Monday Poster Session
Category: Interventional Endoscopy
P3556 - POEM vs Heller Myotomy: A Nationwide 30-Day Outcomes and Procedural Equity in Achalasia
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mohammad AbuAssi, MD (he/him/his)
University of Central Florida, HCA Healthcare GME
Gainesville, FL
Presenting Author(s)
Mohammad Abuassi, MD1, Hadi Khaled. Abou Zeid, MD2, Yaman Mkhaimer, MD3, Kobina Essilfie-Quaye, MD4, Tony Brar, MD4, Mahmoud Y. Madi, MD5, Yaseen Perbtani, DO1
1University of Central Florida, HCA Healthcare GME, Gainesville, FL; 2Mayo Clinic, Rochester, MN; 3Washington university in St. Louis, St. Louis, MO; 4University of Central Florida, Gainesville, FL; 5University of Texas at Austin Dell Medical School, Austin, TX
Introduction: Peroral endoscopic myotomy (POEM) and laparoscopic Heller myotomy (LHM) are definitive treatments for achalasia. However, real-world data comparing short-term safety outcomes and utilization patterns remain limited, and disparities in procedural access are not well characterized. We aimed to evaluate 30-day outcomes and demographic representation among patients undergoing POEM versus LHM.
Methods: We used the TriNetX U.S. Collaborative Network to identify adults with achalasia who underwent POEM or Heller myotomy between January 2022 and May 2025. A 1:1 propensity score match (n = 1,963 per group) was performed using baseline variables including age, sex, race/ethnicity, and clinical comorbidities. We then compared 30-day mortality, complications, medication use, and diagnostic resource utilization. Risk ratios (RR) were calculated. Kaplan–Meier analysis evaluated survival. Racial and ethnic distributions were compared prior to matching to assess potential disparities in procedural access.
Results: POEM patients were slightly more racially and ethnically diverse than those undergoing Heller (White: 70.7% vs 75.2%; Black: 7.0% vs 6.1%; Hispanic: 4.1% vs 3.8%; Other/Unknown: 15.7% vs 12.6%). After matching, POEM was associated with significantly lower 30-day mortality (0% vs 0.5%; p = 0.002) and a reduced risk of pneumothorax (0.8% vs 2.0%; RR 0.38; p = 0.001). ICU admissions were lower in POEM, though not statistically significant (1.2% vs 1.9%; p = 0.073). POEM patients had markedly reduced need for opioids (38.8% vs 79.7%; RR 0.49), non-opioid analgesics (36.6% vs 74.9%; RR 0.49), antiemetics (27.6% vs 39.4%; RR 0.70), and diagnostic radiology (55.2% vs 65.4%; RR 0.84), all p < 0.001. Rates of GI bleeding, perforation, AKI, respiratory failure, and emergency intubation were similar. GERD (4.5% vs 5.3%) and dysphagia (3.2% vs 3.8%) were also comparable. Kaplan–Meier survival curves revealed statistically significant survival benefits in the POEM cohort (log-rank p = 0.017).
Discussion: POEM was associated with lower short-term mortality, fewer complications, and decreased supportive care utilization compared to Heller myotomy. Pre-matching data revealed modestly greater racial and ethnic diversity among POEM recipients. This higlights the importance of preserving and expanding procedural accessibility to ensure equitable adoption of advanced endoscopic therapies nationwide.
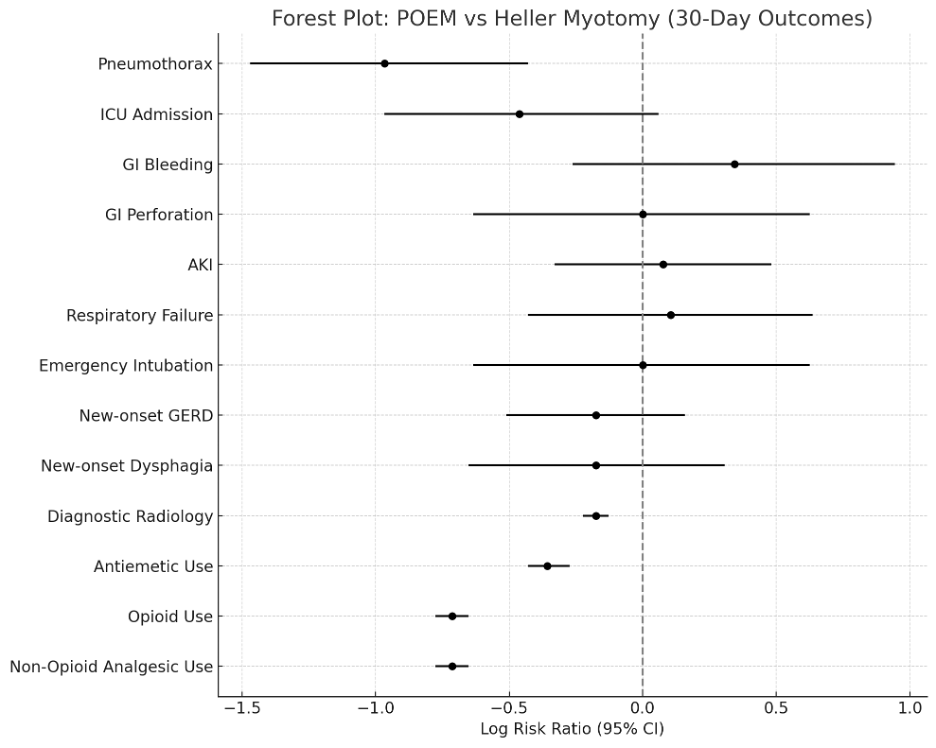
Figure: This plot illustrates the log-transformed risk ratios (RR) and 95% confidence intervals for key complications and healthcare utilization metrics within 30 days of POEM or Heller myotomy. Outcomes include pneumothorax, ICU admission, emergency interventions, new-onset GERD and dysphagia, and medication or radiologic resource use. Points to the left of the dashed vertical line indicate lower risk with POEM.
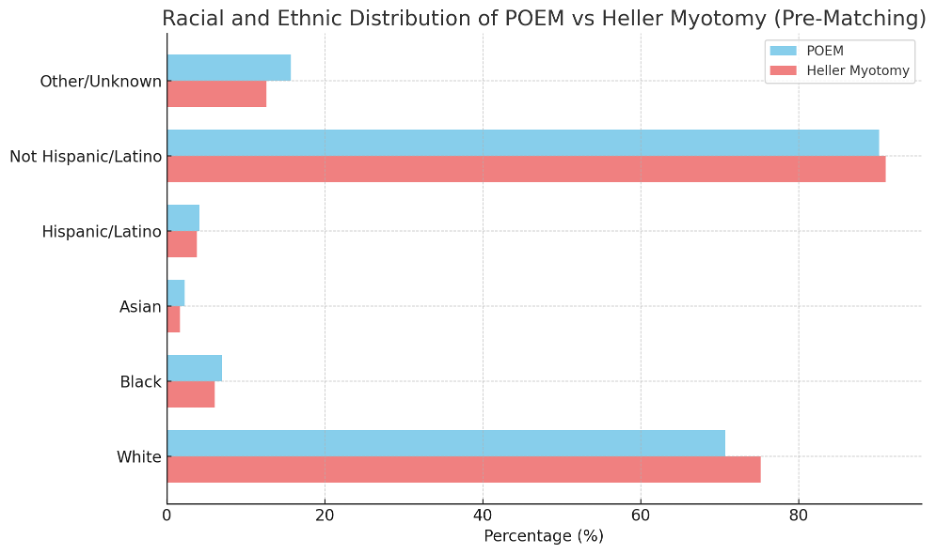
Figure: Bar graph showing the percentage distribution of race and ethnicity among patients undergoing POEM versus Heller myotomy. Compared to Heller, POEM was more commonly performed in patients identifying as Asian, Black, Hispanic, or Other/Unknown race/ethnicity, reflecting a more demographically diverse recipient population.
Disclosures:
Mohammad Abuassi indicated no relevant financial relationships.
Hadi Abou Zeid indicated no relevant financial relationships.
Yaman Mkhaimer indicated no relevant financial relationships.
Kobina Essilfie-Quaye indicated no relevant financial relationships.
Tony Brar indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Yaseen Perbtani indicated no relevant financial relationships.
Mohammad Abuassi, MD1, Hadi Khaled. Abou Zeid, MD2, Yaman Mkhaimer, MD3, Kobina Essilfie-Quaye, MD4, Tony Brar, MD4, Mahmoud Y. Madi, MD5, Yaseen Perbtani, DO1. P3556 - POEM vs Heller Myotomy: A Nationwide 30-Day Outcomes and Procedural Equity in Achalasia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Central Florida, HCA Healthcare GME, Gainesville, FL; 2Mayo Clinic, Rochester, MN; 3Washington university in St. Louis, St. Louis, MO; 4University of Central Florida, Gainesville, FL; 5University of Texas at Austin Dell Medical School, Austin, TX
Introduction: Peroral endoscopic myotomy (POEM) and laparoscopic Heller myotomy (LHM) are definitive treatments for achalasia. However, real-world data comparing short-term safety outcomes and utilization patterns remain limited, and disparities in procedural access are not well characterized. We aimed to evaluate 30-day outcomes and demographic representation among patients undergoing POEM versus LHM.
Methods: We used the TriNetX U.S. Collaborative Network to identify adults with achalasia who underwent POEM or Heller myotomy between January 2022 and May 2025. A 1:1 propensity score match (n = 1,963 per group) was performed using baseline variables including age, sex, race/ethnicity, and clinical comorbidities. We then compared 30-day mortality, complications, medication use, and diagnostic resource utilization. Risk ratios (RR) were calculated. Kaplan–Meier analysis evaluated survival. Racial and ethnic distributions were compared prior to matching to assess potential disparities in procedural access.
Results: POEM patients were slightly more racially and ethnically diverse than those undergoing Heller (White: 70.7% vs 75.2%; Black: 7.0% vs 6.1%; Hispanic: 4.1% vs 3.8%; Other/Unknown: 15.7% vs 12.6%). After matching, POEM was associated with significantly lower 30-day mortality (0% vs 0.5%; p = 0.002) and a reduced risk of pneumothorax (0.8% vs 2.0%; RR 0.38; p = 0.001). ICU admissions were lower in POEM, though not statistically significant (1.2% vs 1.9%; p = 0.073). POEM patients had markedly reduced need for opioids (38.8% vs 79.7%; RR 0.49), non-opioid analgesics (36.6% vs 74.9%; RR 0.49), antiemetics (27.6% vs 39.4%; RR 0.70), and diagnostic radiology (55.2% vs 65.4%; RR 0.84), all p < 0.001. Rates of GI bleeding, perforation, AKI, respiratory failure, and emergency intubation were similar. GERD (4.5% vs 5.3%) and dysphagia (3.2% vs 3.8%) were also comparable. Kaplan–Meier survival curves revealed statistically significant survival benefits in the POEM cohort (log-rank p = 0.017).
Discussion: POEM was associated with lower short-term mortality, fewer complications, and decreased supportive care utilization compared to Heller myotomy. Pre-matching data revealed modestly greater racial and ethnic diversity among POEM recipients. This higlights the importance of preserving and expanding procedural accessibility to ensure equitable adoption of advanced endoscopic therapies nationwide.
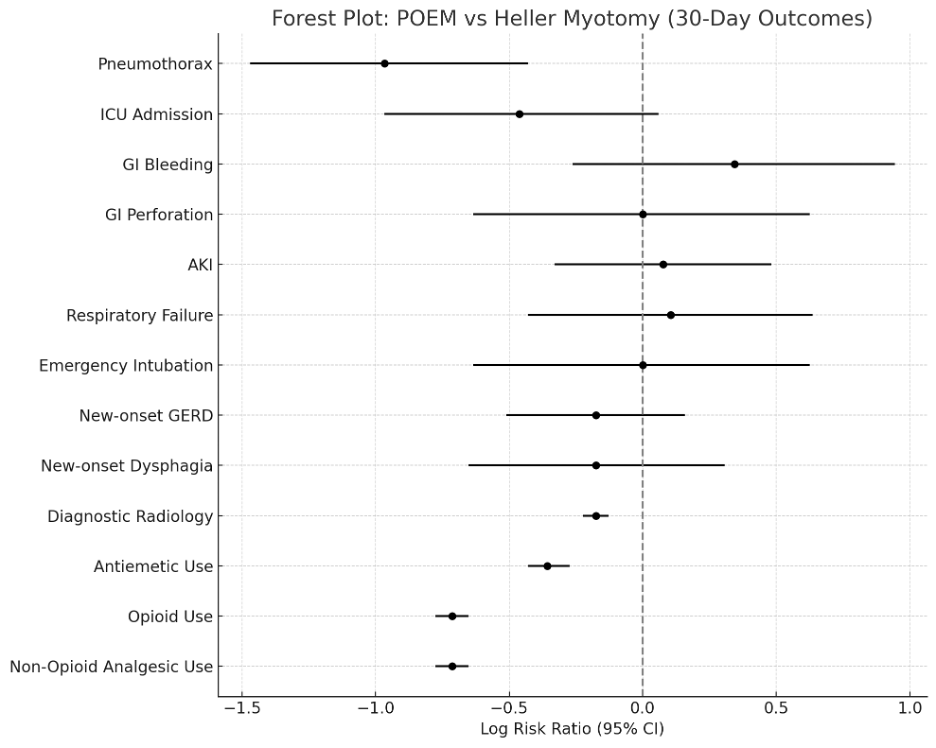
Figure: This plot illustrates the log-transformed risk ratios (RR) and 95% confidence intervals for key complications and healthcare utilization metrics within 30 days of POEM or Heller myotomy. Outcomes include pneumothorax, ICU admission, emergency interventions, new-onset GERD and dysphagia, and medication or radiologic resource use. Points to the left of the dashed vertical line indicate lower risk with POEM.
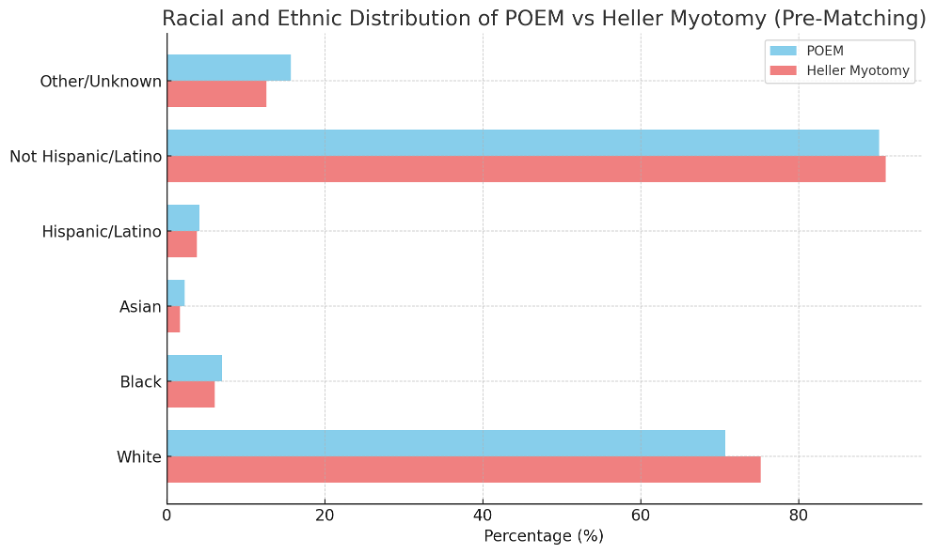
Figure: Bar graph showing the percentage distribution of race and ethnicity among patients undergoing POEM versus Heller myotomy. Compared to Heller, POEM was more commonly performed in patients identifying as Asian, Black, Hispanic, or Other/Unknown race/ethnicity, reflecting a more demographically diverse recipient population.
Disclosures:
Mohammad Abuassi indicated no relevant financial relationships.
Hadi Abou Zeid indicated no relevant financial relationships.
Yaman Mkhaimer indicated no relevant financial relationships.
Kobina Essilfie-Quaye indicated no relevant financial relationships.
Tony Brar indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Yaseen Perbtani indicated no relevant financial relationships.
Mohammad Abuassi, MD1, Hadi Khaled. Abou Zeid, MD2, Yaman Mkhaimer, MD3, Kobina Essilfie-Quaye, MD4, Tony Brar, MD4, Mahmoud Y. Madi, MD5, Yaseen Perbtani, DO1. P3556 - POEM vs Heller Myotomy: A Nationwide 30-Day Outcomes and Procedural Equity in Achalasia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
