Monday Poster Session
Category: IBD
P3405 - Atypical Presentation of Crohn’s Disease Mimicking Segmental Colitis Associated with Diverticulosis in a 76-Year-Old Woman Progressing to Fulminant Pancolitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Muzzafar Haque, MD (he/him/his)
University of Saskatchewan
Regina, SK, Canada
Presenting Author(s)
Muzzafar Haque, MD1, Sanchit Bhasin, MD01, Sunil Samnani, MBBS2
1University of Saskatchewan, Regina, SK, Canada; 2McMaster University, Hamilton, ON, Canada
Introduction: Segmental colitis associated with diverticulosis (SCAD) is a rare entity characterized by chronic inflammation in the inter diverticular mucosa, often mimicking inflammatory bowel disease (IBD). We report an atypical case of a patient diagnosed with SCAD based on endoscopic findings, who progressed to fulminant pancolitis over 14 months requiring subtotal colectomy. Histopathology later confirmed Crohn’s disease (CD), highlighting diagnostic challenges in distinguishing SCAD from IBD.
Case Description/
Methods: A 76-year-old woman presented to the emergency department in March 2021 with severe abdominal pain, hematochezia, and weight loss. A computed tomography (CT) scan revealed partial large bowel obstruction and a flexible sigmoidoscopy demonstrating inflammation in the distal and sigmoid colon, consistent with diverticulitis. She responded to antibiotics and was discharged within a week. One month later, persistent rectal bleeding and lower abdominal pain prompted outpatient follow-up with a gastroenterologist. A repeat colonoscopy revealed inflammation confined to the sigmoid colon with diverticulosis, macroscopically consistent with SCAD. She was treated for a SCAD flare with antibiotics and 5-ASA. In April 2022, a follow-up colonoscopy showed moderately severe sigmoid inflammation, with normal mucosa proximal to the cecum. Biopsies revealed moderate to severe active chronic colitis with cryptitis. In May 2022, she re-presented with worsening abdominal pain and hematochezia. A CT scan revealed pancolitis with pericolic stranding. She had an elevation in CRP, low hemoglobin and albumin. Repeat colonoscopy revealed severe pancolitis. Histopathology now showed transmural inflammation with deep fissures extending into serosal adipose tissue favoring CD. Due to refractory symptoms, she underwent subtotal colectomy with end-ileostomy instead of advanced therapies. Postoperatively, she recovered well, with normalization of CRP and albumin, and was discharged within weeks.
Discussion: Clinicians must maintain a high index of suspicion for IBD in SCAD patients with refractory symptoms, as endoscopic and histologic overlap leading to misdiagnosis. Repeat colonoscopy with biopsies is critical to re-evaluate the diagnosis. Third, the potential progression of SCAD to IBD warrants further research to clarify whether SCAD is a distinct entity or an early manifestation of IBD in some patients. Differential diagnoses, including UC, ischemic colitis, and infectious colitis, should be systematically excluded.
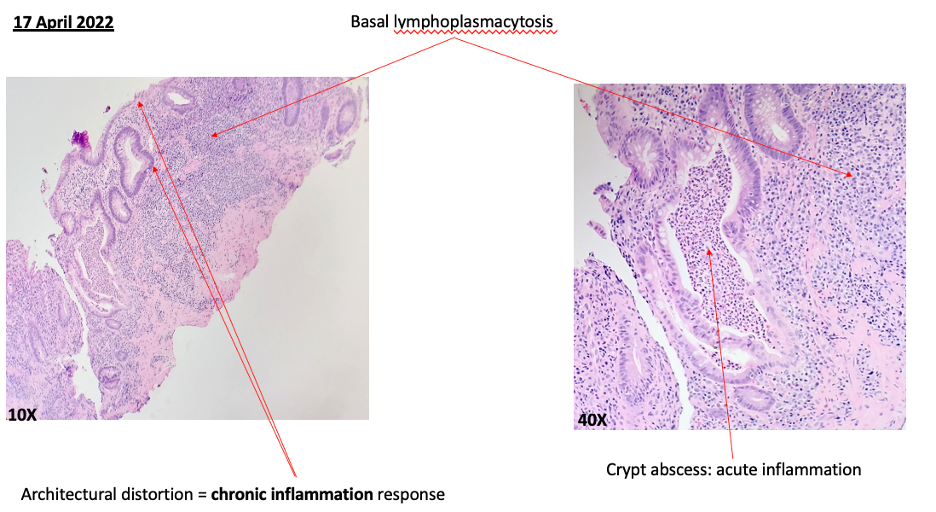
Figure: Figure 1: Histology slides of the sigmoid colon.
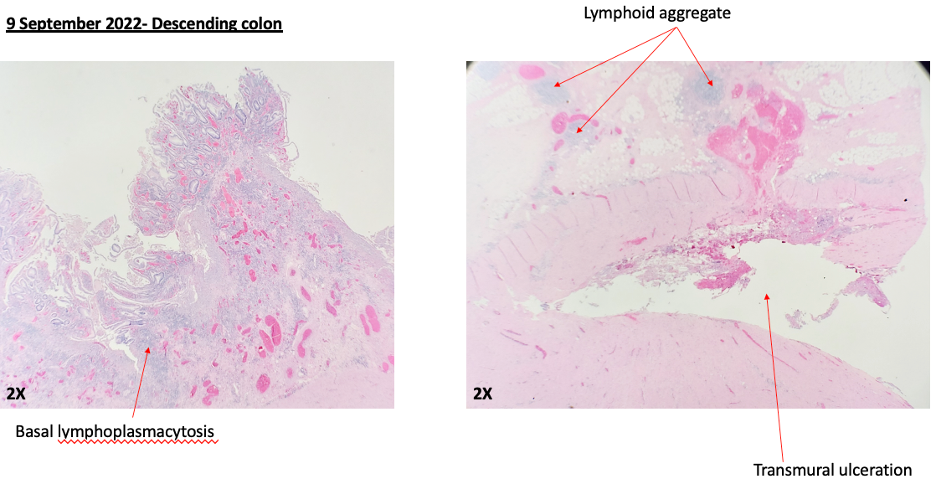
Figure: Figure 2: Repeat colonoscopy to re-evaluate underlying diagnosis of SCAD.
Disclosures:
Muzzafar Haque indicated no relevant financial relationships.
Sanchit Bhasin indicated no relevant financial relationships.
Sunil Samnani indicated no relevant financial relationships.
Muzzafar Haque, MD1, Sanchit Bhasin, MD01, Sunil Samnani, MBBS2. P3405 - Atypical Presentation of Crohn’s Disease Mimicking Segmental Colitis Associated with Diverticulosis in a 76-Year-Old Woman Progressing to Fulminant Pancolitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Saskatchewan, Regina, SK, Canada; 2McMaster University, Hamilton, ON, Canada
Introduction: Segmental colitis associated with diverticulosis (SCAD) is a rare entity characterized by chronic inflammation in the inter diverticular mucosa, often mimicking inflammatory bowel disease (IBD). We report an atypical case of a patient diagnosed with SCAD based on endoscopic findings, who progressed to fulminant pancolitis over 14 months requiring subtotal colectomy. Histopathology later confirmed Crohn’s disease (CD), highlighting diagnostic challenges in distinguishing SCAD from IBD.
Case Description/
Methods: A 76-year-old woman presented to the emergency department in March 2021 with severe abdominal pain, hematochezia, and weight loss. A computed tomography (CT) scan revealed partial large bowel obstruction and a flexible sigmoidoscopy demonstrating inflammation in the distal and sigmoid colon, consistent with diverticulitis. She responded to antibiotics and was discharged within a week. One month later, persistent rectal bleeding and lower abdominal pain prompted outpatient follow-up with a gastroenterologist. A repeat colonoscopy revealed inflammation confined to the sigmoid colon with diverticulosis, macroscopically consistent with SCAD. She was treated for a SCAD flare with antibiotics and 5-ASA. In April 2022, a follow-up colonoscopy showed moderately severe sigmoid inflammation, with normal mucosa proximal to the cecum. Biopsies revealed moderate to severe active chronic colitis with cryptitis. In May 2022, she re-presented with worsening abdominal pain and hematochezia. A CT scan revealed pancolitis with pericolic stranding. She had an elevation in CRP, low hemoglobin and albumin. Repeat colonoscopy revealed severe pancolitis. Histopathology now showed transmural inflammation with deep fissures extending into serosal adipose tissue favoring CD. Due to refractory symptoms, she underwent subtotal colectomy with end-ileostomy instead of advanced therapies. Postoperatively, she recovered well, with normalization of CRP and albumin, and was discharged within weeks.
Discussion: Clinicians must maintain a high index of suspicion for IBD in SCAD patients with refractory symptoms, as endoscopic and histologic overlap leading to misdiagnosis. Repeat colonoscopy with biopsies is critical to re-evaluate the diagnosis. Third, the potential progression of SCAD to IBD warrants further research to clarify whether SCAD is a distinct entity or an early manifestation of IBD in some patients. Differential diagnoses, including UC, ischemic colitis, and infectious colitis, should be systematically excluded.
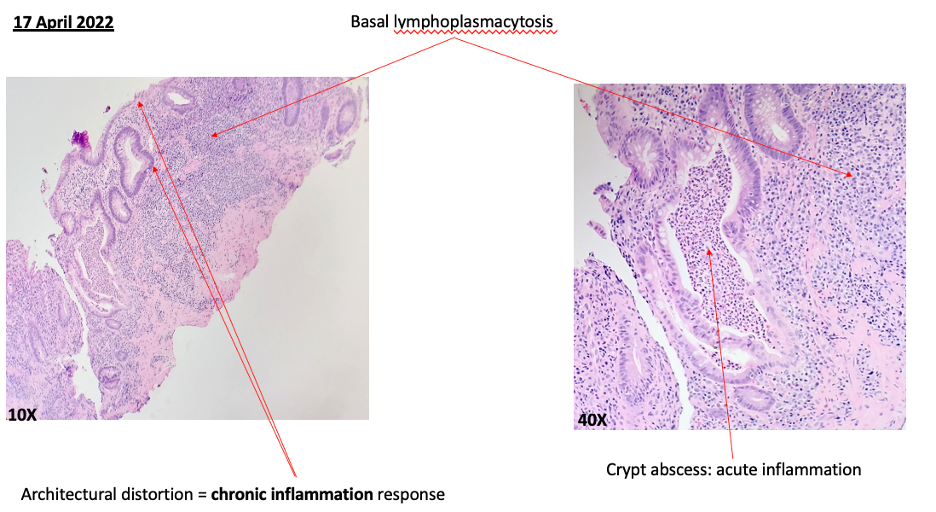
Figure: Figure 1: Histology slides of the sigmoid colon.
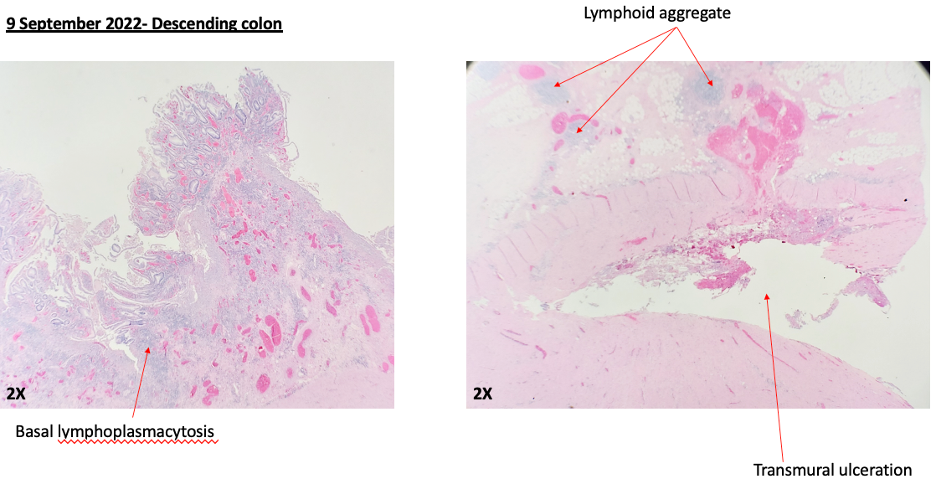
Figure: Figure 2: Repeat colonoscopy to re-evaluate underlying diagnosis of SCAD.
Disclosures:
Muzzafar Haque indicated no relevant financial relationships.
Sanchit Bhasin indicated no relevant financial relationships.
Sunil Samnani indicated no relevant financial relationships.
Muzzafar Haque, MD1, Sanchit Bhasin, MD01, Sunil Samnani, MBBS2. P3405 - Atypical Presentation of Crohn’s Disease Mimicking Segmental Colitis Associated with Diverticulosis in a 76-Year-Old Woman Progressing to Fulminant Pancolitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
