Monday Poster Session
Category: Infections and Microbiome
P3489 - Beyond the Scope: Whipple’s Disease Diagnosed by Molecular Testing (PCR) After Negative Endoscopy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Elena F. Cattaneo, BS, BA (she/her/hers)
University of Minnesota Medical School
Saint Paul, MN
Presenting Author(s)
Elena F. Cattaneo, BS, BA1, Ryan Alexander, MD2, Jessica Atieh, MD2, Navreet Chowla, MD, FACG2
1University of Minnesota Medical School, Saint Paul, MN; 2Mayo Clinic, Rochester, MN
Introduction: Whipple’s disease (WD) is a rare, multisystem disease caused by infection with the bacterium Tropheryma whipplei. It classically presents with weight loss, diarrhea, abdominal pain, arthritis, and neurologic symptoms, but is also considered one of medicine’s ‘great imitators’. Here we report a case of WD with a rare presentation of diffuse granulomatous lymphadenopathy.
Case Description/
Methods: A 52-year-old man with no pertinent medical history presented with nine months of abdominal pain, alternating constipation and diarrhea, fatigue, and a 50 pound weight loss. Labs showed low bicarbonate, albumin 2.5, ESR 71 and CRP 50. He had low levels of fat-soluble vitamins and iron. Colonoscopy and esophagogastroduodenoscopy (EGD) were endoscopically normal, but biopsies showed non-necrotizing granulomas in the terminal ileum and duodenum. CT abdomen/pelvis showed diffuse lymphadenopathy. QuantiFERON and HIV tests were negative. Crohn’s disease (CD) was suspected, and he was treated with prednisone without improvement. Upon presentation to our institution, additional testing included PET-CT which showed diffuse jejunal FDG uptake suggestive of a lymphoproliferative process or atypical infection. Fungal studies were negative. Inguinal lymph node biopsy showed non-necrotizing granulomas, and bone marrow biopsy revealed hemophagocytosis. As part of granulomatous disease workup, serum polymerase chain reaction (PCR) was obtained and was positive for T. whipplei. Repeat EGD showed duodenal lymphangiectasia (Figure 1) and biopsies demonstrated numerous foamy macrophages. Duodenal PCR confirmed T. whipplei, establishing the diagnosis of WD. He was started on hydroxychloroquine and doxycycline.
Discussion: WD is a multisystemic infection that is challenging to diagnose due to its rarity and nonspecific features. Granulomatous diseases have a wide differential including CD, sarcoidosis, atypical infections, and hematologic malignancies; WD should be considered once these are excluded. The initial endoscopically normal EGD with negative Periodic Acid-Schiff (PAS) biopsies decreased suspicion for WD, but up to 30% may lack PAS-positive foamy macrophages. Thus, molecular confirmation with PCR on tissue is essential in these cases. Blood PCR alone is insufficient as T. whipplei can be found in the serum of asymptomatic carriers. This case highlights how WD is a great masquerader and reinforces the role of molecular diagnostics and multidisciplinary collaboration in identifying this elusive but treatable disease.
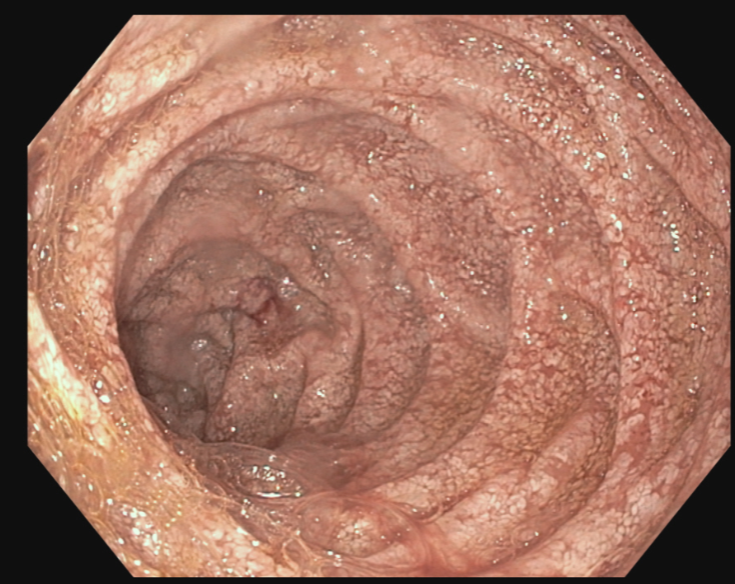
Figure: Figure 1. Endoscopic lymphangiectasia of the duodenum.
Disclosures:
Elena Cattaneo indicated no relevant financial relationships.
Ryan Alexander indicated no relevant financial relationships.
Jessica Atieh indicated no relevant financial relationships.
Navreet Chowla indicated no relevant financial relationships.
Elena F. Cattaneo, BS, BA1, Ryan Alexander, MD2, Jessica Atieh, MD2, Navreet Chowla, MD, FACG2. P3489 - Beyond the Scope: Whipple’s Disease Diagnosed by Molecular Testing (PCR) After Negative Endoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Minnesota Medical School, Saint Paul, MN; 2Mayo Clinic, Rochester, MN
Introduction: Whipple’s disease (WD) is a rare, multisystem disease caused by infection with the bacterium Tropheryma whipplei. It classically presents with weight loss, diarrhea, abdominal pain, arthritis, and neurologic symptoms, but is also considered one of medicine’s ‘great imitators’. Here we report a case of WD with a rare presentation of diffuse granulomatous lymphadenopathy.
Case Description/
Methods: A 52-year-old man with no pertinent medical history presented with nine months of abdominal pain, alternating constipation and diarrhea, fatigue, and a 50 pound weight loss. Labs showed low bicarbonate, albumin 2.5, ESR 71 and CRP 50. He had low levels of fat-soluble vitamins and iron. Colonoscopy and esophagogastroduodenoscopy (EGD) were endoscopically normal, but biopsies showed non-necrotizing granulomas in the terminal ileum and duodenum. CT abdomen/pelvis showed diffuse lymphadenopathy. QuantiFERON and HIV tests were negative. Crohn’s disease (CD) was suspected, and he was treated with prednisone without improvement. Upon presentation to our institution, additional testing included PET-CT which showed diffuse jejunal FDG uptake suggestive of a lymphoproliferative process or atypical infection. Fungal studies were negative. Inguinal lymph node biopsy showed non-necrotizing granulomas, and bone marrow biopsy revealed hemophagocytosis. As part of granulomatous disease workup, serum polymerase chain reaction (PCR) was obtained and was positive for T. whipplei. Repeat EGD showed duodenal lymphangiectasia (Figure 1) and biopsies demonstrated numerous foamy macrophages. Duodenal PCR confirmed T. whipplei, establishing the diagnosis of WD. He was started on hydroxychloroquine and doxycycline.
Discussion: WD is a multisystemic infection that is challenging to diagnose due to its rarity and nonspecific features. Granulomatous diseases have a wide differential including CD, sarcoidosis, atypical infections, and hematologic malignancies; WD should be considered once these are excluded. The initial endoscopically normal EGD with negative Periodic Acid-Schiff (PAS) biopsies decreased suspicion for WD, but up to 30% may lack PAS-positive foamy macrophages. Thus, molecular confirmation with PCR on tissue is essential in these cases. Blood PCR alone is insufficient as T. whipplei can be found in the serum of asymptomatic carriers. This case highlights how WD is a great masquerader and reinforces the role of molecular diagnostics and multidisciplinary collaboration in identifying this elusive but treatable disease.
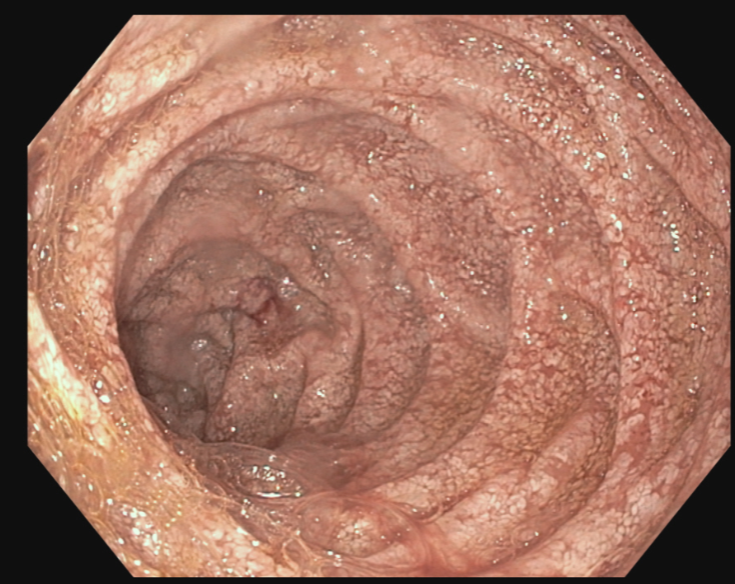
Figure: Figure 1. Endoscopic lymphangiectasia of the duodenum.
Disclosures:
Elena Cattaneo indicated no relevant financial relationships.
Ryan Alexander indicated no relevant financial relationships.
Jessica Atieh indicated no relevant financial relationships.
Navreet Chowla indicated no relevant financial relationships.
Elena F. Cattaneo, BS, BA1, Ryan Alexander, MD2, Jessica Atieh, MD2, Navreet Chowla, MD, FACG2. P3489 - Beyond the Scope: Whipple’s Disease Diagnosed by Molecular Testing (PCR) After Negative Endoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
