that manifested after abrupt smoking cessation.
Case Description/
Methods: A 37-year-old male with a history of alcohol and tobacco use disorder presented with nausea, vomiting, diarrhea, and abdominal cramping that resolved with amoxicillin-clavulanic acid. Four months later, he abruptly stopped smoking and developed severe lower abdominal pain with hematochezia. His labs showed CRP 19.5MG/L and lipase 346U/L. CT of the abdomen and pelvis showed long segment bowel wall thickening with enhancement of the sigmoid colon and rectum, and a 2.5 cm hypodense lesion in the pancreatic head. IgG4 level was 85mg/dL. Endoscopic ultrasound (EUS) demonstrated pancreatic parenchymal abnormalities in the entire pancreas. Colonoscopy showed severe, contiguous pancolonic inflammation, consistent with endoscopic Mayo score of 3, with biopsy confirming a diagnosis of UC. He was initially treated with intravenous steroids with marked clinical improvement. He was transitioned to oral steroids on discharge and then initiated on infliximab and azathioprine therapy, with complete resolution UC symptoms and parenchymal pancreas injury and lesion on cross-sectional imaging with MRI. Given that the pancreatic parenchymal abnormality responded to steroids and biologic agents, in the setting of diagnosed IBD, with normal IgG4 levels, he was diagnosed with Type 2 Autoimmune Pancreatitis.
Discussion: We present a case of UC and Type 2 AIP, with abrupt onset after smoking cessation. Though the association of smoking cessation with onset of UC is a well-described phenomenon, there is lack of consensus on a potential protective effect of smoking on improved UC outcomes. Conversely, for AIP, smoking cessation is an important part of disease management. Tobacco smoking has been associated with significantly more pancreatic damage, and potentially disease relapse rates, impacting the clinical course and increasing rates of complications, such as diabetes or exocrine pancreatic insufficiency. This case highlights the complex role of nicotine in immune modulation and clinical course of UC and AIP.
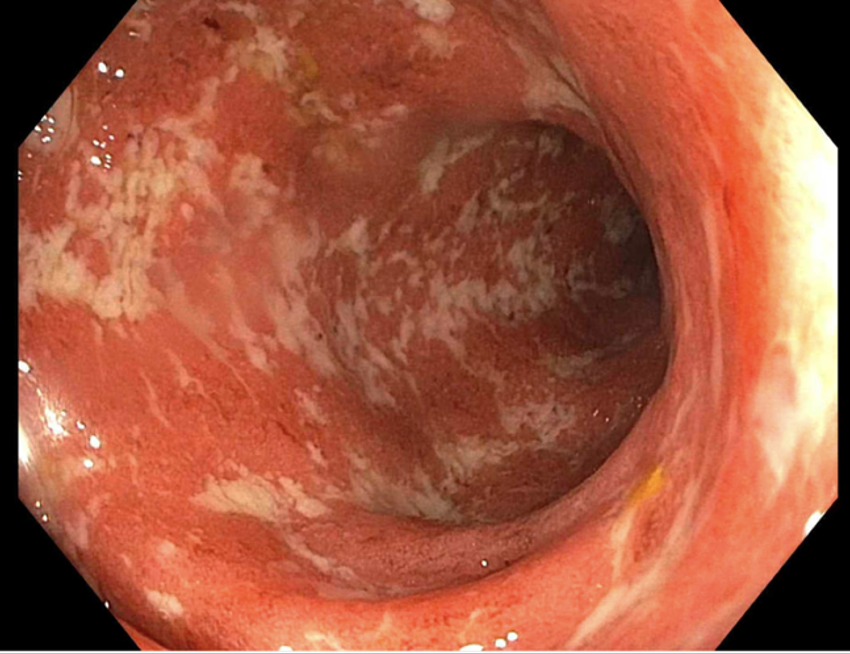
Figure: Figure 1: Index colonoscopy during diagnosis of Ulcerative Colitis
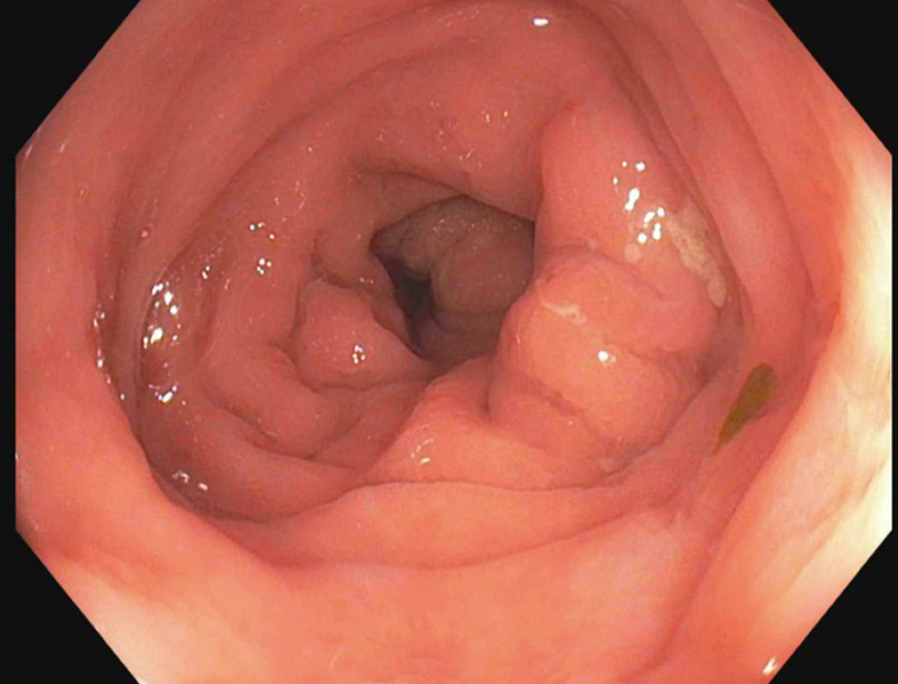
Figure: Figure 2: Colonoscopy after 6 months of therapy
Disclosures:
Hetal Patel indicated no relevant financial relationships.
Yousif Esho indicated no relevant financial relationships.
Sean Tompkins indicated no relevant financial relationships.
Itishree Trivedi indicated no relevant financial relationships.
Hetal Patel, MD1, Yousif Esho, MD1, Sean C. Tompkins, MD, PhD2, Itishree Trivedi, MD3. P3357 - Smoking Cessation Leading to Ulcerative Colitis and Autoimmune Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Illinois College of Medicine, Chicago, IL; 2University of Illinois Chicago, Chicago, IL; 3University of Illinois, Chicago, IL
Introduction: Type 2 Autoimmune pancreatitis (AIP), an exceedingly rare diagnosis, is commonly concurrent with a diagnosis of Ulcerative Colitis (UC). The prevalence of UC in patients with known Type 2 AIP can vary from 16-83%, though only 0.5-0.6% of all UC patients develop Type 2 AIP. Here, we present a case of a 37-year-old-male who was newly diagnosed with both pancreatitis and severe pancolonic UC that manifested after abrupt smoking cessation.
Case Description/
Methods: A 37-year-old male with a history of alcohol and tobacco use disorder presented with nausea, vomiting, diarrhea, and abdominal cramping that resolved with amoxicillin-clavulanic acid. Four months later, he abruptly stopped smoking and developed severe lower abdominal pain with hematochezia. His labs showed CRP 19.5MG/L and lipase 346U/L. CT of the abdomen and pelvis showed long segment bowel wall thickening with enhancement of the sigmoid colon and rectum, and a 2.5 cm hypodense lesion in the pancreatic head. IgG4 level was 85mg/dL. Endoscopic ultrasound (EUS) demonstrated pancreatic parenchymal abnormalities in the entire pancreas. Colonoscopy showed severe, contiguous pancolonic inflammation, consistent with endoscopic Mayo score of 3, with biopsy confirming a diagnosis of UC. He was initially treated with intravenous steroids with marked clinical improvement. He was transitioned to oral steroids on discharge and then initiated on infliximab and azathioprine therapy, with complete resolution UC symptoms and parenchymal pancreas injury and lesion on cross-sectional imaging with MRI. Given that the pancreatic parenchymal abnormality responded to steroids and biologic agents, in the setting of diagnosed IBD, with normal IgG4 levels, he was diagnosed with Type 2 Autoimmune Pancreatitis.
Discussion: We present a case of UC and Type 2 AIP, with abrupt onset after smoking cessation. Though the association of smoking cessation with onset of UC is a well-described phenomenon, there is lack of consensus on a potential protective effect of smoking on improved UC outcomes. Conversely, for AIP, smoking cessation is an important part of disease management. Tobacco smoking has been associated with significantly more pancreatic damage, and potentially disease relapse rates, impacting the clinical course and increasing rates of complications, such as diabetes or exocrine pancreatic insufficiency. This case highlights the complex role of nicotine in immune modulation and clinical course of UC and AIP.
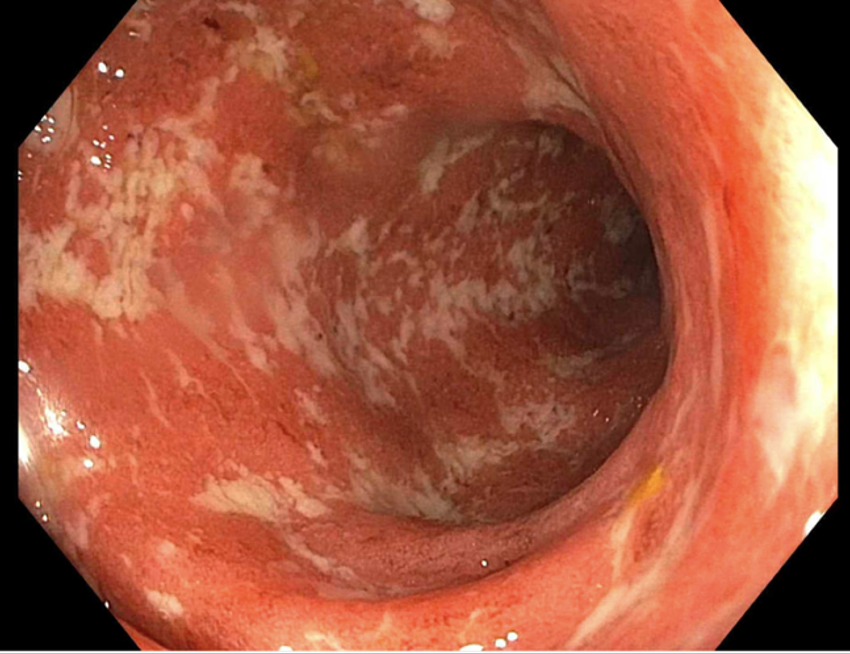
Figure: Figure 1: Index colonoscopy during diagnosis of Ulcerative Colitis
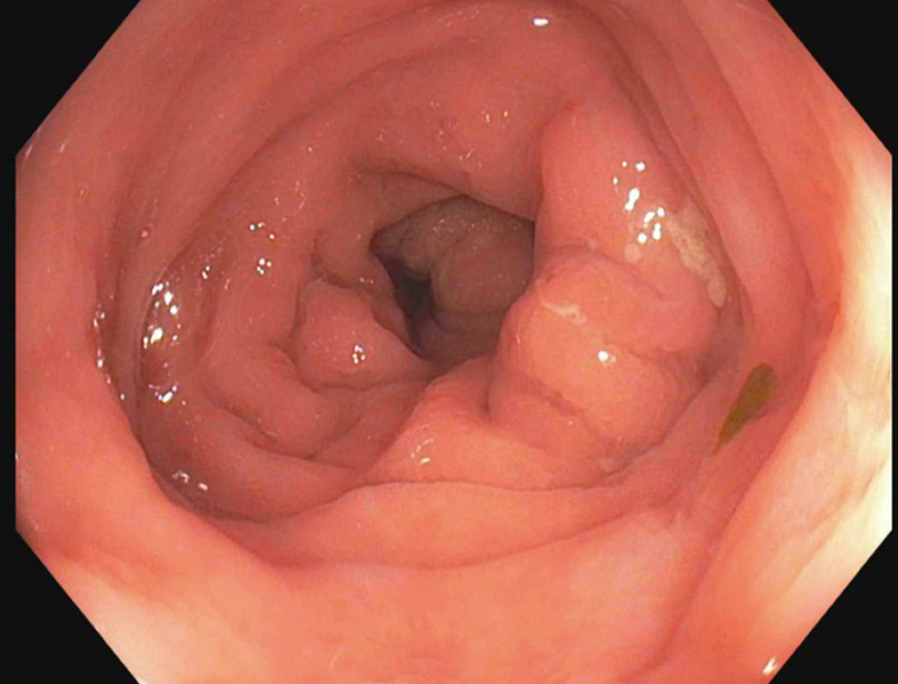
Figure: Figure 2: Colonoscopy after 6 months of therapy
Disclosures:
Hetal Patel indicated no relevant financial relationships.
Yousif Esho indicated no relevant financial relationships.
Sean Tompkins indicated no relevant financial relationships.
Itishree Trivedi indicated no relevant financial relationships.
Hetal Patel, MD1, Yousif Esho, MD1, Sean C. Tompkins, MD, PhD2, Itishree Trivedi, MD3. P3357 - Smoking Cessation Leading to Ulcerative Colitis and Autoimmune Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
