Monday Poster Session
Category: IBD
P3350 - The Dietary Information Needs of Minority Patients With Inflammatory Bowel Disease
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SC
Seerat Chawla, BS, MSc (she/her/hers)
Harvard Medical School
Boston, MA
Presenting Author(s)
Seerat Chawla, BS, MSc1, Miram Salama, RD2, Shawna E. Walsh, MD3, Rachel Zhang, BS2, Ashwin Ananthakrishnan, 4, Emily Lopes, MD, MPH2, Bharati Kochar, MD2
1Harvard Medical School, Boston, MA; 2Massachusetts General Hospital, Boston, MA; 3Massachusetts General Hospital, Harvard Medical School, Boston, MA; 4Division of Gastroenterology, Massachusetts General Hospital and Harvard Medical School, Boston, MA
Introduction: Diet profoundly shapes the lived experiences of people with IBD. The lack of evidence for specific diets, however, limits professional support, often resulting in nutrient deficiencies and malnutrition from exclusion diets. Given the dearth of information on cultural diets, Black, Indigenous, and People of Color (BIPOC) with IBD face significant challenges navigating dietary decisions. We aimed to: 1) determine the dietary attitudes and behaviors of BIPOC patients with IBD, 2) identify their unmet dietary information needs, and 3) understand their preferences for dietary information delivery.
Methods: We administered a quantitative survey assessing the dietary counseling available for IBD patients ≥18 years. Descriptive statistics and bivariable analyses with Chi-squared tests were performed to identify differences in dietary guidance for BIPOC and non-BIPOC patients. We also conducted qualitative semi-structured interviews with BIPOC patients with IBD from Massachusetts General Hospital. A deductive-inductive thematic analysis was employed for the qualitative interviews.
Results: Of the 667 who completed the survey, 52 participants identified as BIPOC (Table 1). Comparing BIPOC and non-BIPOC patients, there was no statistical difference between the frequency of dietary discussions (p=0.9) and level of comfort discussing diet with their IBD provider (p=0.3). However, from interviews with BIPOC participants (n=15), three themes emerged regarding the quality of this dietary guidance: psychosocial impact of diet, self-expertise in dietary management, and desired support (Table 2). Subthemes included the role of food in their lives and IBD management, the sense of burdening others, adopting a trial-and-error approach to dietary decision-making, and advocating for oneself in medical spaces. Participants expressed gaps in the applicability of the dietary information they received with a disconnect between general advice designed for Western/white diets and their diets. Despite the trial-and-error approach, there remained a desire for additional support with interest in patient support groups, integration of cultural diets into counseling, and a centralized location for information.
Discussion: In this mixed methods study, we present nuanced contexts that shape the challenges BIPOC patients with IBD face in accessing and implementing dietary guidance. This study also highlights the need to improve the IBD workforce’s capacity to deliver culturally sensitive and inclusive dietary guidance.
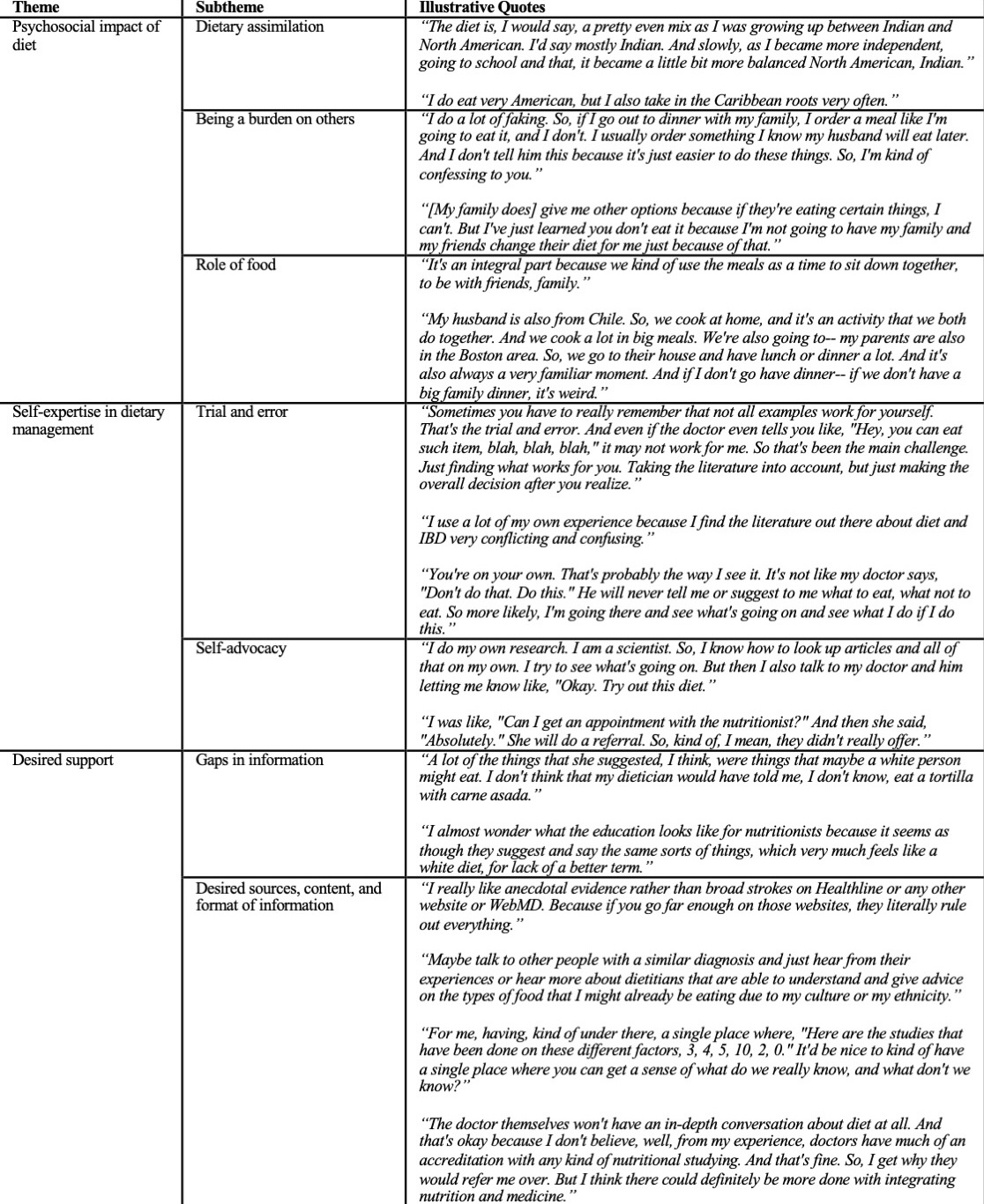
Figure: Table 1: Baseline characteristics of respondents to the survey regarding the nutritional informational needs of people with inflammatory bowel disease (n=667).
BIPOC: Black, Indigenous, People of Color, IBD-U: inflammatory bowel disease-unclassified
*Participants were able to select all responses that applied.
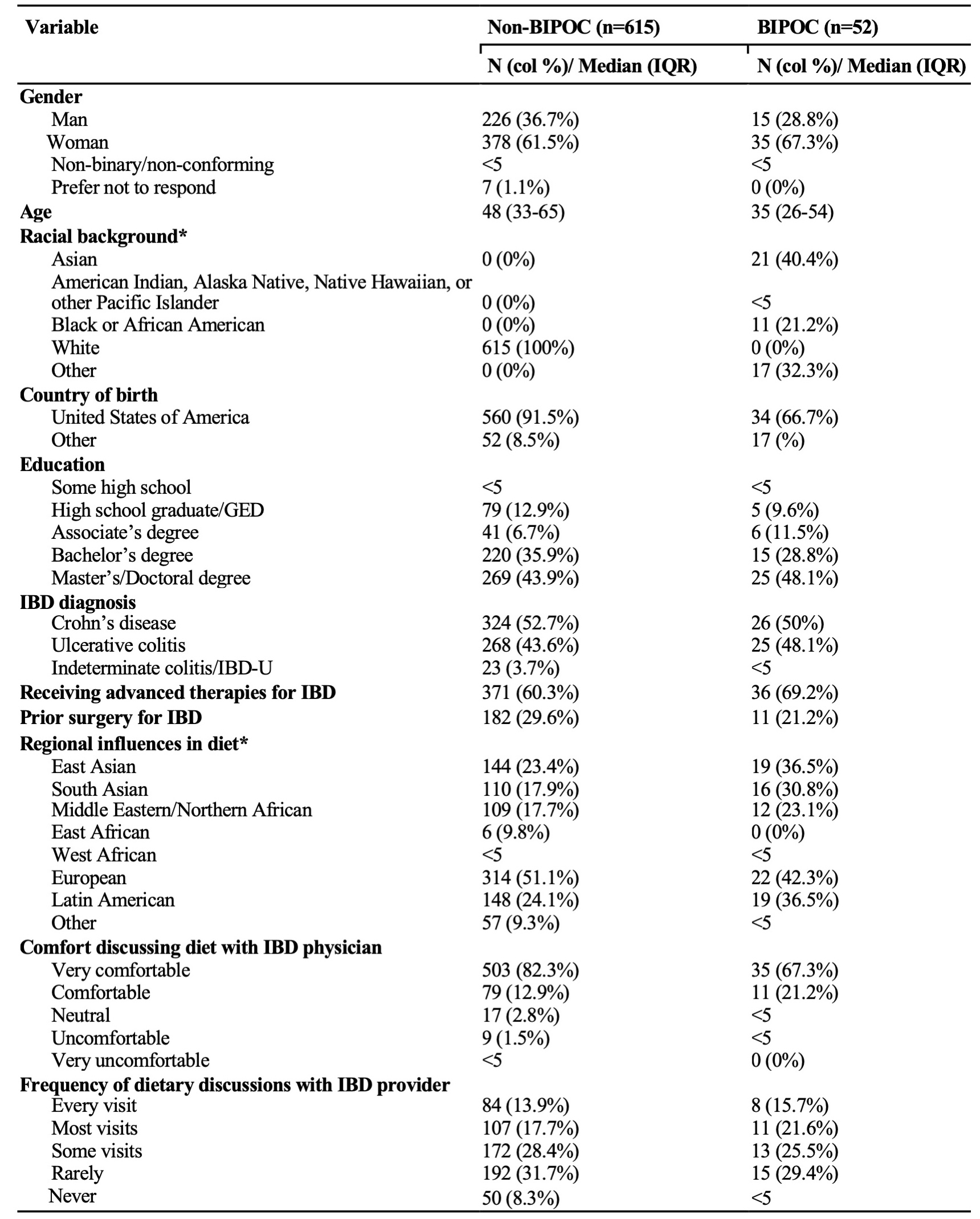
Figure: Table 2: Themes and subthemes with accompanying quotes from individual interviews (n=15).
Disclosures:
Seerat Chawla indicated no relevant financial relationships.
Miram Salama indicated no relevant financial relationships.
Shawna Walsh indicated no relevant financial relationships.
Rachel Zhang indicated no relevant financial relationships.
Ashwin Ananthakrishnan: Takeda – Grant/Research Support.
Emily Lopes indicated no relevant financial relationships.
Bharati Kochar: Bristol Myers Squibb – Advisory Committee/Board Member. Pfizer, Inc – Advisory Committee/Board Member.
Seerat Chawla, BS, MSc1, Miram Salama, RD2, Shawna E. Walsh, MD3, Rachel Zhang, BS2, Ashwin Ananthakrishnan, 4, Emily Lopes, MD, MPH2, Bharati Kochar, MD2. P3350 - The Dietary Information Needs of Minority Patients With Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Harvard Medical School, Boston, MA; 2Massachusetts General Hospital, Boston, MA; 3Massachusetts General Hospital, Harvard Medical School, Boston, MA; 4Division of Gastroenterology, Massachusetts General Hospital and Harvard Medical School, Boston, MA
Introduction: Diet profoundly shapes the lived experiences of people with IBD. The lack of evidence for specific diets, however, limits professional support, often resulting in nutrient deficiencies and malnutrition from exclusion diets. Given the dearth of information on cultural diets, Black, Indigenous, and People of Color (BIPOC) with IBD face significant challenges navigating dietary decisions. We aimed to: 1) determine the dietary attitudes and behaviors of BIPOC patients with IBD, 2) identify their unmet dietary information needs, and 3) understand their preferences for dietary information delivery.
Methods: We administered a quantitative survey assessing the dietary counseling available for IBD patients ≥18 years. Descriptive statistics and bivariable analyses with Chi-squared tests were performed to identify differences in dietary guidance for BIPOC and non-BIPOC patients. We also conducted qualitative semi-structured interviews with BIPOC patients with IBD from Massachusetts General Hospital. A deductive-inductive thematic analysis was employed for the qualitative interviews.
Results: Of the 667 who completed the survey, 52 participants identified as BIPOC (Table 1). Comparing BIPOC and non-BIPOC patients, there was no statistical difference between the frequency of dietary discussions (p=0.9) and level of comfort discussing diet with their IBD provider (p=0.3). However, from interviews with BIPOC participants (n=15), three themes emerged regarding the quality of this dietary guidance: psychosocial impact of diet, self-expertise in dietary management, and desired support (Table 2). Subthemes included the role of food in their lives and IBD management, the sense of burdening others, adopting a trial-and-error approach to dietary decision-making, and advocating for oneself in medical spaces. Participants expressed gaps in the applicability of the dietary information they received with a disconnect between general advice designed for Western/white diets and their diets. Despite the trial-and-error approach, there remained a desire for additional support with interest in patient support groups, integration of cultural diets into counseling, and a centralized location for information.
Discussion: In this mixed methods study, we present nuanced contexts that shape the challenges BIPOC patients with IBD face in accessing and implementing dietary guidance. This study also highlights the need to improve the IBD workforce’s capacity to deliver culturally sensitive and inclusive dietary guidance.
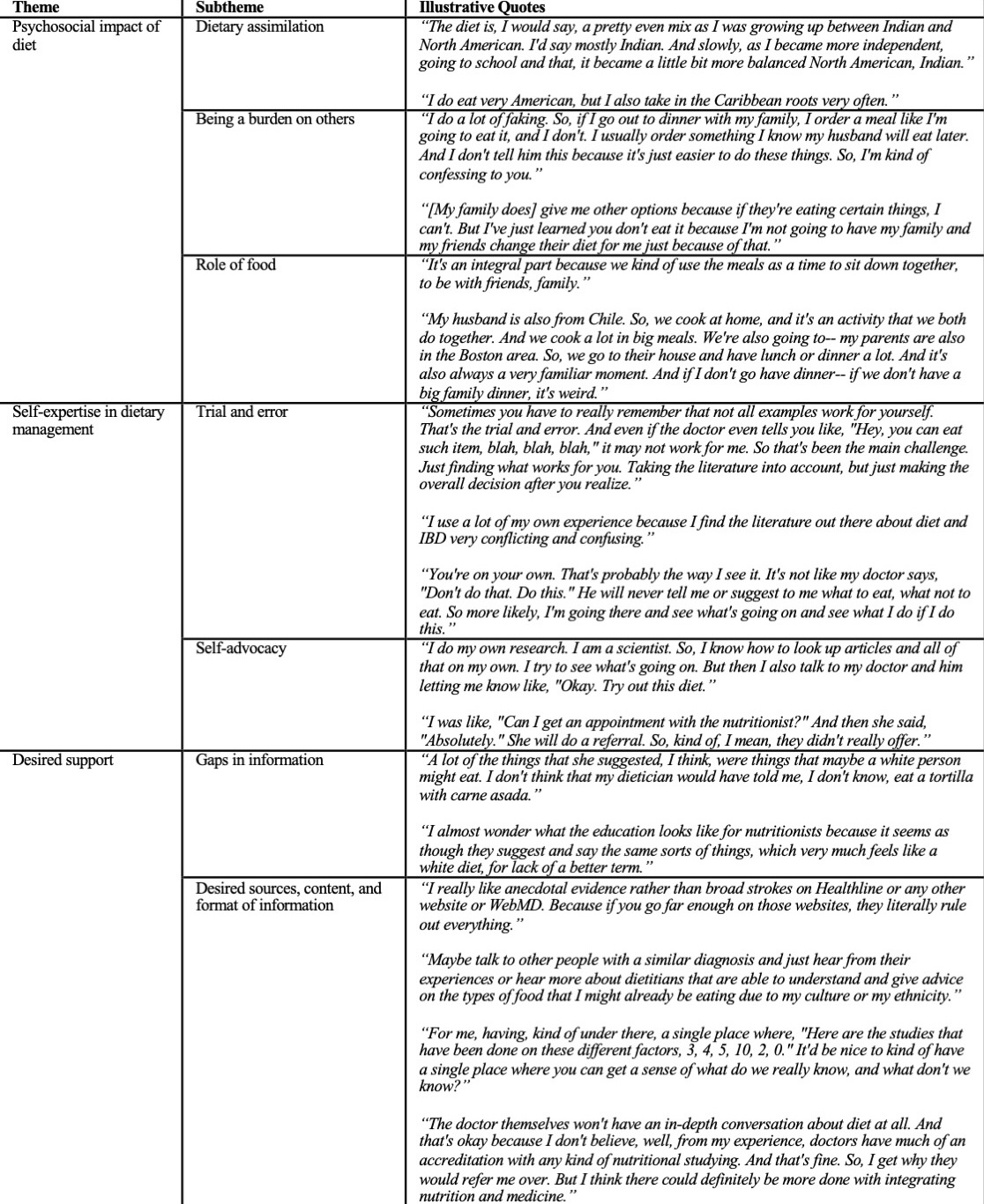
Figure: Table 1: Baseline characteristics of respondents to the survey regarding the nutritional informational needs of people with inflammatory bowel disease (n=667).
BIPOC: Black, Indigenous, People of Color, IBD-U: inflammatory bowel disease-unclassified
*Participants were able to select all responses that applied.
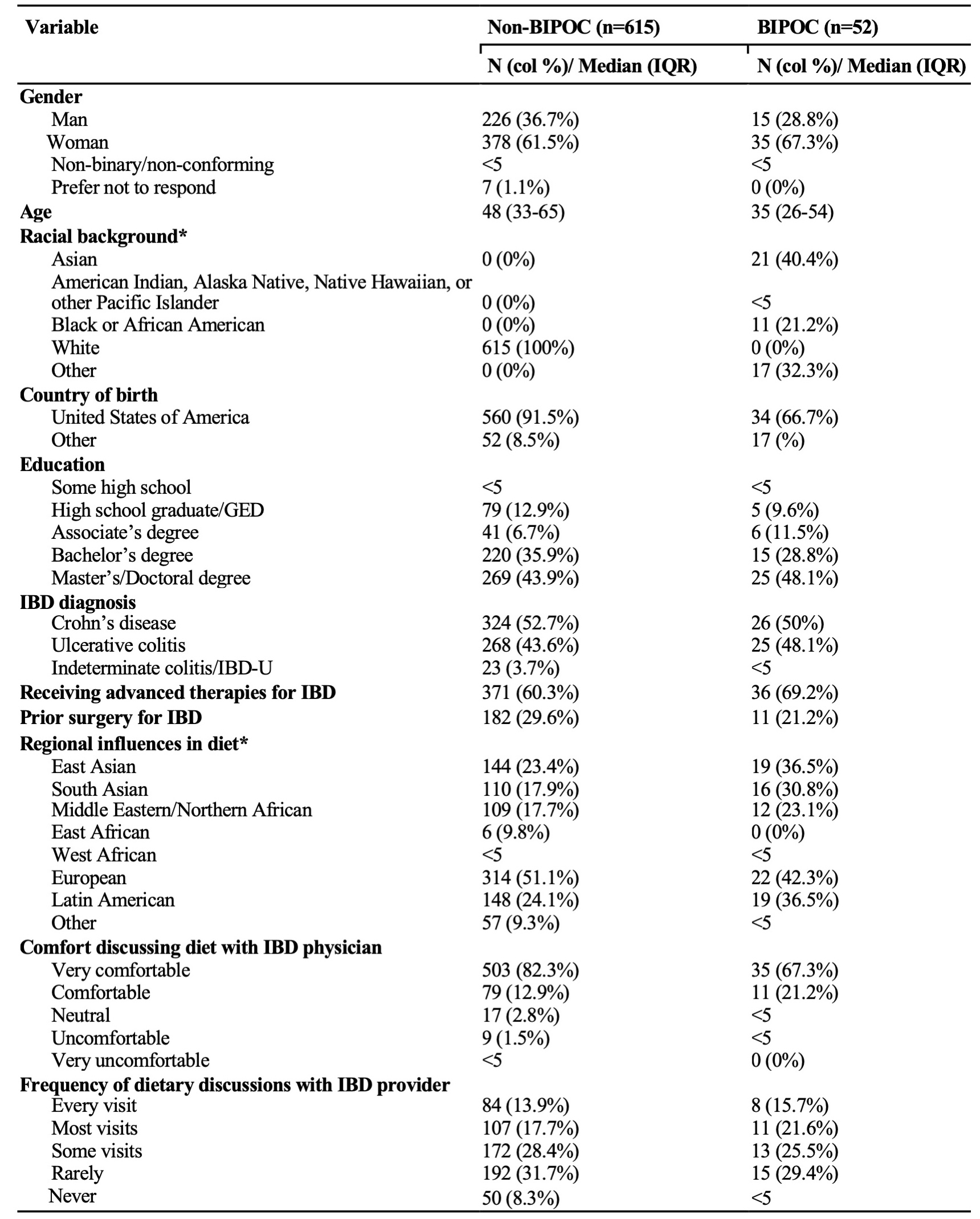
Figure: Table 2: Themes and subthemes with accompanying quotes from individual interviews (n=15).
Disclosures:
Seerat Chawla indicated no relevant financial relationships.
Miram Salama indicated no relevant financial relationships.
Shawna Walsh indicated no relevant financial relationships.
Rachel Zhang indicated no relevant financial relationships.
Ashwin Ananthakrishnan: Takeda – Grant/Research Support.
Emily Lopes indicated no relevant financial relationships.
Bharati Kochar: Bristol Myers Squibb – Advisory Committee/Board Member. Pfizer, Inc – Advisory Committee/Board Member.
Seerat Chawla, BS, MSc1, Miram Salama, RD2, Shawna E. Walsh, MD3, Rachel Zhang, BS2, Ashwin Ananthakrishnan, 4, Emily Lopes, MD, MPH2, Bharati Kochar, MD2. P3350 - The Dietary Information Needs of Minority Patients With Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
