Monday Poster Session
Category: IBD
P3409 - The Unseen Fire: Perianal Fistulizing Crohn's Disease in the Absence of GI Symptoms
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- PR
Patricia Rivera, MD (she/her/hers)
VA Caribbean Healthcare System
San Juan, PR
Presenting Author(s)
Patricia Rivera-Cariño, MD, Orlando Rodriguez-Amador, MD, Jose Martin-Ortiz, MD, FACG
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Crohn’s disease (CD) is a chronic inflammatory disorder that can affect any part of the gastrointestinal (GI) tract. While perianal fistulizing disease is a known manifestation, isolated perianal involvement as an initial presentation, particularly in adults without GI symptoms is uncommon and often portends a more severe disease course with future luminal progression. We present the case of a male that debuted with isolated perianal disease (IPD) without other GI symptoms followed by ileal and microscopic colonic involvement.
Case Description/
Methods: A 50-year-old man with history of constipation, recurrent perianal abscesses and prior fistula managed with incision, drainage, and seton placement, who presented to the ED with perianal pain, fever, and chills for 2 days. Examination revealed a draining perianal incision. He denied diarrheas, rectal bleeding, nocturnal awakening for defecation, unintentional weight loss, abdominal pain, oral ulcers, pain in his articulations, rashes, or family history of autoimmune diseases. A recent high-quality colonoscopy with biopsy and without ileal intubation was unremarkable. Physical exam showed a benign abdomen and a left anal border incision of 0.5 inch at 5 o’clock with serous fluid discharge. Pelvic MRI showed a trans and an inter-sphincteric anal fistulas without abscesses. Given the recurrent nature of his perianal disease and absence of luminal findings on prior colonoscopy, capsule endoscopy was pursued. This revealed moderate ileal erosions, which were subsequently confirmed on follow-up colonoscopy. Although the colonic mucosa appeared normal, random biopsies showed patchy acute and chronic colitis with non-necrotizing granulomas; findings consistent with CD (Figure 1). Anti-TNF therapy was initiated.
Discussion: IPD is a rare presentation of CD in adults, comprising approximately 4-5% of cases. It more commonly affects younger patients and may be associated with more severe disease outcomes. This case highlights the need for a high index of suspicion for CD in patients presenting solely with perianal disease, even in the absence of luminal symptoms. Capsule endoscopy proved pivotal in this case for diagnosis, particularly because early and isolated lesions may be missed by other modalities. Moreover, this case reinforces the importance of obtaining biopsies from endoscopically normal mucosa, as microscopic disease may be the only diagnostic clue in early or patchy presentation of CD.
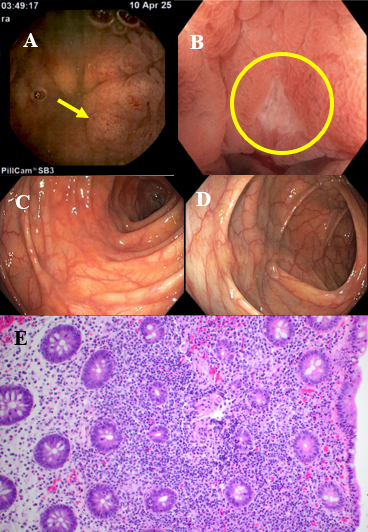
Figure: Figure 1: Capsule endoscopy (A) showing erosions at the terminal ileum (yellow arrow); (B) colonoscopy showing aphthous ulcer in the terminal ileum (yellow circle). Ascending (C) colon and hepatic flexure (D) normal mucosa; Histology (E) showing acute and chronic colitis with small non-necrotizing granuloma.
Disclosures:
Patricia Rivera-Cariño indicated no relevant financial relationships.
Orlando Rodriguez-Amador indicated no relevant financial relationships.
Jose Martin-Ortiz indicated no relevant financial relationships.
Patricia Rivera-Cariño, MD, Orlando Rodriguez-Amador, MD, Jose Martin-Ortiz, MD, FACG. P3409 - The Unseen Fire: Perianal Fistulizing Crohn's Disease in the Absence of GI Symptoms, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Crohn’s disease (CD) is a chronic inflammatory disorder that can affect any part of the gastrointestinal (GI) tract. While perianal fistulizing disease is a known manifestation, isolated perianal involvement as an initial presentation, particularly in adults without GI symptoms is uncommon and often portends a more severe disease course with future luminal progression. We present the case of a male that debuted with isolated perianal disease (IPD) without other GI symptoms followed by ileal and microscopic colonic involvement.
Case Description/
Methods: A 50-year-old man with history of constipation, recurrent perianal abscesses and prior fistula managed with incision, drainage, and seton placement, who presented to the ED with perianal pain, fever, and chills for 2 days. Examination revealed a draining perianal incision. He denied diarrheas, rectal bleeding, nocturnal awakening for defecation, unintentional weight loss, abdominal pain, oral ulcers, pain in his articulations, rashes, or family history of autoimmune diseases. A recent high-quality colonoscopy with biopsy and without ileal intubation was unremarkable. Physical exam showed a benign abdomen and a left anal border incision of 0.5 inch at 5 o’clock with serous fluid discharge. Pelvic MRI showed a trans and an inter-sphincteric anal fistulas without abscesses. Given the recurrent nature of his perianal disease and absence of luminal findings on prior colonoscopy, capsule endoscopy was pursued. This revealed moderate ileal erosions, which were subsequently confirmed on follow-up colonoscopy. Although the colonic mucosa appeared normal, random biopsies showed patchy acute and chronic colitis with non-necrotizing granulomas; findings consistent with CD (Figure 1). Anti-TNF therapy was initiated.
Discussion: IPD is a rare presentation of CD in adults, comprising approximately 4-5% of cases. It more commonly affects younger patients and may be associated with more severe disease outcomes. This case highlights the need for a high index of suspicion for CD in patients presenting solely with perianal disease, even in the absence of luminal symptoms. Capsule endoscopy proved pivotal in this case for diagnosis, particularly because early and isolated lesions may be missed by other modalities. Moreover, this case reinforces the importance of obtaining biopsies from endoscopically normal mucosa, as microscopic disease may be the only diagnostic clue in early or patchy presentation of CD.
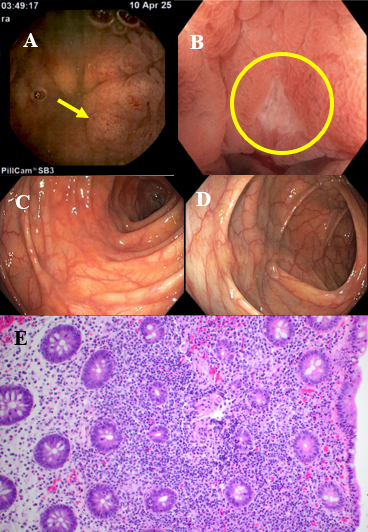
Figure: Figure 1: Capsule endoscopy (A) showing erosions at the terminal ileum (yellow arrow); (B) colonoscopy showing aphthous ulcer in the terminal ileum (yellow circle). Ascending (C) colon and hepatic flexure (D) normal mucosa; Histology (E) showing acute and chronic colitis with small non-necrotizing granuloma.
Disclosures:
Patricia Rivera-Cariño indicated no relevant financial relationships.
Orlando Rodriguez-Amador indicated no relevant financial relationships.
Jose Martin-Ortiz indicated no relevant financial relationships.
Patricia Rivera-Cariño, MD, Orlando Rodriguez-Amador, MD, Jose Martin-Ortiz, MD, FACG. P3409 - The Unseen Fire: Perianal Fistulizing Crohn's Disease in the Absence of GI Symptoms, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
