Monday Poster Session
Category: IBD
P3346 - Risk Factors for Underutilization of Bone Mineral Deficiency Screenings in an Older Cohort of Patients With Inflammatory Bowel Disease: A Single Center Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- AE
Ahmed El-Sadek, MD (he/him/his)
UMass Chan Medical School
Worcester, MA
Presenting Author(s)
Harris Feldman, MD, Ahmed El-Sadek, MD, Xiang Li, MS, Michael Wang, MD, Olivia Michaels, BS, Katherine Mackey, BS, Abbas Rupawala, MD, Apurv Soni, MD
UMass Chan Medical School, Worcester, MA
Introduction: The complex interplay of chronic inflammation, malnutrition, and steroid exposures put patients with inflammatory bowel disease (IBD) at a higher risk for disorders of bone mineral deficiency (BMD) compared to the general population. The American Gastroenterological Association (AGA) recommends DEXA screening for males ≥ 50 years old and postmenopausal women as part of evidence-based health maintenance in IBD management. This study will determine DEXA screening rates in this population and examine risk factors associated with DEXA screening.
Methods: In this single center, retrospective cohort study, electronic medical record (EMR) data were extracted to identify patients with IBD age ≥ 50 years using International Classification of Diseases-10 (ICD-10) codes K50 (Crohn’s disease - CD) and K51 (ulcerative colitis - UC) billed by at least one gastroenterology office visit from study period 1/1/2018-12/31/2024. The primary outcome variable of DEXA screening rate was defined as a DEXA scan result during study period for all patients. EMR charts for a subset of patients were reviewed to generate approximate disease duration. Multivariable logistic regression was used to examine association between risk factors (demographic characteristics and disease-time) associated with risk of underutilization of DEXA screening.
Results: Of 895 IBD patients who met the study criteria, 47.8% had UC and 52.2% had CD. Average age among the analytic sample was 63.8 years (SD: 9.5), 49.6% male, majority were non-Hispanic White (91.0%), nearly half had a smoking history (46.7%), nearly half of the sample (45.9%) had Medicare insurance. Among those patients who had complete information about the onset of disease (n = 257, 28.7%), the average disease duration was 18.0 years (SD: 16.1). Overall, only a third of eligible patients received a DEXA scan screening (n = 282, 31.5%). After adjusting for covariates, age group 50-59 years and male gender were associated with 53.0% (OR 0.47 [0.22 , 0.98]) and 87.1% (OR 0.13 [0.09 , 0.18]) lower odds of DEXA screening, respectively. Medicaid insurance was associated with 47.6% (OR 0.52 [0.28 , 0.97]) lower odds, though this was only seen in the unadjusted model.
Discussion: Despite the well-established AGA guidelines for the use of DEXA screening to prevent bone-related morbidity and mortality, we observed that majority of eligible patients did not receive DEXA screening. Younger age, male gender, and Medicaid insurance were associated with lower practice of DEXA screening.
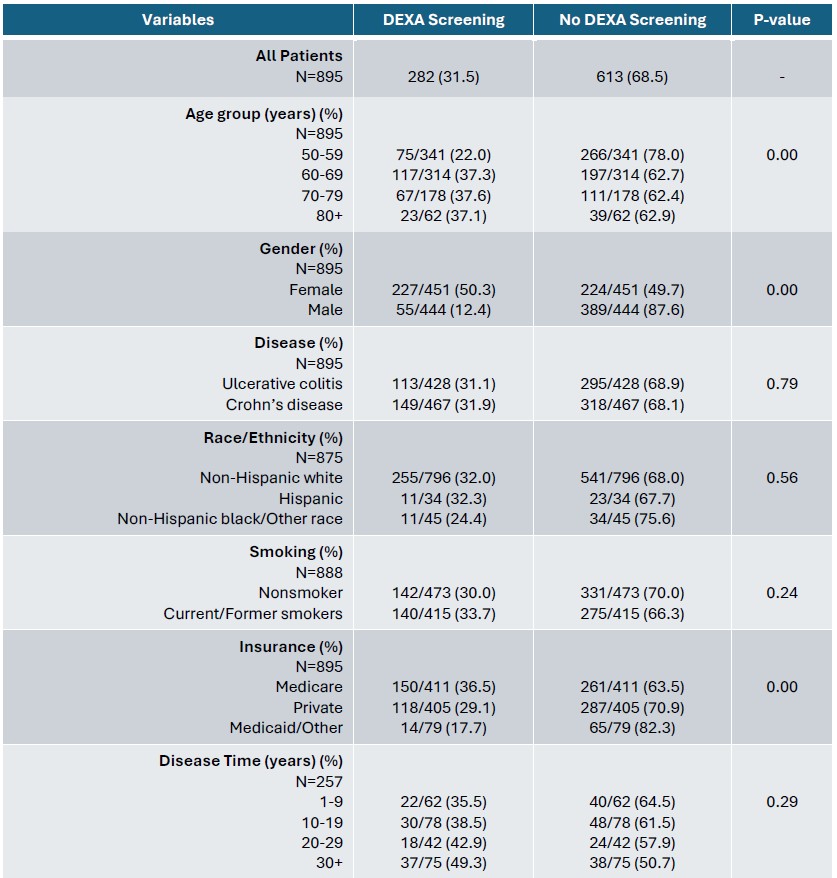
Figure: Table 1. Chi-squared comparison of rates of DEXA screening between demographic covariates and disease time
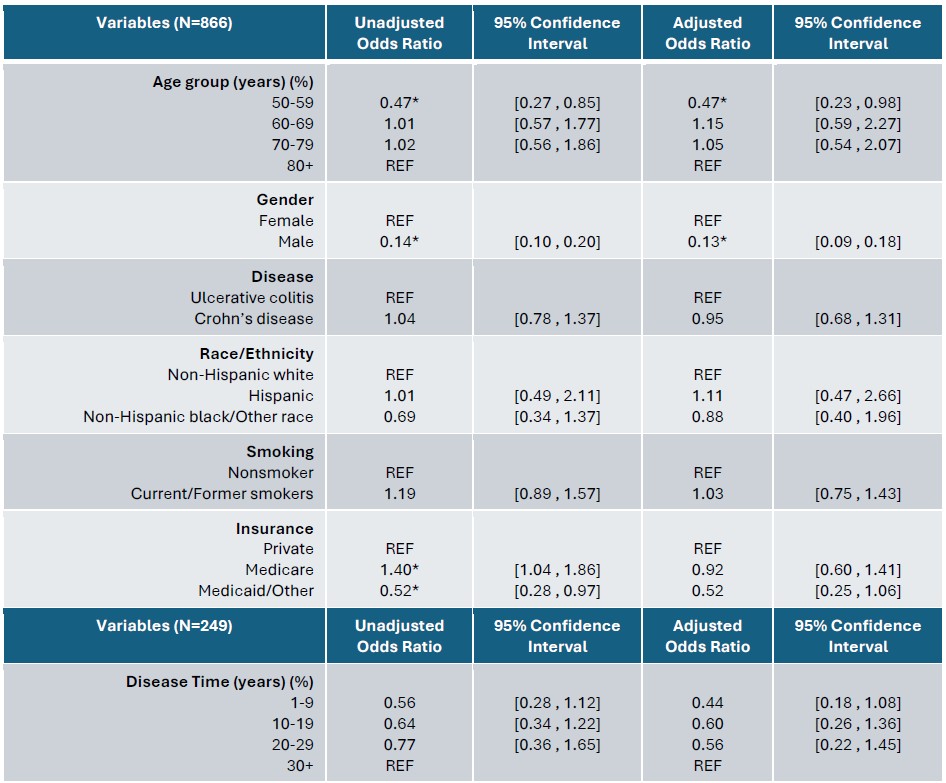
Figure: Table 2. Logistic regression (n=866) of demographic covariates with odds of DEXA screening. Subset model including disease time (n=249). Unadjusted and adjusted demographic covariate odds ratios not reported in subset model. “*” denotes significant odds ratios
Disclosures:
Harris Feldman indicated no relevant financial relationships.
Ahmed El-Sadek indicated no relevant financial relationships.
Xiang Li indicated no relevant financial relationships.
Michael Wang indicated no relevant financial relationships.
Olivia Michaels indicated no relevant financial relationships.
Katherine Mackey indicated no relevant financial relationships.
Abbas Rupawala: Abbvie – Consultant, Speakers Bureau. Pfizer – Consultant. Takeda – Consultant.
Apurv Soni indicated no relevant financial relationships.
Harris Feldman, MD, Ahmed El-Sadek, MD, Xiang Li, MS, Michael Wang, MD, Olivia Michaels, BS, Katherine Mackey, BS, Abbas Rupawala, MD, Apurv Soni, MD. P3346 - Risk Factors for Underutilization of Bone Mineral Deficiency Screenings in an Older Cohort of Patients With Inflammatory Bowel Disease: A Single Center Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
UMass Chan Medical School, Worcester, MA
Introduction: The complex interplay of chronic inflammation, malnutrition, and steroid exposures put patients with inflammatory bowel disease (IBD) at a higher risk for disorders of bone mineral deficiency (BMD) compared to the general population. The American Gastroenterological Association (AGA) recommends DEXA screening for males ≥ 50 years old and postmenopausal women as part of evidence-based health maintenance in IBD management. This study will determine DEXA screening rates in this population and examine risk factors associated with DEXA screening.
Methods: In this single center, retrospective cohort study, electronic medical record (EMR) data were extracted to identify patients with IBD age ≥ 50 years using International Classification of Diseases-10 (ICD-10) codes K50 (Crohn’s disease - CD) and K51 (ulcerative colitis - UC) billed by at least one gastroenterology office visit from study period 1/1/2018-12/31/2024. The primary outcome variable of DEXA screening rate was defined as a DEXA scan result during study period for all patients. EMR charts for a subset of patients were reviewed to generate approximate disease duration. Multivariable logistic regression was used to examine association between risk factors (demographic characteristics and disease-time) associated with risk of underutilization of DEXA screening.
Results: Of 895 IBD patients who met the study criteria, 47.8% had UC and 52.2% had CD. Average age among the analytic sample was 63.8 years (SD: 9.5), 49.6% male, majority were non-Hispanic White (91.0%), nearly half had a smoking history (46.7%), nearly half of the sample (45.9%) had Medicare insurance. Among those patients who had complete information about the onset of disease (n = 257, 28.7%), the average disease duration was 18.0 years (SD: 16.1). Overall, only a third of eligible patients received a DEXA scan screening (n = 282, 31.5%). After adjusting for covariates, age group 50-59 years and male gender were associated with 53.0% (OR 0.47 [0.22 , 0.98]) and 87.1% (OR 0.13 [0.09 , 0.18]) lower odds of DEXA screening, respectively. Medicaid insurance was associated with 47.6% (OR 0.52 [0.28 , 0.97]) lower odds, though this was only seen in the unadjusted model.
Discussion: Despite the well-established AGA guidelines for the use of DEXA screening to prevent bone-related morbidity and mortality, we observed that majority of eligible patients did not receive DEXA screening. Younger age, male gender, and Medicaid insurance were associated with lower practice of DEXA screening.
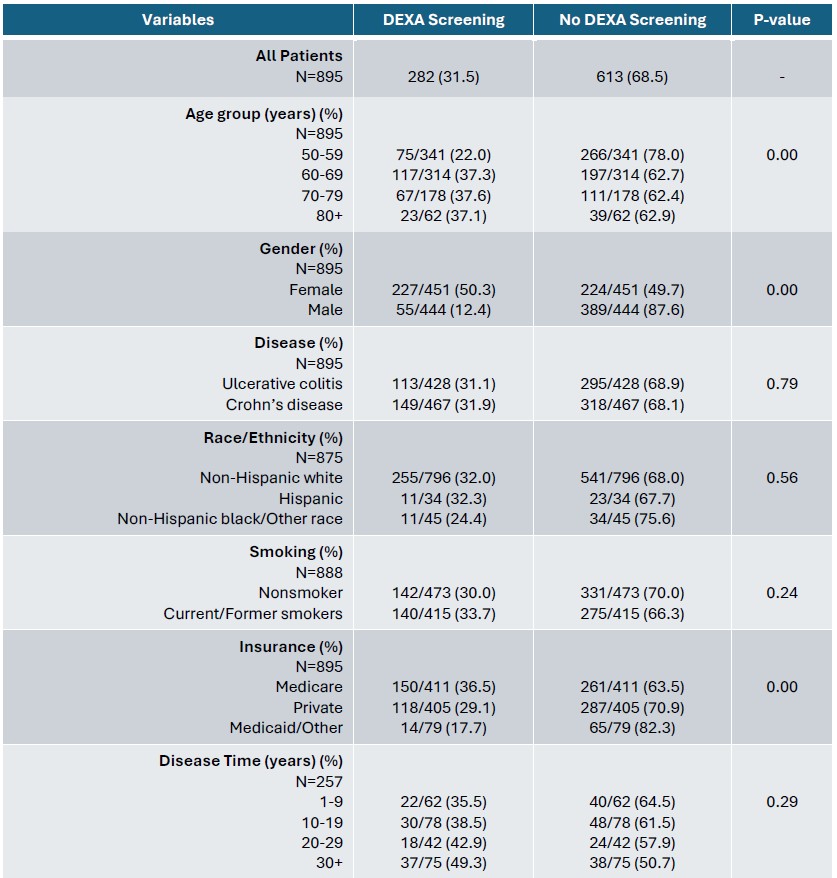
Figure: Table 1. Chi-squared comparison of rates of DEXA screening between demographic covariates and disease time
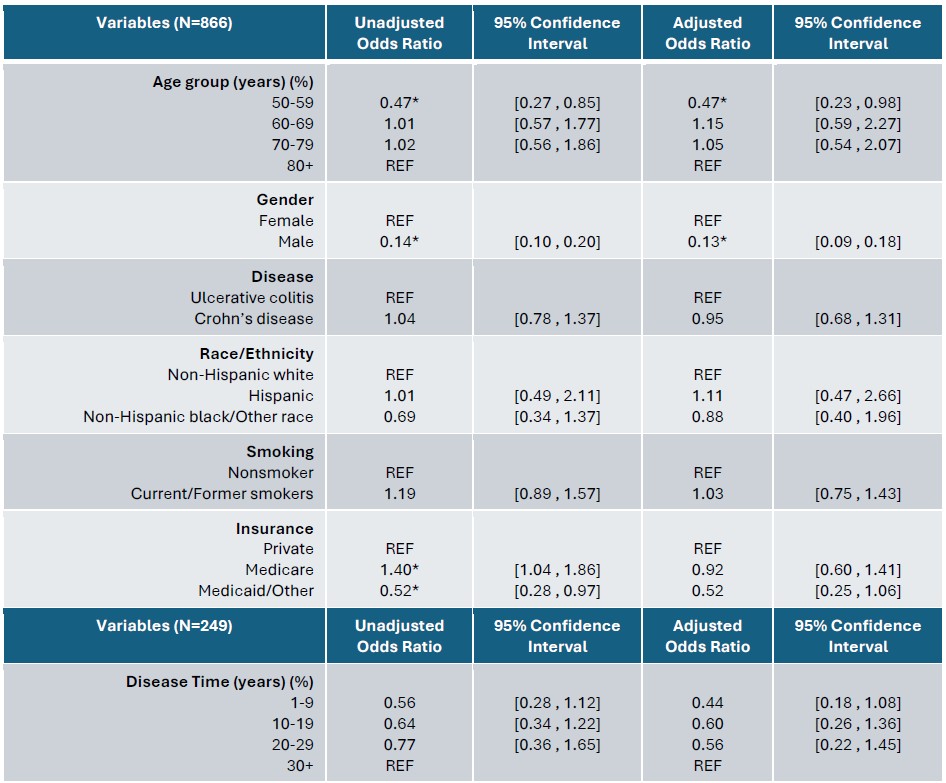
Figure: Table 2. Logistic regression (n=866) of demographic covariates with odds of DEXA screening. Subset model including disease time (n=249). Unadjusted and adjusted demographic covariate odds ratios not reported in subset model. “*” denotes significant odds ratios
Disclosures:
Harris Feldman indicated no relevant financial relationships.
Ahmed El-Sadek indicated no relevant financial relationships.
Xiang Li indicated no relevant financial relationships.
Michael Wang indicated no relevant financial relationships.
Olivia Michaels indicated no relevant financial relationships.
Katherine Mackey indicated no relevant financial relationships.
Abbas Rupawala: Abbvie – Consultant, Speakers Bureau. Pfizer – Consultant. Takeda – Consultant.
Apurv Soni indicated no relevant financial relationships.
Harris Feldman, MD, Ahmed El-Sadek, MD, Xiang Li, MS, Michael Wang, MD, Olivia Michaels, BS, Katherine Mackey, BS, Abbas Rupawala, MD, Apurv Soni, MD. P3346 - Risk Factors for Underutilization of Bone Mineral Deficiency Screenings in an Older Cohort of Patients With Inflammatory Bowel Disease: A Single Center Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
