Monday Poster Session
Category: Infections and Microbiome
P3494 - From Dysentery to Disaster: Shigella-Induced Toxic Megacolon
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- JJ
Jenny Joseph, MBBS (she/her/hers)
Norwalk Hospital/Yale University
Norwalk, CT
Presenting Author(s)
Jenny Joseph, MBBS1, Juan Jose Chaves, MD2, Zablon Sewalem, MD, MSc1, Rammy Bashir, MD, MSc1, Mohammed Al-Aquily, MD1, Triston Berger, MD2, Reid Hopkins, MD2
1Norwalk Hospital/Yale University, Norwalk, CT; 2Norwalk Hospital, Norwalk, CT
Introduction: Toxic megacolon is a life-threatening non-obstructive colonic dilation in the setting of systemic toxicity commonly associated with IBD or C. difficile. Shigellosis has been linked to toxic megacolon but is rare in immunocompetent adults. Identifying infection and differentiating from inflammatory causes is critical, as management strategies differ. Surgical intervention, although rare, is necessary for refractory disease.
Case Description/
Methods: 66-year-old Indian male with a 2-week history of profuse diarrhea, initially bloody, presented with fever, tachycardia, leukocytosis (12.7 x109/L), anemia (10.7 g/dL), and electrolyte imbalances (potassium 2.7 mmol/L) after recent travel to Virginia. Stool PCR was positive for Enteroinvasive E. coli/Shigella species. Initial in-hospital stool culture was negative for Shigella but Shigella flexneri 2 was identified on a sample sent to state health lab. He was treated with ceftriaxone, later escalated to cefepime and azithromycin due to persistent symptoms. X-ray abdomen showed progressive colonic dilatation to 12.5 cm. Colonic decompression by flexible sigmoidoscopy was attempted which revealed ulcerated, inflamed mucosa. Biopsies were negative for IBD. C. difficile PCR and toxin were negative. Ongoing fever, tachycardia, electrolyte abnormalities, anemia and radiographic findings confirmed toxic megacolon. As he failed to respond to more than 10 days of antibiotics, he underwent total colectomy with end ileostomy due to impending risk of perforation. Pathology confirmed ischemic hemorrhagic colitis with ulcerations consistent with Shigella colitis. He recovered well and later underwent ileostomy reversal.
Discussion: Toxic megacolon due to Shigella is rare but can be fatal. Early identification of etiology is essential, as corticosteroids used in IBD can be harmful in infections. Stool cultures may be delayed or even negative, requiring high clinical suspicion. In our case, culture-guided antibiotics and serial imaging supported medical management initially, but worsening colonic dilation warranted surgery. It is important to consider differentials like C.difficile colitis and IBD in cases of shigellosis, as these conditions may coexist or occur in close succession. Antibiotic management of shigellosis is also complicated by resistance, and the association with hemolytic uremic syndrome. This case underscores the importance of recognizing rare infectious causes of toxic megacolon, and close coordination between medical and surgical teams.
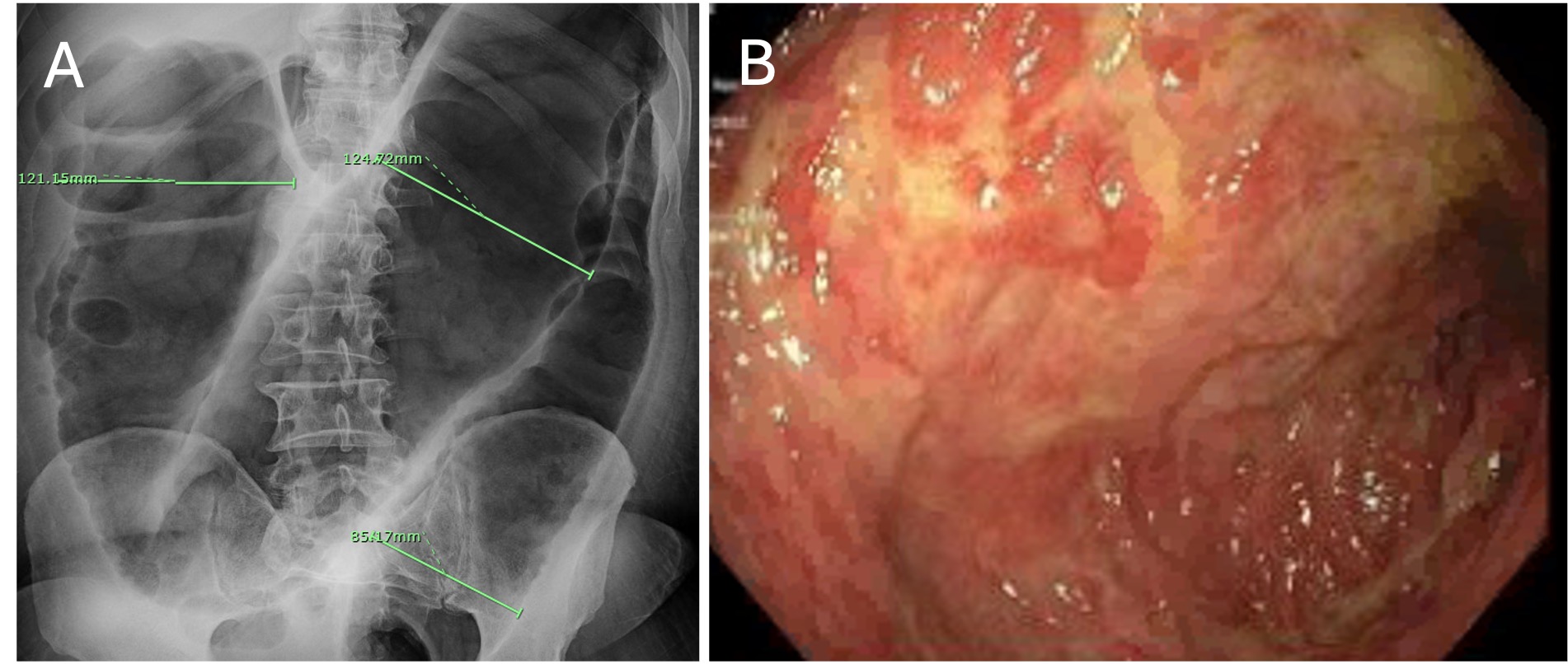
Figure: Figure 1. (A)Xray abdomen showing severe colonic distension; transverse colon measuring 12.5cm (B)Flexible sigmoidoscopy with evidence of congested, erythematous, inflamed, and ulcerated mucosa in the sigmoid colon
Disclosures:
Jenny Joseph indicated no relevant financial relationships.
Juan Jose Chaves indicated no relevant financial relationships.
Zablon Sewalem indicated no relevant financial relationships.
Rammy Bashir indicated no relevant financial relationships.
Mohammed Al-Aquily indicated no relevant financial relationships.
Triston Berger indicated no relevant financial relationships.
Reid Hopkins indicated no relevant financial relationships.
Jenny Joseph, MBBS1, Juan Jose Chaves, MD2, Zablon Sewalem, MD, MSc1, Rammy Bashir, MD, MSc1, Mohammed Al-Aquily, MD1, Triston Berger, MD2, Reid Hopkins, MD2. P3494 - From Dysentery to Disaster: Shigella-Induced Toxic Megacolon, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Norwalk Hospital/Yale University, Norwalk, CT; 2Norwalk Hospital, Norwalk, CT
Introduction: Toxic megacolon is a life-threatening non-obstructive colonic dilation in the setting of systemic toxicity commonly associated with IBD or C. difficile. Shigellosis has been linked to toxic megacolon but is rare in immunocompetent adults. Identifying infection and differentiating from inflammatory causes is critical, as management strategies differ. Surgical intervention, although rare, is necessary for refractory disease.
Case Description/
Methods: 66-year-old Indian male with a 2-week history of profuse diarrhea, initially bloody, presented with fever, tachycardia, leukocytosis (12.7 x109/L), anemia (10.7 g/dL), and electrolyte imbalances (potassium 2.7 mmol/L) after recent travel to Virginia. Stool PCR was positive for Enteroinvasive E. coli/Shigella species. Initial in-hospital stool culture was negative for Shigella but Shigella flexneri 2 was identified on a sample sent to state health lab. He was treated with ceftriaxone, later escalated to cefepime and azithromycin due to persistent symptoms. X-ray abdomen showed progressive colonic dilatation to 12.5 cm. Colonic decompression by flexible sigmoidoscopy was attempted which revealed ulcerated, inflamed mucosa. Biopsies were negative for IBD. C. difficile PCR and toxin were negative. Ongoing fever, tachycardia, electrolyte abnormalities, anemia and radiographic findings confirmed toxic megacolon. As he failed to respond to more than 10 days of antibiotics, he underwent total colectomy with end ileostomy due to impending risk of perforation. Pathology confirmed ischemic hemorrhagic colitis with ulcerations consistent with Shigella colitis. He recovered well and later underwent ileostomy reversal.
Discussion: Toxic megacolon due to Shigella is rare but can be fatal. Early identification of etiology is essential, as corticosteroids used in IBD can be harmful in infections. Stool cultures may be delayed or even negative, requiring high clinical suspicion. In our case, culture-guided antibiotics and serial imaging supported medical management initially, but worsening colonic dilation warranted surgery. It is important to consider differentials like C.difficile colitis and IBD in cases of shigellosis, as these conditions may coexist or occur in close succession. Antibiotic management of shigellosis is also complicated by resistance, and the association with hemolytic uremic syndrome. This case underscores the importance of recognizing rare infectious causes of toxic megacolon, and close coordination between medical and surgical teams.
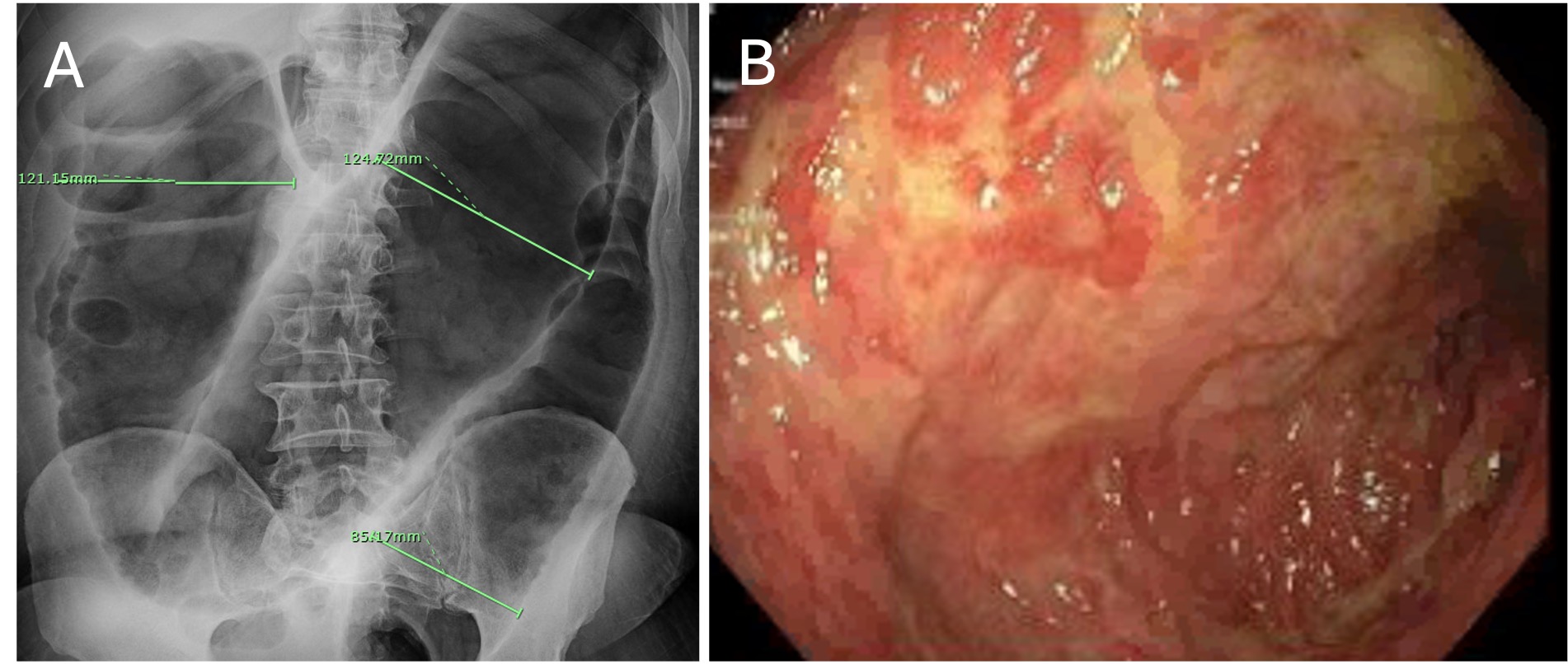
Figure: Figure 1. (A)Xray abdomen showing severe colonic distension; transverse colon measuring 12.5cm (B)Flexible sigmoidoscopy with evidence of congested, erythematous, inflamed, and ulcerated mucosa in the sigmoid colon
Disclosures:
Jenny Joseph indicated no relevant financial relationships.
Juan Jose Chaves indicated no relevant financial relationships.
Zablon Sewalem indicated no relevant financial relationships.
Rammy Bashir indicated no relevant financial relationships.
Mohammed Al-Aquily indicated no relevant financial relationships.
Triston Berger indicated no relevant financial relationships.
Reid Hopkins indicated no relevant financial relationships.
Jenny Joseph, MBBS1, Juan Jose Chaves, MD2, Zablon Sewalem, MD, MSc1, Rammy Bashir, MD, MSc1, Mohammed Al-Aquily, MD1, Triston Berger, MD2, Reid Hopkins, MD2. P3494 - From Dysentery to Disaster: Shigella-Induced Toxic Megacolon, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
