Monday Poster Session
Category: IBD
P3356 - Toxic Proctitis of the Hartmann’s Pouch Requiring Proctectomy in Ulcerative Colitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- GB
Grant Barber, MD, MS
Stanford Health Care
Stanford, CA
Presenting Author(s)
Samuel Simpson, MD, Yan Jiang, MD, Andrew Shelton, MD, Grant Barber, MD, MS
Stanford Health Care, Stanford, CA
Introduction: Toxic megacolon (TM) is a devastating complication in ulcerative colitis (UC). Despite advances in medical management, most cases require surgical intervention which results in rapid clinical resolution. Active disease in the rectal stump is often well controlled with topical therapies. Herein, we present a rare case of recurrent TM of the remnant rectal stump.
Case Description/
Methods: The patient is a 24-year-old male with ulcerative pancolitis complicated by TM one month status post total abdominal colectomy (TAC) with ileostomy and Hartmann pouch who initially represented to the Stanford Hospital with an incisional wound dehiscence. He underwent mechanical wound debridement with wound vacuum placement. Flexible sigmoidoscopy with colorectal surgery at that time was notable for severe proctitis without evidence of cytomegalovirus. The patient was started on topical mesalamine suppositories and budesonide foam.
The patient was preparing for discharge when he developed distributive shock and was transferred to the intensive care unit. Examination was notable for a benign abdomen with an intact midline wound vacuum. He was started on broad-spectrum empiric antibiotics, and computed tomography of the abdomen and pelvis showed marked fluid distention of the Hartmann pouch without free fluid, perforation, or source of intra-abdominal infection (Figure 1). Repeat flexible sigmoidoscopy completed by gastroenterology showed severe necrotizing proctitis (Figure 2).
Given evidence of interval development of necrotizing proctitis, lack of evidence to support stump blowout, and a broadly negative infectious workup, his distributive shock was most felt to be secondary to toxic proctitis of the Hartmann pouch. The colorectal surgery team subsequently completed an urgent abdominal perineal resection (APR) without complications. Surgical pathology showed severe, grade 4 Nancy histologic index active proctitis with mucosal ulcerations. There was no evidence of a perforation or significant abnormalities in adjacent lymph nodes. Postoperatively, the patient’s shock rapidly resolved and discharged home.
Discussion: To our knowledge, we report the first case of isolated toxic proctitis in a Hartmann’s pouch. This case highlights the importance of continuing to consider proctectomy in UC patients with a Hartmann’s pouch after TAC for TM who present with systemic toxicity.
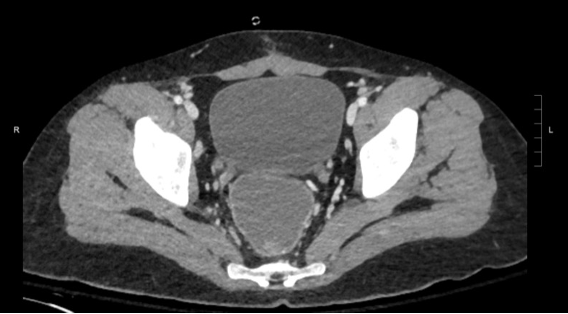
Figure: Figure 1: axial slices of pelvis computed tomography showing severely dilated rectum.
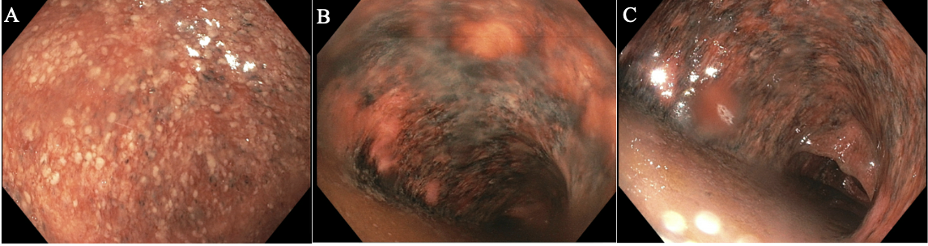
Figure: Figure 2: (A-C) severe inflammation with areas of ulceration and necrotic appearing mucosa seen in the rectum on flexible sigmoidoscopy.
Disclosures:
Samuel Simpson indicated no relevant financial relationships.
Yan Jiang indicated no relevant financial relationships.
Andrew Shelton indicated no relevant financial relationships.
Grant Barber indicated no relevant financial relationships.
Samuel Simpson, MD, Yan Jiang, MD, Andrew Shelton, MD, Grant Barber, MD, MS. P3356 - Toxic Proctitis of the Hartmann’s Pouch Requiring Proctectomy in Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Stanford Health Care, Stanford, CA
Introduction: Toxic megacolon (TM) is a devastating complication in ulcerative colitis (UC). Despite advances in medical management, most cases require surgical intervention which results in rapid clinical resolution. Active disease in the rectal stump is often well controlled with topical therapies. Herein, we present a rare case of recurrent TM of the remnant rectal stump.
Case Description/
Methods: The patient is a 24-year-old male with ulcerative pancolitis complicated by TM one month status post total abdominal colectomy (TAC) with ileostomy and Hartmann pouch who initially represented to the Stanford Hospital with an incisional wound dehiscence. He underwent mechanical wound debridement with wound vacuum placement. Flexible sigmoidoscopy with colorectal surgery at that time was notable for severe proctitis without evidence of cytomegalovirus. The patient was started on topical mesalamine suppositories and budesonide foam.
The patient was preparing for discharge when he developed distributive shock and was transferred to the intensive care unit. Examination was notable for a benign abdomen with an intact midline wound vacuum. He was started on broad-spectrum empiric antibiotics, and computed tomography of the abdomen and pelvis showed marked fluid distention of the Hartmann pouch without free fluid, perforation, or source of intra-abdominal infection (Figure 1). Repeat flexible sigmoidoscopy completed by gastroenterology showed severe necrotizing proctitis (Figure 2).
Given evidence of interval development of necrotizing proctitis, lack of evidence to support stump blowout, and a broadly negative infectious workup, his distributive shock was most felt to be secondary to toxic proctitis of the Hartmann pouch. The colorectal surgery team subsequently completed an urgent abdominal perineal resection (APR) without complications. Surgical pathology showed severe, grade 4 Nancy histologic index active proctitis with mucosal ulcerations. There was no evidence of a perforation or significant abnormalities in adjacent lymph nodes. Postoperatively, the patient’s shock rapidly resolved and discharged home.
Discussion: To our knowledge, we report the first case of isolated toxic proctitis in a Hartmann’s pouch. This case highlights the importance of continuing to consider proctectomy in UC patients with a Hartmann’s pouch after TAC for TM who present with systemic toxicity.
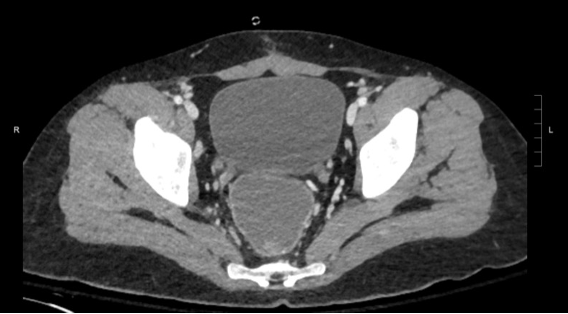
Figure: Figure 1: axial slices of pelvis computed tomography showing severely dilated rectum.
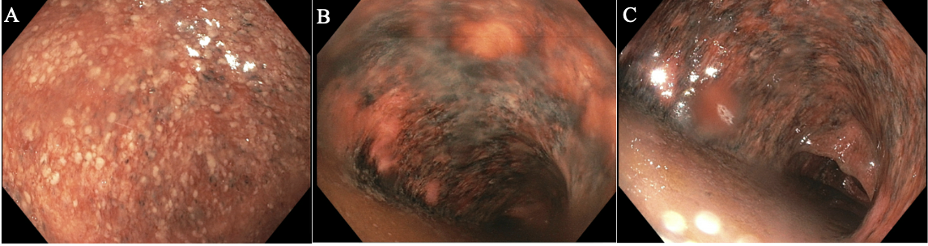
Figure: Figure 2: (A-C) severe inflammation with areas of ulceration and necrotic appearing mucosa seen in the rectum on flexible sigmoidoscopy.
Disclosures:
Samuel Simpson indicated no relevant financial relationships.
Yan Jiang indicated no relevant financial relationships.
Andrew Shelton indicated no relevant financial relationships.
Grant Barber indicated no relevant financial relationships.
Samuel Simpson, MD, Yan Jiang, MD, Andrew Shelton, MD, Grant Barber, MD, MS. P3356 - Toxic Proctitis of the Hartmann’s Pouch Requiring Proctectomy in Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
