Monday Poster Session
Category: Infections and Microbiome
P3418 - Clostridioides difficile Infection Increases the Risk of Belated Microscopic Colitis Development: A 20-Year Propensity-Matched, Multicenter, Cohort Study Across the United States
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Clive J. Miranda, DO, MSc
CHI Health Creighton University Medical Center
Omaha, NE
Presenting Author(s)
Clive J. Miranda, DO, MSc1, Anmol Singh, MBBS2, Andrew Ford, MD3, Arjun Chatterjee, MD4, Marcellus A. Singh, MD1, Abdallah Kobeissy, MD, MPH5, Jessica R. Philpott, MD, PhD, FACG4, Brian B. Baggott, MD4, Ahmed N. Al-Chalabi, MD, MSc, MPH1
1CHI Health Creighton University Medical Center, Omaha, NE; 2Tristar Centennial Medical Center, Nashville, TN, Nashville, TN; 3Case Western Reserve University / MetroHealth, Cleveland, OH; 4Cleveland Clinic Foundation, Cleveland, OH; 5The University of Toledo, Toledo, OH
Introduction: Clostridium difficile is an anaerobic gram-positive bacillus that is a leading cause of health-associated infectious diarrhea, primarily due to antibiotic-induced disruption of the normal gut microbiota. The bacterium’s pathogenicity is mediated by the production of two major exotoxins, leading to cytoskeletal disruption, loss of epithelial barrier function, cell death, and a devastating inflammatory response. Scattered case-control studies have recently noted that patients with Clostridium difficile infection (CDI) have increased odds of developing microscopic colitis (MC), a chronic inflammatory disease characterized by watery diarrhea. To date, there is no nationwide or global study on this association.
Methods: We conducted a retrospective nationwide cohort study on adults ≥50 years using the TriNetX database from January 2004 to May 2025. Two patient cohorts were generated via ICD-10 coding – one with a diagnosis of enterocolitis due to CDI [A04.07] and the other with healthy patients with no CDI history [Z00.00]. Evaluation for MC and its subtypes – lymphocytic colitis (LC) and collagenous colitis (CC) – within each cohort were then assessed, and 1:1 propensity score matching was completed for age, sex, race, medications, and autoimmune conditions to account for any confounding variables. Risk ratios with 95% confidence intervals (CI) were reported.
Results: Our cohorts consisted of 287,128 patients each after 1:1 propensity score matching. The mean age was 68.2 years +/- 12.6 with a demographic breakdown of 55% female, 75% White, and 11% Black. The median follow-up time to MC diagnosis was 671 days for CDI-positive patients and 1427 days for CDI-negative patients. Compared with their noninfected counterparts, patients with CDI had a 1.9 relative risk of developing MC [95% CI 1.69-2.02, p< 0.001]. Sub-stratifying this further, CDI-positive patients had a 2-fold relative risk of developing CC [95% CI 1.71-2.29, p< 0.001] and a 1.8 relative risk of developing LC [95% CI 1.51-1.94, p< 0.001] as compared to CDI-negative patients.
Discussion: This is the first nationwide cohort study investigating the relationship between MC and CDI. MC development is increased ~2-fold after CDI in patients ≥50 years, even occurring years after the index infection. Patients with a prior CDI history presenting with chronic watery diarrhea should raise one’s suspicion for possible MC, as timely diagnosis and treatment can greatly improve quality of life and reduce unnecessary healthcare expenditures.
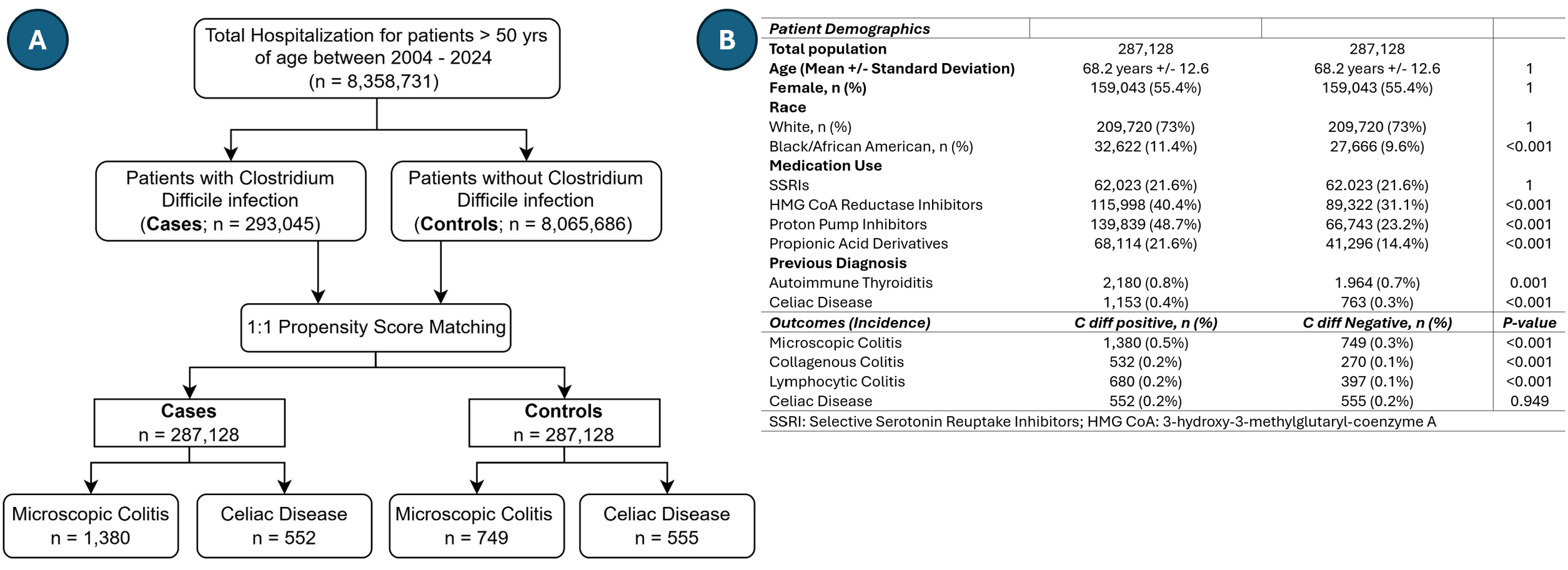
Figure: A: Inclusion flow diagram for the nationwide retrospective cohort study
B: Patient demographics after 1:1 propensity score matching
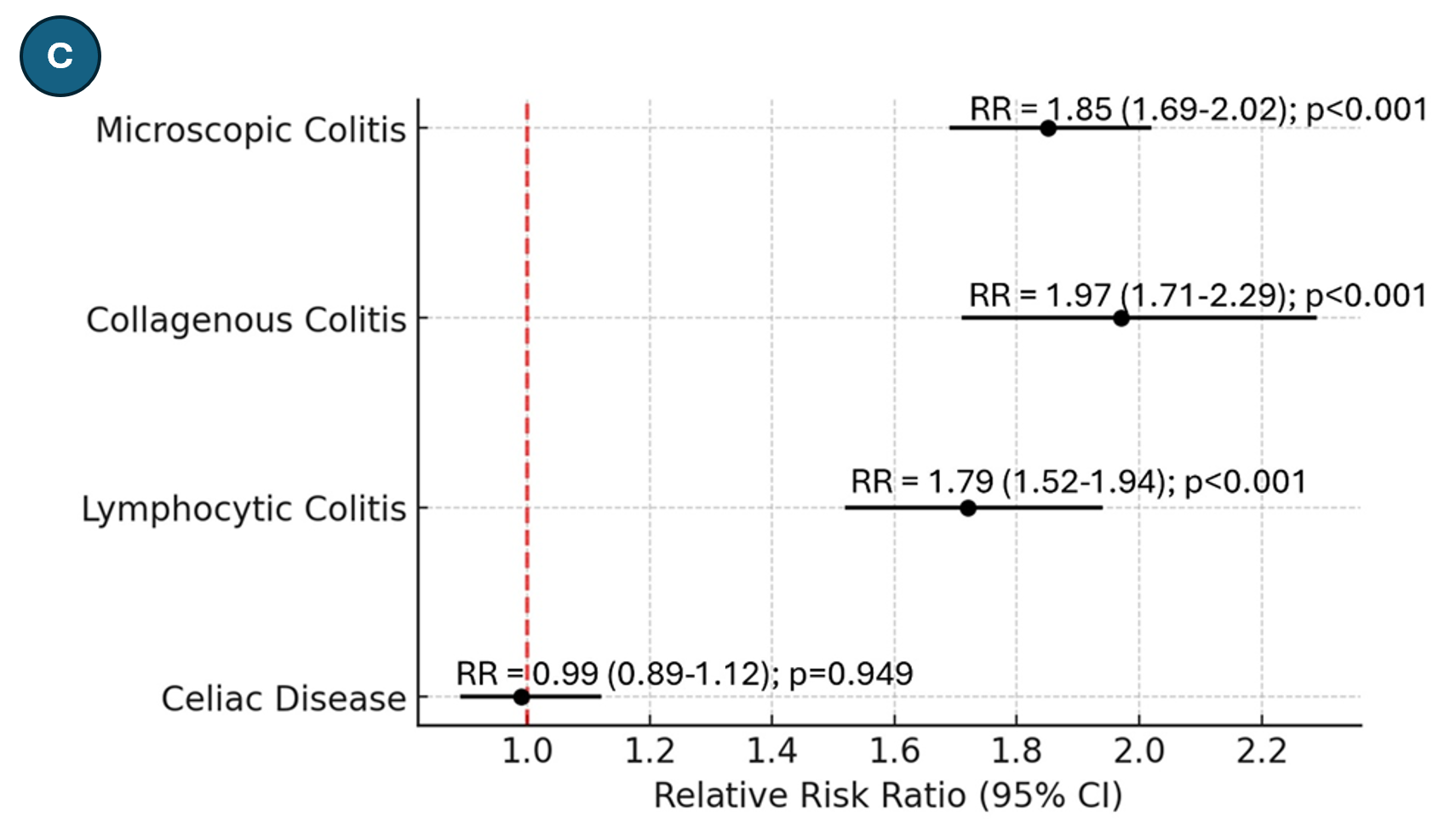
Figure: C: Relative risk of development of microscopic colitis (and its subtypes) and celiac disease in patients with a history of Clostridium difficile infection compared to patients without Clostridium difficile infection. RR, Relative Risk
Disclosures:
Clive Miranda indicated no relevant financial relationships.
Anmol Singh indicated no relevant financial relationships.
Andrew Ford indicated no relevant financial relationships.
Arjun Chatterjee indicated no relevant financial relationships.
Marcellus Singh indicated no relevant financial relationships.
Abdallah Kobeissy indicated no relevant financial relationships.
Jessica Philpott: Abbvie – Speakers Bureau.
Brian Baggott indicated no relevant financial relationships.
Ahmed Al-Chalabi indicated no relevant financial relationships.
Clive J. Miranda, DO, MSc1, Anmol Singh, MBBS2, Andrew Ford, MD3, Arjun Chatterjee, MD4, Marcellus A. Singh, MD1, Abdallah Kobeissy, MD, MPH5, Jessica R. Philpott, MD, PhD, FACG4, Brian B. Baggott, MD4, Ahmed N. Al-Chalabi, MD, MSc, MPH1. P3418 - <i>Clostridioides difficile</i> Infection Increases the Risk of Belated Microscopic Colitis Development: A 20-Year Propensity-Matched, Multicenter, Cohort Study Across the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1CHI Health Creighton University Medical Center, Omaha, NE; 2Tristar Centennial Medical Center, Nashville, TN, Nashville, TN; 3Case Western Reserve University / MetroHealth, Cleveland, OH; 4Cleveland Clinic Foundation, Cleveland, OH; 5The University of Toledo, Toledo, OH
Introduction: Clostridium difficile is an anaerobic gram-positive bacillus that is a leading cause of health-associated infectious diarrhea, primarily due to antibiotic-induced disruption of the normal gut microbiota. The bacterium’s pathogenicity is mediated by the production of two major exotoxins, leading to cytoskeletal disruption, loss of epithelial barrier function, cell death, and a devastating inflammatory response. Scattered case-control studies have recently noted that patients with Clostridium difficile infection (CDI) have increased odds of developing microscopic colitis (MC), a chronic inflammatory disease characterized by watery diarrhea. To date, there is no nationwide or global study on this association.
Methods: We conducted a retrospective nationwide cohort study on adults ≥50 years using the TriNetX database from January 2004 to May 2025. Two patient cohorts were generated via ICD-10 coding – one with a diagnosis of enterocolitis due to CDI [A04.07] and the other with healthy patients with no CDI history [Z00.00]. Evaluation for MC and its subtypes – lymphocytic colitis (LC) and collagenous colitis (CC) – within each cohort were then assessed, and 1:1 propensity score matching was completed for age, sex, race, medications, and autoimmune conditions to account for any confounding variables. Risk ratios with 95% confidence intervals (CI) were reported.
Results: Our cohorts consisted of 287,128 patients each after 1:1 propensity score matching. The mean age was 68.2 years +/- 12.6 with a demographic breakdown of 55% female, 75% White, and 11% Black. The median follow-up time to MC diagnosis was 671 days for CDI-positive patients and 1427 days for CDI-negative patients. Compared with their noninfected counterparts, patients with CDI had a 1.9 relative risk of developing MC [95% CI 1.69-2.02, p< 0.001]. Sub-stratifying this further, CDI-positive patients had a 2-fold relative risk of developing CC [95% CI 1.71-2.29, p< 0.001] and a 1.8 relative risk of developing LC [95% CI 1.51-1.94, p< 0.001] as compared to CDI-negative patients.
Discussion: This is the first nationwide cohort study investigating the relationship between MC and CDI. MC development is increased ~2-fold after CDI in patients ≥50 years, even occurring years after the index infection. Patients with a prior CDI history presenting with chronic watery diarrhea should raise one’s suspicion for possible MC, as timely diagnosis and treatment can greatly improve quality of life and reduce unnecessary healthcare expenditures.
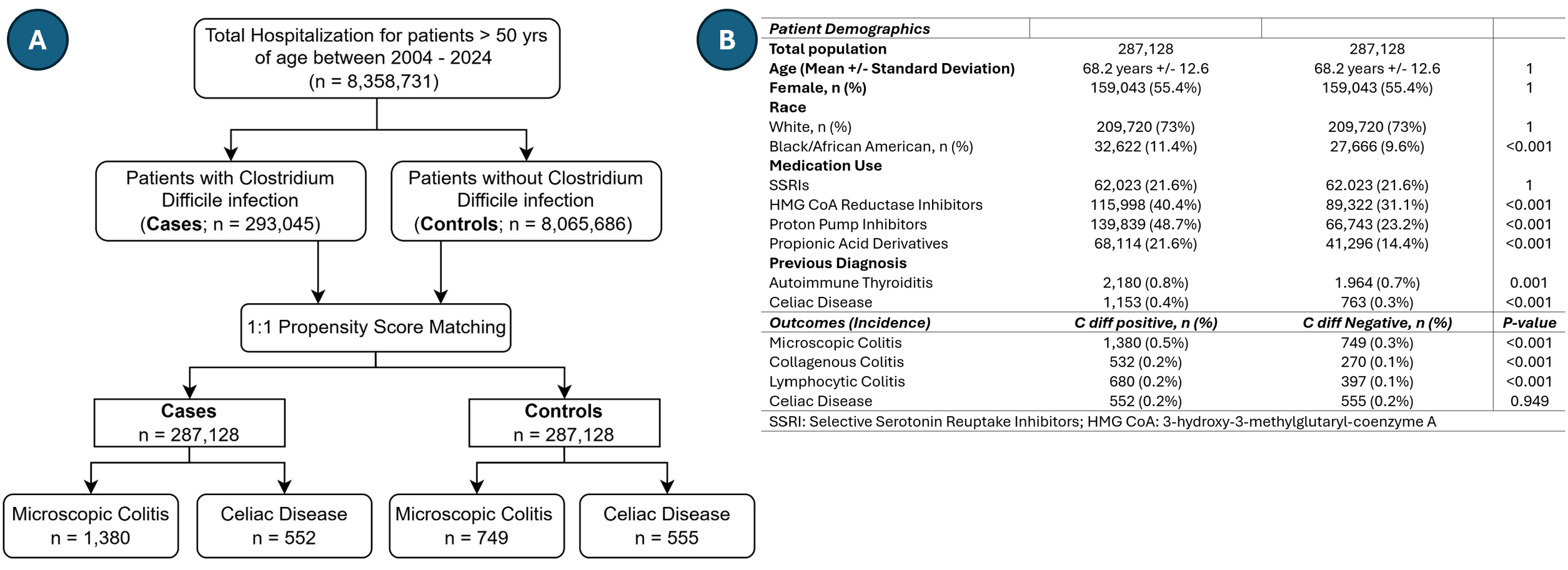
Figure: A: Inclusion flow diagram for the nationwide retrospective cohort study
B: Patient demographics after 1:1 propensity score matching
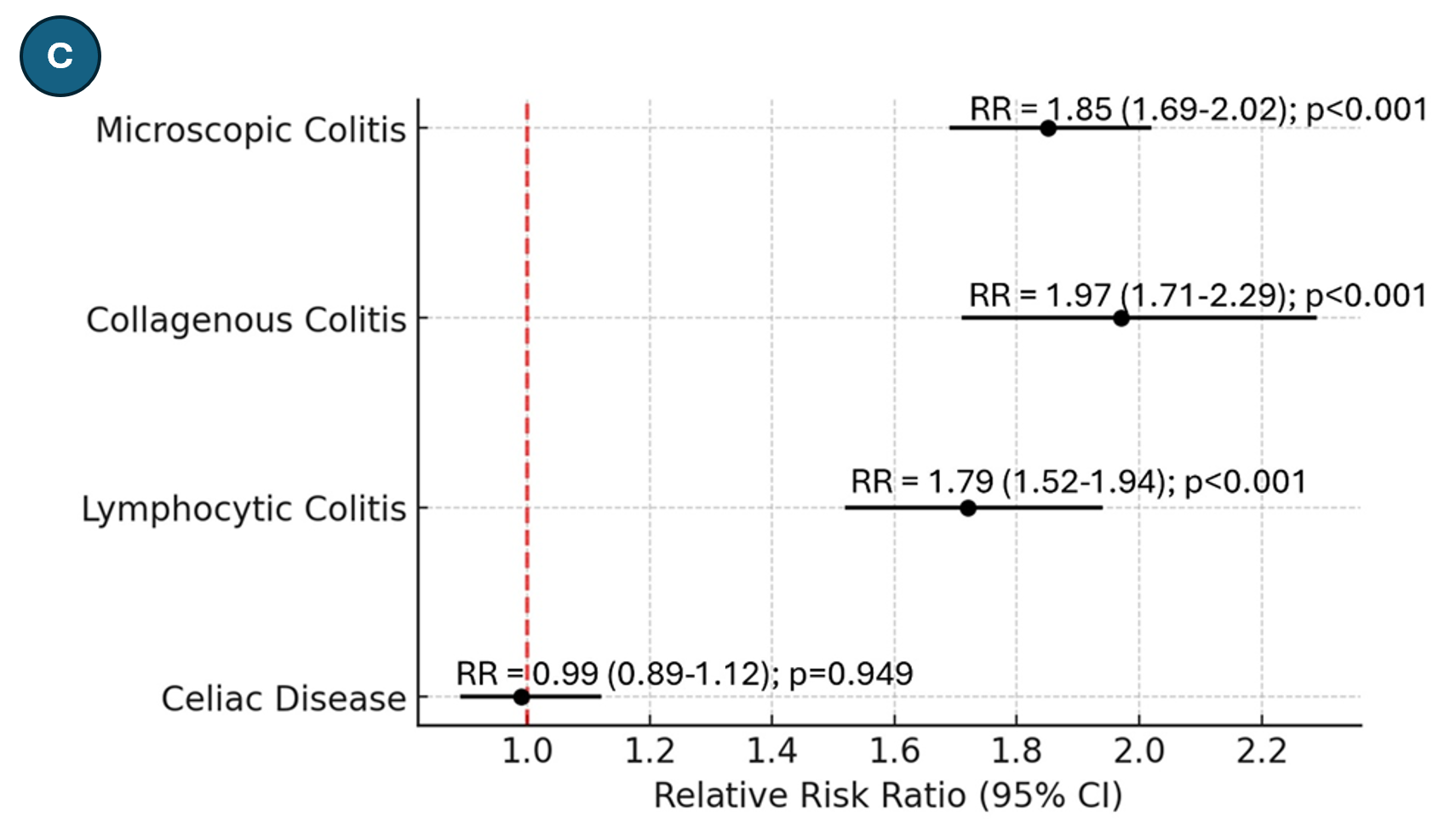
Figure: C: Relative risk of development of microscopic colitis (and its subtypes) and celiac disease in patients with a history of Clostridium difficile infection compared to patients without Clostridium difficile infection. RR, Relative Risk
Disclosures:
Clive Miranda indicated no relevant financial relationships.
Anmol Singh indicated no relevant financial relationships.
Andrew Ford indicated no relevant financial relationships.
Arjun Chatterjee indicated no relevant financial relationships.
Marcellus Singh indicated no relevant financial relationships.
Abdallah Kobeissy indicated no relevant financial relationships.
Jessica Philpott: Abbvie – Speakers Bureau.
Brian Baggott indicated no relevant financial relationships.
Ahmed Al-Chalabi indicated no relevant financial relationships.
Clive J. Miranda, DO, MSc1, Anmol Singh, MBBS2, Andrew Ford, MD3, Arjun Chatterjee, MD4, Marcellus A. Singh, MD1, Abdallah Kobeissy, MD, MPH5, Jessica R. Philpott, MD, PhD, FACG4, Brian B. Baggott, MD4, Ahmed N. Al-Chalabi, MD, MSc, MPH1. P3418 - <i>Clostridioides difficile</i> Infection Increases the Risk of Belated Microscopic Colitis Development: A 20-Year Propensity-Matched, Multicenter, Cohort Study Across the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
