Monday Poster Session
Category: IBD
Ulcerative Colitis and ILD Complicated by Recurrent Enteric Infections: A Case of <i>C. difficile</i> and <i>C. perfringens</i> Bacteremia
P3413 - Ulcerative Colitis and ILD Complicated by Recurrent Enteric Infections: A Case of C. difficile and C. perfringens Bacteremia
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ahmad Zain, MBBS (he/him/his)
Parkview Medical Center
Pueblo, CO
Presenting Author(s)
Ahmad Zain, MBBS1, Amil Shah, DO1, Hammad Qadri, DO2, Fatima Ashfaq, MBBS3, Syed Rafay H zaidi, MBBS1, Muhammad Sohaib, MBBS1, Bryant Javier, DO1, Mustafa Nayeem, MD1, Shan Tandon, MD1, Zoha Shahzad, MD4
1Parkview Medical Center, Pueblo, CO; 2United Health Services, Wilson Medical Center, Vestal, NY; 3Nishtar Medical University, Multan, Punjab, Pakistan; 4One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY
Introduction: While extraintestinal manifestations like arthritis, asthma, psoriasis, and pericarditis are well-documented in inflammatory bowel disease (IBD), pulmonary involvement remains a relatively rare complication. However, emerging studies suggest that 28-58% of patients with IBD may have related pulmonary manifestations. This suggests an intricate interplay between the gut and lungs, often referred to as the gut-lung axis, where shared immune and microbiotic pathways may contribute to both gastrointestinal and respiratory complications.
Case Description/
Methods: A 65-year-old male with a medical history of moderate ulcerative colitis (UC), interstitial lung disease (ILD), and COPD presented with worsening chronic diarrhea and progressive shortness of breath. He had been recently hospitalized for a UC flare, during which colonoscopy revealed pancolitis without dysplasia and segmental severe inflammation in the sigmoid and descending colon and was discharged on oral mesalamine and budesonide.Although his bowel symptoms initially improved, he relapsed experiencing 5–6 watery to profuse bowel movements per day.He reported fatigue and chills, but denied fever, abdominal,chest pain, or urinary symptoms. In the ED, a CT abdomen and pelvis (CTAP) was performed, and stool testing returned positive for Clostridium difficile. He was treated with a full course of oral vancomycin and discharged. However, his symptoms worsened, now with increased shortness of breath and persistent diarrhea accompanied by hypoxia, requiring 2 L/min of supplemental oxygen. A CTA of the chest revealed honeycombing and fibrotic changes consistent with underlying ILD. The autoimmune panel showed positive ANA but no other specific markers identified. Blood cultures later revealed Clostridium perfringens bacteremia, suspected to be secondary to bacterial translocation across compromised colonic mucosa. The patient was treated with IV vancomycin, IV corticosteroids, and metronidazole, and was admitted for further pulmonary and gastrointestinal evaluation.
Discussion: Here, we report a rare case of ILD in a patient with UC, a manifestation that is often overlooked. Early recognition and intervention are crucial to prevent long-term morbidity. This case highlights the critical need for systematic ILD screening protocols in the IBD patient population to facilitate early detection and management.
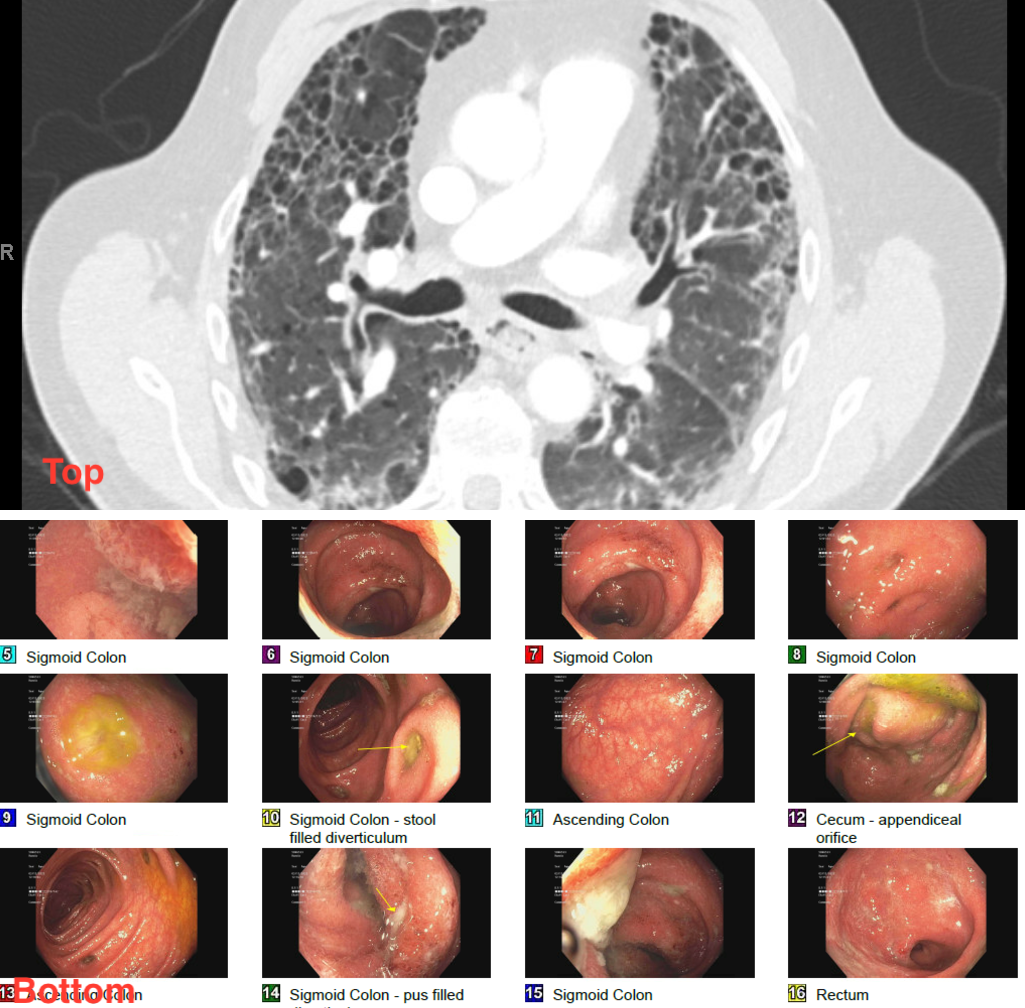
Figure: Top: CT scan showing structural lung disease
Bottom: Images of colonoscope showing pan-colitis

Figure: A= chronic proctitis B= crypt abscess in rectum C= crypt abscess in Caecum = D= Cryptitis in caecum
Disclosures:
Ahmad Zain indicated no relevant financial relationships.
Amil Shah indicated no relevant financial relationships.
Hammad Qadri indicated no relevant financial relationships.
Fatima Ashfaq indicated no relevant financial relationships.
Syed Rafay H zaidi indicated no relevant financial relationships.
Muhammad Sohaib indicated no relevant financial relationships.
Bryant Javier indicated no relevant financial relationships.
Mustafa Nayeem indicated no relevant financial relationships.
Shan Tandon indicated no relevant financial relationships.
Zoha Shahzad indicated no relevant financial relationships.
Ahmad Zain, MBBS1, Amil Shah, DO1, Hammad Qadri, DO2, Fatima Ashfaq, MBBS3, Syed Rafay H zaidi, MBBS1, Muhammad Sohaib, MBBS1, Bryant Javier, DO1, Mustafa Nayeem, MD1, Shan Tandon, MD1, Zoha Shahzad, MD4. P3413 - Ulcerative Colitis and ILD Complicated by Recurrent Enteric Infections: A Case of <i>C. difficile</i> and <i>C. perfringens</i> Bacteremia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Parkview Medical Center, Pueblo, CO; 2United Health Services, Wilson Medical Center, Vestal, NY; 3Nishtar Medical University, Multan, Punjab, Pakistan; 4One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY
Introduction: While extraintestinal manifestations like arthritis, asthma, psoriasis, and pericarditis are well-documented in inflammatory bowel disease (IBD), pulmonary involvement remains a relatively rare complication. However, emerging studies suggest that 28-58% of patients with IBD may have related pulmonary manifestations. This suggests an intricate interplay between the gut and lungs, often referred to as the gut-lung axis, where shared immune and microbiotic pathways may contribute to both gastrointestinal and respiratory complications.
Case Description/
Methods: A 65-year-old male with a medical history of moderate ulcerative colitis (UC), interstitial lung disease (ILD), and COPD presented with worsening chronic diarrhea and progressive shortness of breath. He had been recently hospitalized for a UC flare, during which colonoscopy revealed pancolitis without dysplasia and segmental severe inflammation in the sigmoid and descending colon and was discharged on oral mesalamine and budesonide.Although his bowel symptoms initially improved, he relapsed experiencing 5–6 watery to profuse bowel movements per day.He reported fatigue and chills, but denied fever, abdominal,chest pain, or urinary symptoms. In the ED, a CT abdomen and pelvis (CTAP) was performed, and stool testing returned positive for Clostridium difficile. He was treated with a full course of oral vancomycin and discharged. However, his symptoms worsened, now with increased shortness of breath and persistent diarrhea accompanied by hypoxia, requiring 2 L/min of supplemental oxygen. A CTA of the chest revealed honeycombing and fibrotic changes consistent with underlying ILD. The autoimmune panel showed positive ANA but no other specific markers identified. Blood cultures later revealed Clostridium perfringens bacteremia, suspected to be secondary to bacterial translocation across compromised colonic mucosa. The patient was treated with IV vancomycin, IV corticosteroids, and metronidazole, and was admitted for further pulmonary and gastrointestinal evaluation.
Discussion: Here, we report a rare case of ILD in a patient with UC, a manifestation that is often overlooked. Early recognition and intervention are crucial to prevent long-term morbidity. This case highlights the critical need for systematic ILD screening protocols in the IBD patient population to facilitate early detection and management.
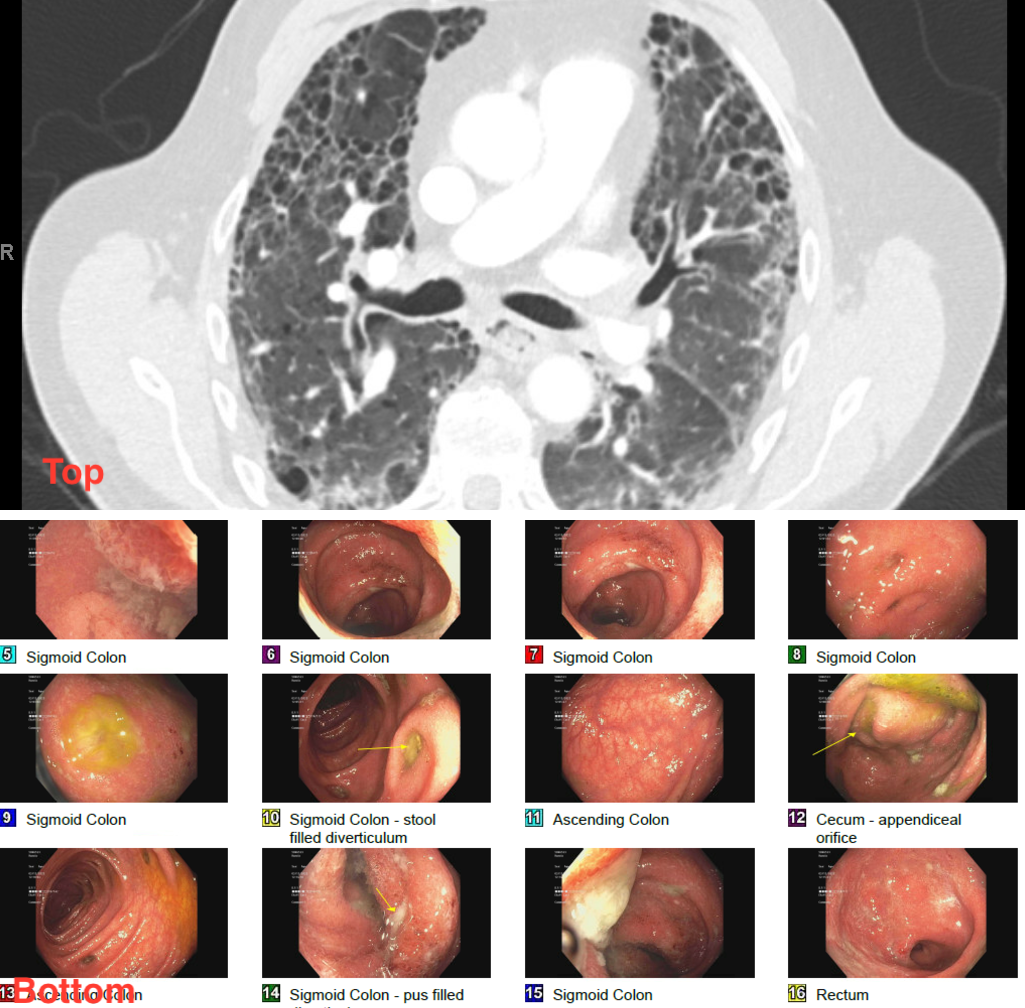
Figure: Top: CT scan showing structural lung disease
Bottom: Images of colonoscope showing pan-colitis

Figure: A= chronic proctitis B= crypt abscess in rectum C= crypt abscess in Caecum = D= Cryptitis in caecum
Disclosures:
Ahmad Zain indicated no relevant financial relationships.
Amil Shah indicated no relevant financial relationships.
Hammad Qadri indicated no relevant financial relationships.
Fatima Ashfaq indicated no relevant financial relationships.
Syed Rafay H zaidi indicated no relevant financial relationships.
Muhammad Sohaib indicated no relevant financial relationships.
Bryant Javier indicated no relevant financial relationships.
Mustafa Nayeem indicated no relevant financial relationships.
Shan Tandon indicated no relevant financial relationships.
Zoha Shahzad indicated no relevant financial relationships.
Ahmad Zain, MBBS1, Amil Shah, DO1, Hammad Qadri, DO2, Fatima Ashfaq, MBBS3, Syed Rafay H zaidi, MBBS1, Muhammad Sohaib, MBBS1, Bryant Javier, DO1, Mustafa Nayeem, MD1, Shan Tandon, MD1, Zoha Shahzad, MD4. P3413 - Ulcerative Colitis and ILD Complicated by Recurrent Enteric Infections: A Case of <i>C. difficile</i> and <i>C. perfringens</i> Bacteremia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
