Monday Poster Session
Category: Interventional Endoscopy
P3545 - Efficacy and Safety of Gastric Underwater Endoscopic Mucosal Resection: Systematic Review and Meta-Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- TA
Tareq Alsaleh, MD
Department of Internal Medicine, AdventHealth Orlando
Orlando, FL
Presenting Author(s)
Tareq Alsaleh, MD1, Prachi Mann, MD2, Nihal Khan, MD1, Nouman Shafique, MD1, Mohamad Khaled Almujarkesh, MD3, Babu P. Mohan, MD4
1Department of Internal Medicine, AdventHealth Orlando, Orlando, FL; 2Department of Internal Medicine, Adventhealth Orlando, Orlando, FL; 3Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL; 4Orlando Gastroenterology PA, Orlando, FL
Introduction: Endoscopic mucosal resection (EMR) is the method of choice for resection of small gastric lesions. Underwater EMR (UEMR) is an emerging method utilizing a water-filled environment that does not require submucosal injection. A few case reports have suggested that UEMR may be advantageous for gastric lesions. We conducted a systematic review and meta-analysis of studies assessing the feasibility, efficacy, and safety of UEMR for gastric lesion resection.
Methods: A comprehensive search of MEDLINE, EMBASE, and Scopus was performed through April 2025 to identify studies reporting outcomes of UEMR for gastric neoplasms. Outcomes assessed included en bloc resection, R0 resection, recurrence, delayed bleeding, and perforation. Pooled effect estimates were calculated using a random-effects model and expressed as proportions with 95% confidence intervals (CI). Heterogeneity was assessed using the I² statistic.
Results: A total of four studies including 123 patients undergoing UEMR for gastric lesions were included in the analysis. The participants included 68 (55.3%) males. Two studies were retrospective, while the other two were case series. Length of follow-up ranged from a median of 90 days to 243 days, and the mean size of the lesions ranged from 9 mm to 10.2 mm (Table 1).
The pooled en bloc resection rate was 98.9% (95% CI: 92.3–100; I² = 57%), and the R0 resection rate was 93% (95% CI: 76.8–99.9; I² = 73.8%). The immediate bleeding rate was 4.3% (95% CI: 0.0–35.5; I² = 93%), and the recurrence rate was low, at 1.3% (95% CI: 0.1-4.1; I² = 0%), with minimal heterogeneity across studies. No incidents of delayed bleeding or perforation were reported in any of the four studies. The mean procedure time was short, at 4.8 minutes (95% CI: 1.8-7.8; I2 = 98.7%) (Figure 1).
Discussion: This meta-analysis demonstrates that UEMR is a highly effective, quick, and safe modality for the resection of small gastric neoplasms, with high en bloc and R0 resection rates and low rates of recurrence and complications. These findings support UEMR as a minimally invasive alternative to surgery for these lesions. Further prospective studies with long-term follow-up and direct comparison to conventional EMR are warranted to validate these outcomes, assess survival impact, and identify the optimal resection technique.
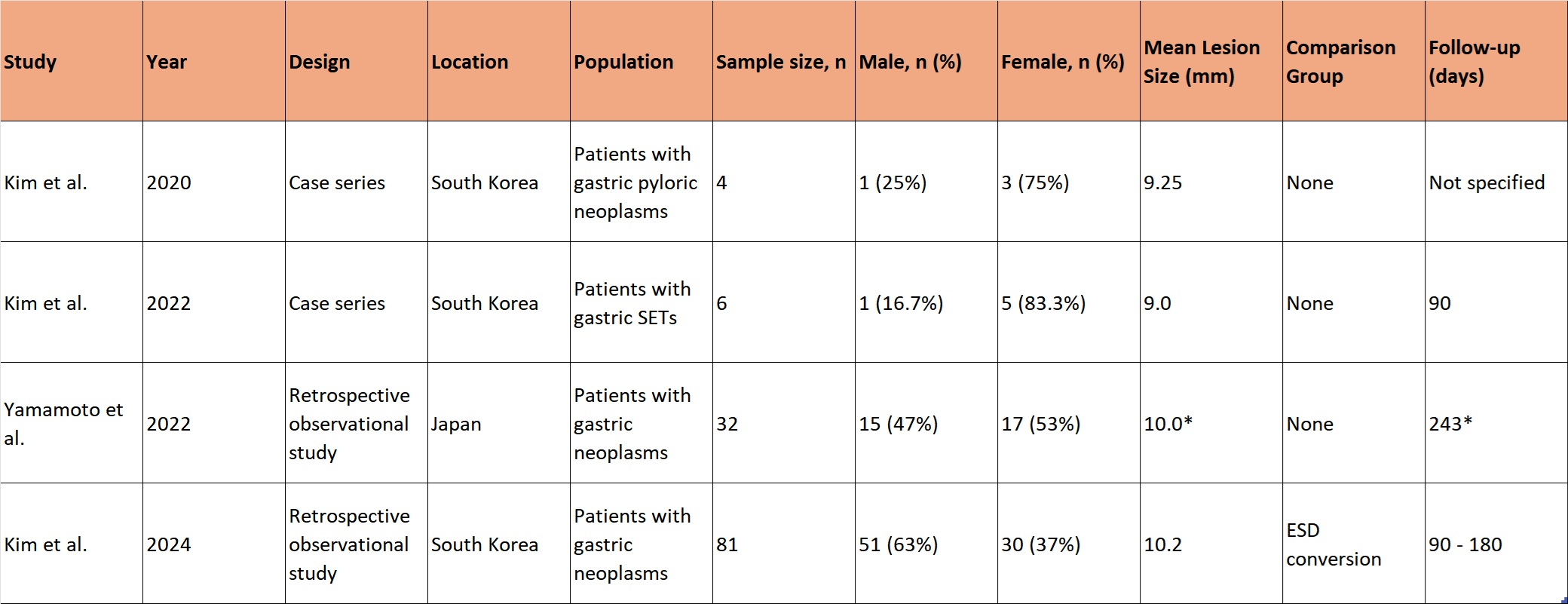
Figure: Table 1. Study characteristics
Abbreviations: EMR, Endoscopic Mucosal Resection; ESD, Endoscopic Submucosal Dissection; SETs, Subepithelial Tumors; UEMR, Underwater Endoscopic Mucosal Resection.
*Median
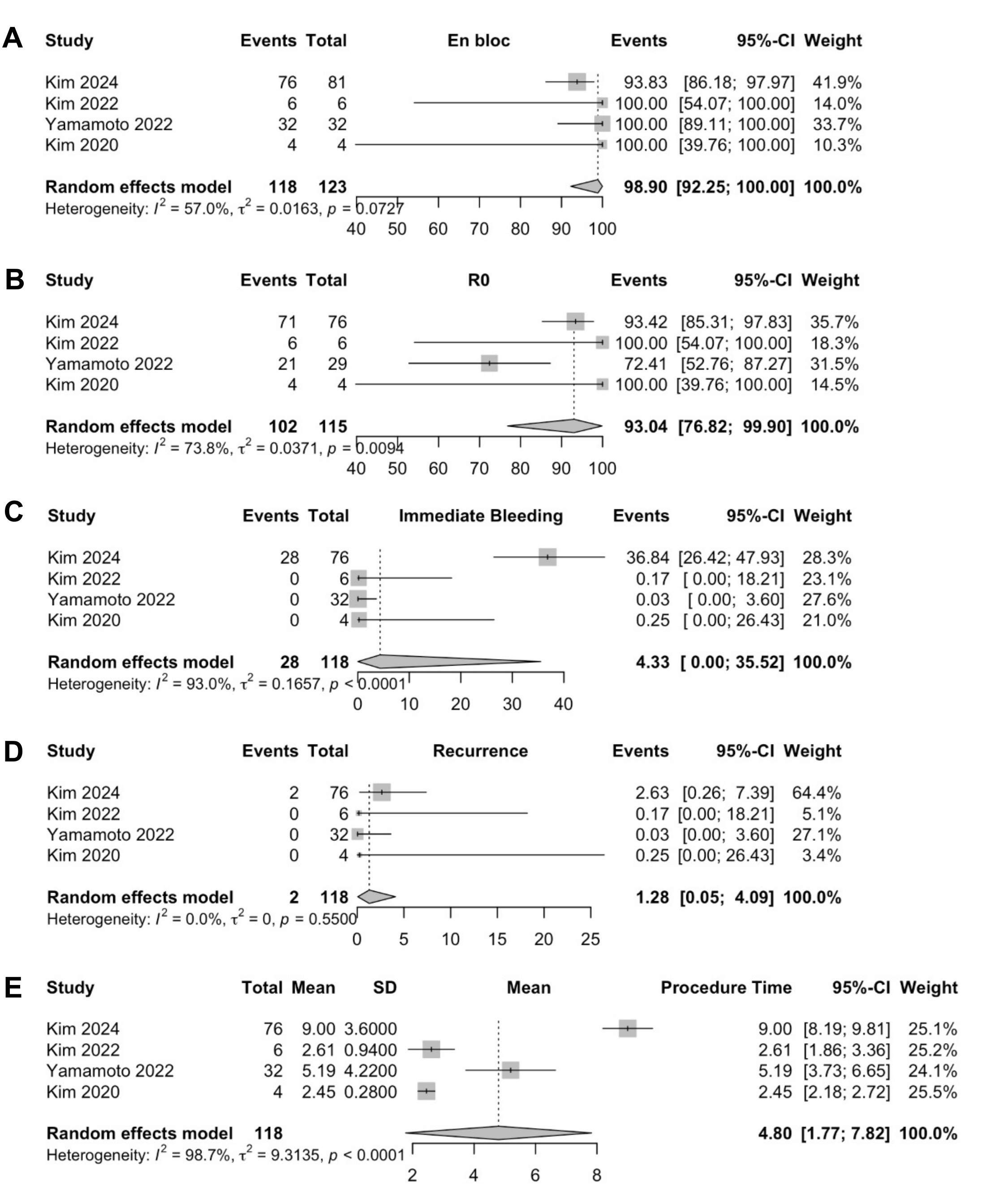
Figure: Figure 1. Analysis of proportions using random effects model showing pooled rates of:
A – En bloc resection
B – R0 resection
C – Immediate bleeding
D – Recurrence
E – Procedure time
Disclosures:
Tareq Alsaleh indicated no relevant financial relationships.
Prachi Mann indicated no relevant financial relationships.
Nihal Khan indicated no relevant financial relationships.
Nouman Shafique indicated no relevant financial relationships.
Mohamad Khaled Almujarkesh indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Tareq Alsaleh, MD1, Prachi Mann, MD2, Nihal Khan, MD1, Nouman Shafique, MD1, Mohamad Khaled Almujarkesh, MD3, Babu P. Mohan, MD4. P3545 - Efficacy and Safety of Gastric Underwater Endoscopic Mucosal Resection: Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine, AdventHealth Orlando, Orlando, FL; 2Department of Internal Medicine, Adventhealth Orlando, Orlando, FL; 3Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL; 4Orlando Gastroenterology PA, Orlando, FL
Introduction: Endoscopic mucosal resection (EMR) is the method of choice for resection of small gastric lesions. Underwater EMR (UEMR) is an emerging method utilizing a water-filled environment that does not require submucosal injection. A few case reports have suggested that UEMR may be advantageous for gastric lesions. We conducted a systematic review and meta-analysis of studies assessing the feasibility, efficacy, and safety of UEMR for gastric lesion resection.
Methods: A comprehensive search of MEDLINE, EMBASE, and Scopus was performed through April 2025 to identify studies reporting outcomes of UEMR for gastric neoplasms. Outcomes assessed included en bloc resection, R0 resection, recurrence, delayed bleeding, and perforation. Pooled effect estimates were calculated using a random-effects model and expressed as proportions with 95% confidence intervals (CI). Heterogeneity was assessed using the I² statistic.
Results: A total of four studies including 123 patients undergoing UEMR for gastric lesions were included in the analysis. The participants included 68 (55.3%) males. Two studies were retrospective, while the other two were case series. Length of follow-up ranged from a median of 90 days to 243 days, and the mean size of the lesions ranged from 9 mm to 10.2 mm (Table 1).
The pooled en bloc resection rate was 98.9% (95% CI: 92.3–100; I² = 57%), and the R0 resection rate was 93% (95% CI: 76.8–99.9; I² = 73.8%). The immediate bleeding rate was 4.3% (95% CI: 0.0–35.5; I² = 93%), and the recurrence rate was low, at 1.3% (95% CI: 0.1-4.1; I² = 0%), with minimal heterogeneity across studies. No incidents of delayed bleeding or perforation were reported in any of the four studies. The mean procedure time was short, at 4.8 minutes (95% CI: 1.8-7.8; I2 = 98.7%) (Figure 1).
Discussion: This meta-analysis demonstrates that UEMR is a highly effective, quick, and safe modality for the resection of small gastric neoplasms, with high en bloc and R0 resection rates and low rates of recurrence and complications. These findings support UEMR as a minimally invasive alternative to surgery for these lesions. Further prospective studies with long-term follow-up and direct comparison to conventional EMR are warranted to validate these outcomes, assess survival impact, and identify the optimal resection technique.
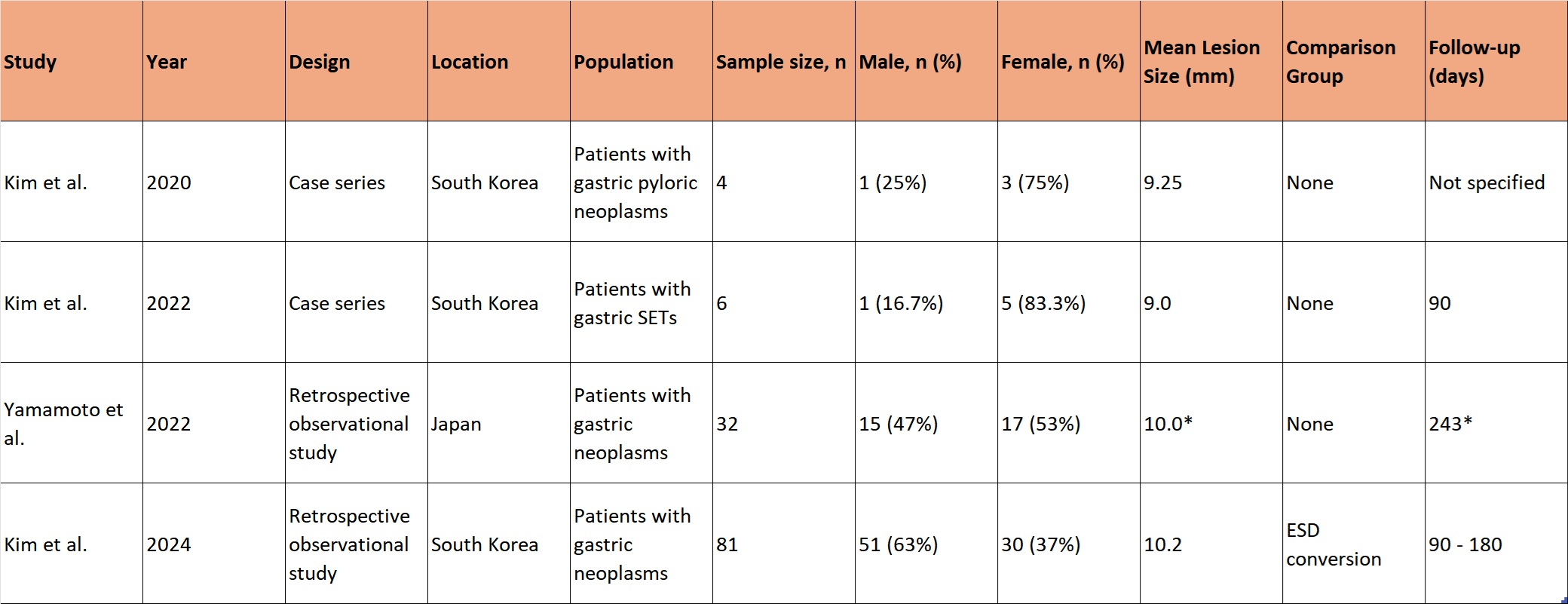
Figure: Table 1. Study characteristics
Abbreviations: EMR, Endoscopic Mucosal Resection; ESD, Endoscopic Submucosal Dissection; SETs, Subepithelial Tumors; UEMR, Underwater Endoscopic Mucosal Resection.
*Median
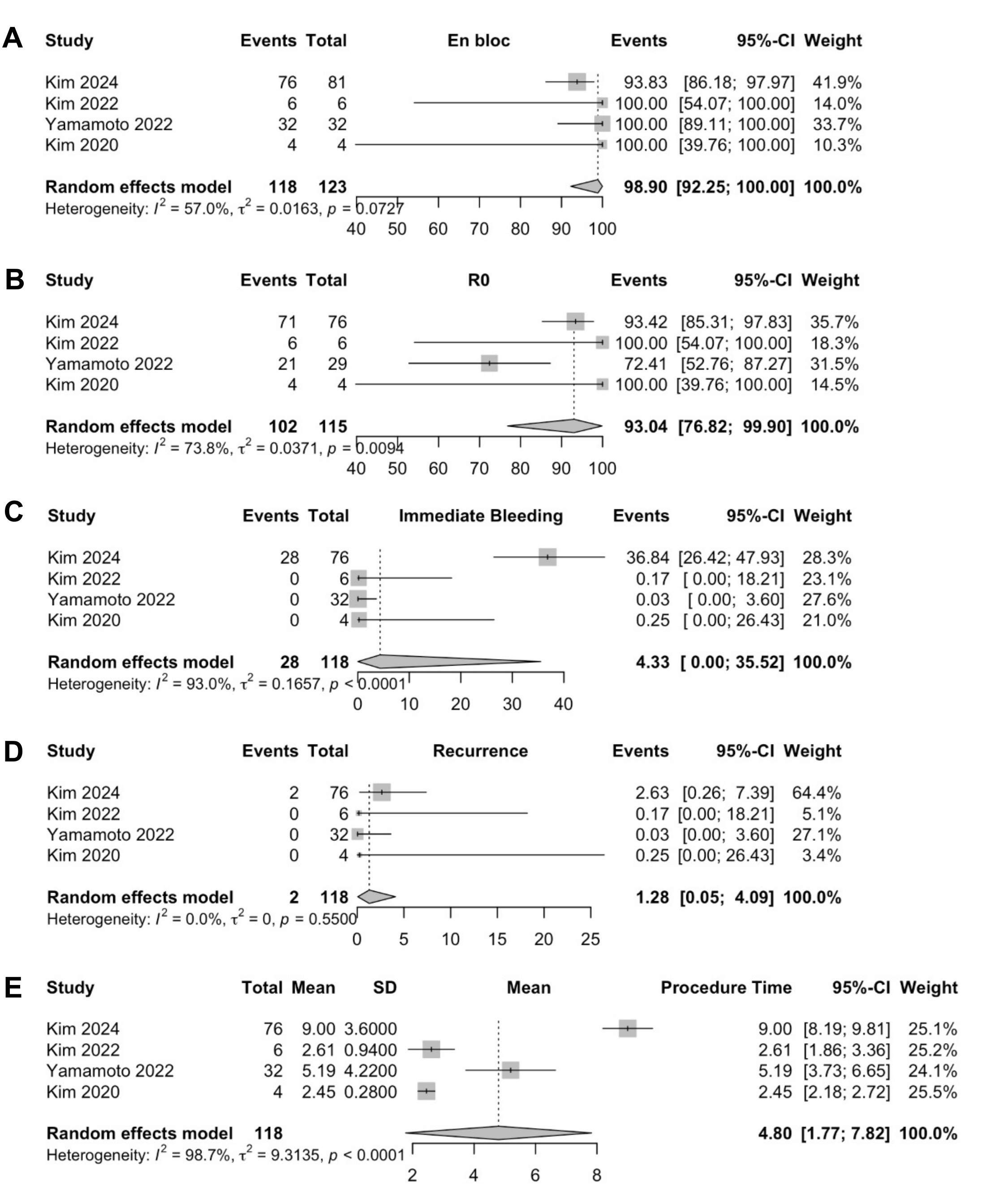
Figure: Figure 1. Analysis of proportions using random effects model showing pooled rates of:
A – En bloc resection
B – R0 resection
C – Immediate bleeding
D – Recurrence
E – Procedure time
Disclosures:
Tareq Alsaleh indicated no relevant financial relationships.
Prachi Mann indicated no relevant financial relationships.
Nihal Khan indicated no relevant financial relationships.
Nouman Shafique indicated no relevant financial relationships.
Mohamad Khaled Almujarkesh indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Tareq Alsaleh, MD1, Prachi Mann, MD2, Nihal Khan, MD1, Nouman Shafique, MD1, Mohamad Khaled Almujarkesh, MD3, Babu P. Mohan, MD4. P3545 - Efficacy and Safety of Gastric Underwater Endoscopic Mucosal Resection: Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
