Monday Poster Session
Category: Infections and Microbiome
P3476 - An Unusual Case of Disseminated Nocardia in an Immunocompetent Patient
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- FP
Felicia Peoples, MD (she/her/hers)
Atrium Health Wake Forest Baptist
Winston-Salem, NC
Presenting Author(s)
Felicia Peoples, MD, Anton J. De Witte, MD, Meredith Clary, MD
Atrium Health Wake Forest Baptist, Winston-Salem, NC
Introduction: Fistulizing diseases require thorough work up of etiology, including inflammatory and infectious. These diseases can simultaneously affect multiple systems of the body, making diagnosis complicated. It is important to rule out the presence of IBD anytime fistulas involve the GI tract.
Case Description/
Methods: Patient was a 45 year old male from Mexico with a past medical history of recurrent draining abdominal wall and left axilla abscesses since age 13 that would heal within 2 months. He had left axilla I&D in 2019 with doxycycline treatment, then was lost to follow up. He presented again after abscesses had been draining for more than 1 year, with change in drainage from serosanguinous to purulent with fecal matter. He had associated 40 lb unintentional weight loss with night sweats. Labs significant for WBC 13.6, ALP 143, CRP 170, A1c 8.1%, and fecal calprotectin 326. CT AP with contrast showed gastro-cutaneous/colocutaneous/enterocutaneous fistulae, hepatic abscess with hepatocutaneous fistula, and collections along left anterior peritoneal wall and left ventral abdominal wall. Dermatology was consulted, who obtained skin biopsies concerning for hidradenitis suppurativa (HS). GI was consulted due to concern for IBD. EGD revealed Candida esophagitis, and fistulous tracts in the gastric body, gastric antrum, and duodenum. Colonoscopy showed fistulous tracts in the transverse and descending colon. No visual or biopsy evidence of IBD. Skin abscess culture grew Nocardia brasiliensis. ID was consulted who recommended empiric TMP/SMX and moxifloxacin for disseminated Nocardia. HIV screen was negative and quantitative immunoglobulins were normal. MRI brain was negative, however CT thorax showed retrosternal soft tissue extending to the peritoneum, and concerns for sternum/left rib osteomyelitis. Patient planned to complete a 6 month antibiotic course.
Discussion: Nocardia is an infectious cause of fistulas with visual/histologic skin changes similar to HS. It is found in soil, and infection occurs via inhalation or percutaneous contiguous spread. It remains localized to inoculation sites in the immunocompetent, but can disseminate in the immunocompromised most often with brain abscess. Infection in abdominal/retroperitoneal sites could be from hematogenous spread vs slowly progressive pyogenic percutaneous spread. This patient was likely exposed percutaneously via farm work in Mexico, and had progressive percutaneous spread that may have been exacerbated by unidentified immunocompromising disease.

Figure: Actively oozing cutaneous fistulas with diffuse abdominal wall scarring from prior abscesses
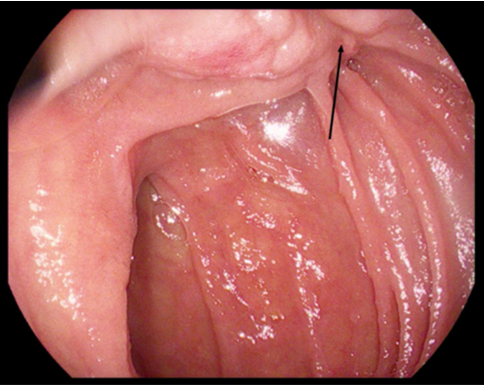
Figure: 2nd part of duodenum with suspected enteric fistula (see arrow)
Disclosures:
Felicia Peoples indicated no relevant financial relationships.
Anton De Witte indicated no relevant financial relationships.
Meredith Clary indicated no relevant financial relationships.
Felicia Peoples, MD, Anton J. De Witte, MD, Meredith Clary, MD. P3476 - An Unusual Case of Disseminated Nocardia in an Immunocompetent Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Atrium Health Wake Forest Baptist, Winston-Salem, NC
Introduction: Fistulizing diseases require thorough work up of etiology, including inflammatory and infectious. These diseases can simultaneously affect multiple systems of the body, making diagnosis complicated. It is important to rule out the presence of IBD anytime fistulas involve the GI tract.
Case Description/
Methods: Patient was a 45 year old male from Mexico with a past medical history of recurrent draining abdominal wall and left axilla abscesses since age 13 that would heal within 2 months. He had left axilla I&D in 2019 with doxycycline treatment, then was lost to follow up. He presented again after abscesses had been draining for more than 1 year, with change in drainage from serosanguinous to purulent with fecal matter. He had associated 40 lb unintentional weight loss with night sweats. Labs significant for WBC 13.6, ALP 143, CRP 170, A1c 8.1%, and fecal calprotectin 326. CT AP with contrast showed gastro-cutaneous/colocutaneous/enterocutaneous fistulae, hepatic abscess with hepatocutaneous fistula, and collections along left anterior peritoneal wall and left ventral abdominal wall. Dermatology was consulted, who obtained skin biopsies concerning for hidradenitis suppurativa (HS). GI was consulted due to concern for IBD. EGD revealed Candida esophagitis, and fistulous tracts in the gastric body, gastric antrum, and duodenum. Colonoscopy showed fistulous tracts in the transverse and descending colon. No visual or biopsy evidence of IBD. Skin abscess culture grew Nocardia brasiliensis. ID was consulted who recommended empiric TMP/SMX and moxifloxacin for disseminated Nocardia. HIV screen was negative and quantitative immunoglobulins were normal. MRI brain was negative, however CT thorax showed retrosternal soft tissue extending to the peritoneum, and concerns for sternum/left rib osteomyelitis. Patient planned to complete a 6 month antibiotic course.
Discussion: Nocardia is an infectious cause of fistulas with visual/histologic skin changes similar to HS. It is found in soil, and infection occurs via inhalation or percutaneous contiguous spread. It remains localized to inoculation sites in the immunocompetent, but can disseminate in the immunocompromised most often with brain abscess. Infection in abdominal/retroperitoneal sites could be from hematogenous spread vs slowly progressive pyogenic percutaneous spread. This patient was likely exposed percutaneously via farm work in Mexico, and had progressive percutaneous spread that may have been exacerbated by unidentified immunocompromising disease.

Figure: Actively oozing cutaneous fistulas with diffuse abdominal wall scarring from prior abscesses
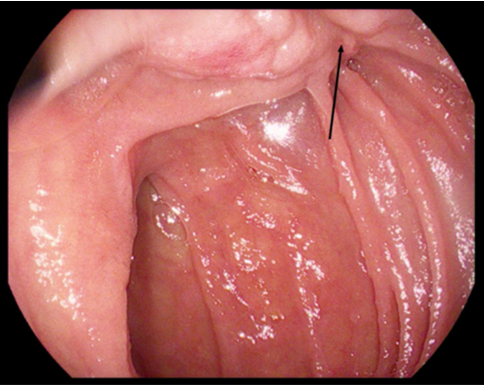
Figure: 2nd part of duodenum with suspected enteric fistula (see arrow)
Disclosures:
Felicia Peoples indicated no relevant financial relationships.
Anton De Witte indicated no relevant financial relationships.
Meredith Clary indicated no relevant financial relationships.
Felicia Peoples, MD, Anton J. De Witte, MD, Meredith Clary, MD. P3476 - An Unusual Case of Disseminated Nocardia in an Immunocompetent Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
