Monday Poster Session
Category: Interventional Endoscopy
P3543 - Endoscopic Ultrasound versus ERCP for Biliary Drainage Prior to Surgery: A Systematic Review and Meta-Analysis of Surgical Outcomes
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- TA
Tareq Alsaleh, MD
Department of Internal Medicine, AdventHealth Orlando
Orlando, FL
Presenting Author(s)
Tareq Alsaleh, MD1, Abdul Mohammed, MD2, Mohamad Khaled Almujarkesh, MD2, Saurabh Chandan, MD3, Babu P. Mohan, MD4, John George, MD2, Maham Hayat, MD3, Deepanshu Jain, MD3, Natalie Cosgrove, MD3, Kambiz Kadkhodayan, MD3, Dennis Yang, MD, FACG5, Muhammad Hasan, MD, FACG3, Mustafa Arain, MD3
1Department of Internal Medicine, AdventHealth Orlando, Orlando, FL; 2Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL; 3Center for Interventional Endoscopy, AdventHealth Orlando, Orlando, FL; 4Orlando Gastroenterology PA, Orlando, FL; 5Center for Interventional Endoscopic, AdventHealth Orlando, Orlando, FL
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) is usually used for preoperative biliary drainage (PBD) but carries risks of post-ERCP pancreatitis and stent-related complications, potentially delaying surgery. EUS-guided biliary drainage may reduce complications, but its impact on surgical exploration remains unclear. We conducted a systematic review and meta-analysis comparing the safety and efficacy of EUS and ERCP for PBD in terms of post-operative outcomes.
Methods: A systematic review of the literature from PubMed, EMBASE, and Scopus was conducted through April 2025, for studies comparing outcomes after pancreaticoduodenectomy and other surgeries when PBD is performed with EUS or ERCP. Outcomes of interest were surgical complications, need for reintervention, length of stay, and post-operative mortality. Standard meta-analysis methods were followed using the random-effects model. Treatment effect estimates were expressed as odds ratio (OR) or mean difference (MD) and 95% confidence interval (CI). Heterogeneity was assessed using the I2% statistic.
Results: Four retrospective studies were included that reported on 546 patients (54.4% males). 185 patients underwent EUS while 361 underwent ERCP. Three studies were multicenter, while on was single center. (Table 1).
There were trends towards decreased odds of post-operative complications (OR 0.55; 95% CI [0.28, 1.09], P=0.08) and pancreatic fistula formation (OR 0.73; 95% CI [0.42, 1.25], P=0.25) in the EUS group compared to the ERCP group that were not statistically significant. There was a statistically significant decrease in mean length of stay (MD -2.96; 95% CI [-4.92, -0.99], P=0.003) and odds of need for endoscopic reintervention (OR 0.29; 95% CI [0.09, 0.87], P=0.03) in the EUS group. There was no statistically significant difference in the odds of need for surgical reintervention (OR 1.60; 95% CI [0.49, 5.40], P=0.44) or post-operative mortality (OR 2.01; 95% CI [0.44, 9.17], P=0.37) between the two groups (Figure 1).
Discussion: Our meta-analysis demonstrates that in terms of post-surgical outcomes, EUS is a feasible and potentially safe alternative to ERCP for PBD. It was associated with shorter lengths of stay and reduced repeat endoscopic interventions without increasing the risk of post-operative complications or mortality. Further prospective studies are required to clarify the utility of EUS in PBD and to establish its comparative safety and efficacy relative to ERCP.
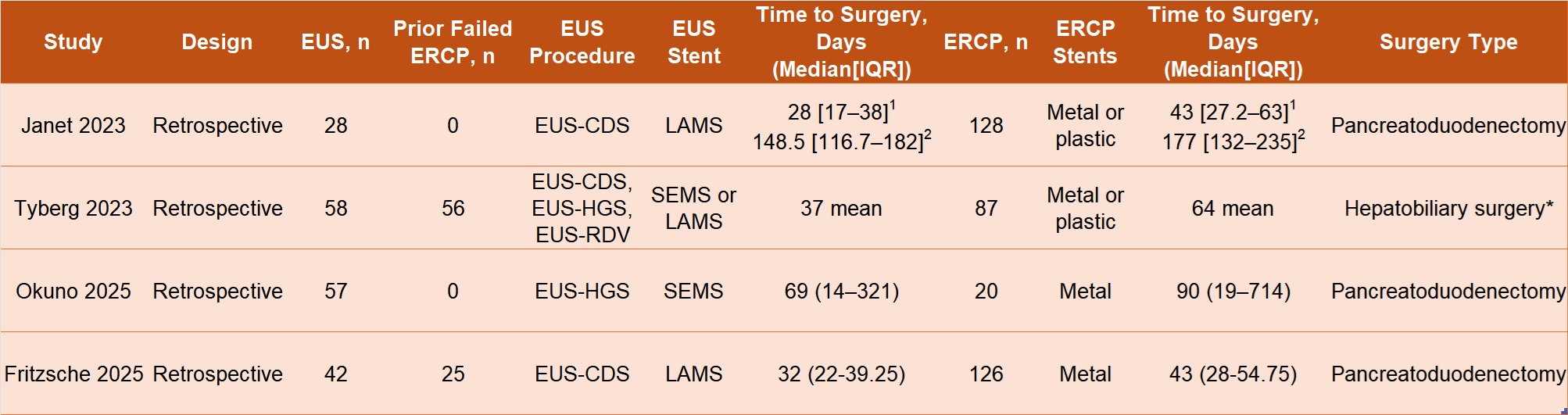
Figure: Table 1. Characteristics of the included studies. EUS-CDS: Endoscopic ultrasound-guided choledochoduodenostomy, EUS-HGS: Endoscopic ultrasound-guided hepaticogastrostomy, EUS-RDV: Endoscopic ultrasound-guided rendezvous, LAMS: Lumen apposing metal stent, SEMS: self-expanding metal stent
*Majority (97/143) were pancreatoduodenectomies. Other surgeries included diagnostic laparoscopy, biliary duct deviation, partial hepatectomy, and gastroenterostomy.
1No neoadjuvant therapy administered between endoscopic drainage and surgery
2Neoadjuvant therapy administered between endoscopic drainage and surgery
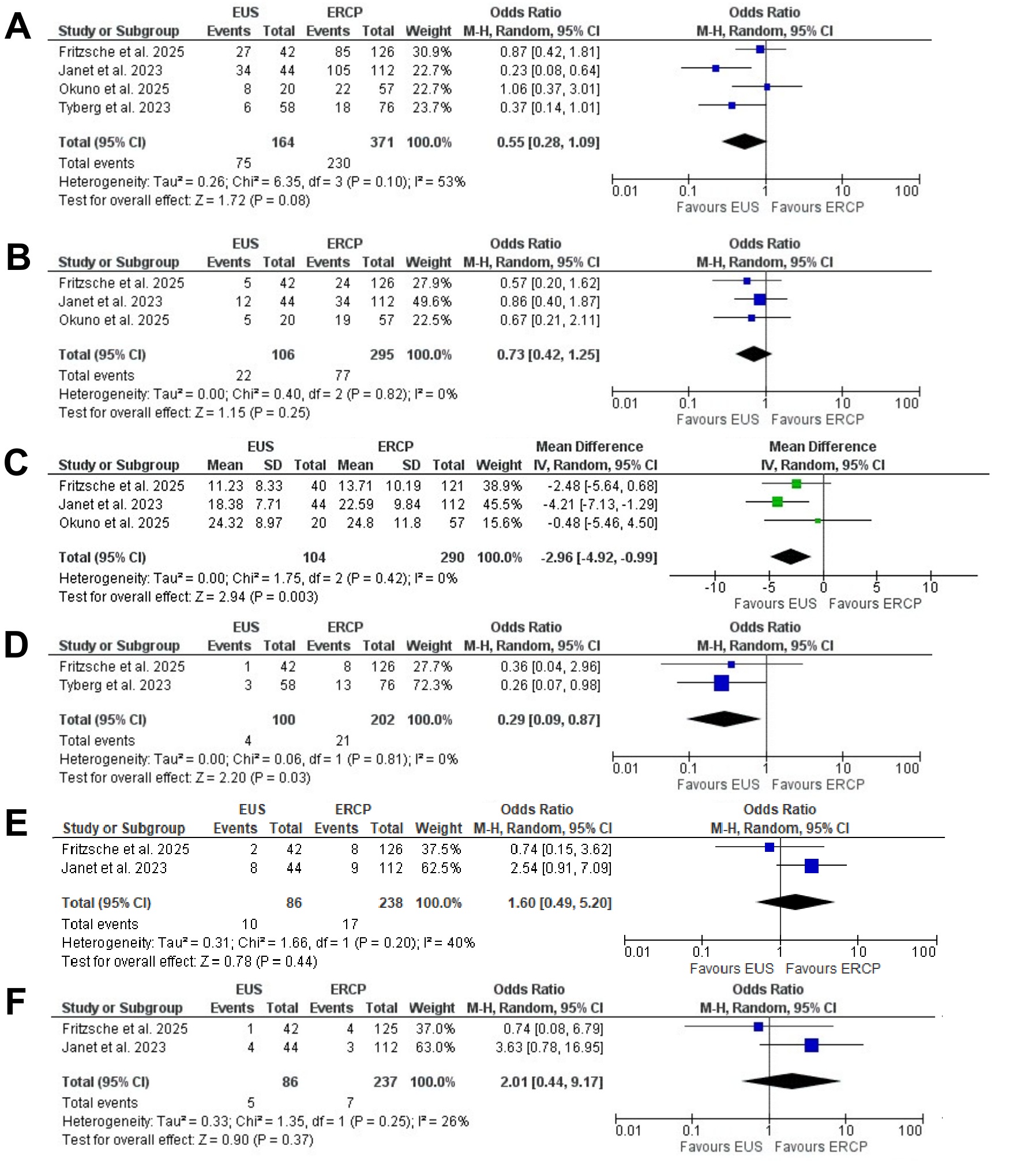
Figure: Figure 1. Forest plots showing the odds ratio/mean difference between the EUS and ERCP groups in terms of post-operative: A - Overall complications, B -Pancreatic fistula formation, C - Length of stay, D - Need for endoscopic re-intervention, E - Need for surgical intervention, F - Mortality
Disclosures:
Tareq Alsaleh indicated no relevant financial relationships.
Abdul Mohammed indicated no relevant financial relationships.
Mohamad Khaled Almujarkesh indicated no relevant financial relationships.
Saurabh Chandan indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
John George indicated no relevant financial relationships.
Maham Hayat indicated no relevant financial relationships.
Deepanshu Jain indicated no relevant financial relationships.
Natalie Cosgrove indicated no relevant financial relationships.
Kambiz Kadkhodayan indicated no relevant financial relationships.
Dennis Yang: 3D-Matrix – Consultant. Apollo Endosurgery – Consultant. ERBE – Consultant. Fujifilm – Consultant. Medtronic – Consultant. MicroTech – Consultant. Olympus – Consultant.
Muhammad Hasan: Boston Scientific – Consultant. MicroTech Endoscopy – Consultant. Olympus America – Consultant.
Mustafa Arain: Boston Scientific – Consultant. Cook Endoscopy – Consultant. Olympus – Consultant.
Tareq Alsaleh, MD1, Abdul Mohammed, MD2, Mohamad Khaled Almujarkesh, MD2, Saurabh Chandan, MD3, Babu P. Mohan, MD4, John George, MD2, Maham Hayat, MD3, Deepanshu Jain, MD3, Natalie Cosgrove, MD3, Kambiz Kadkhodayan, MD3, Dennis Yang, MD, FACG5, Muhammad Hasan, MD, FACG3, Mustafa Arain, MD3. P3543 - Endoscopic Ultrasound versus ERCP for Biliary Drainage Prior to Surgery: A Systematic Review and Meta-Analysis of Surgical Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine, AdventHealth Orlando, Orlando, FL; 2Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL; 3Center for Interventional Endoscopy, AdventHealth Orlando, Orlando, FL; 4Orlando Gastroenterology PA, Orlando, FL; 5Center for Interventional Endoscopic, AdventHealth Orlando, Orlando, FL
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) is usually used for preoperative biliary drainage (PBD) but carries risks of post-ERCP pancreatitis and stent-related complications, potentially delaying surgery. EUS-guided biliary drainage may reduce complications, but its impact on surgical exploration remains unclear. We conducted a systematic review and meta-analysis comparing the safety and efficacy of EUS and ERCP for PBD in terms of post-operative outcomes.
Methods: A systematic review of the literature from PubMed, EMBASE, and Scopus was conducted through April 2025, for studies comparing outcomes after pancreaticoduodenectomy and other surgeries when PBD is performed with EUS or ERCP. Outcomes of interest were surgical complications, need for reintervention, length of stay, and post-operative mortality. Standard meta-analysis methods were followed using the random-effects model. Treatment effect estimates were expressed as odds ratio (OR) or mean difference (MD) and 95% confidence interval (CI). Heterogeneity was assessed using the I2% statistic.
Results: Four retrospective studies were included that reported on 546 patients (54.4% males). 185 patients underwent EUS while 361 underwent ERCP. Three studies were multicenter, while on was single center. (Table 1).
There were trends towards decreased odds of post-operative complications (OR 0.55; 95% CI [0.28, 1.09], P=0.08) and pancreatic fistula formation (OR 0.73; 95% CI [0.42, 1.25], P=0.25) in the EUS group compared to the ERCP group that were not statistically significant. There was a statistically significant decrease in mean length of stay (MD -2.96; 95% CI [-4.92, -0.99], P=0.003) and odds of need for endoscopic reintervention (OR 0.29; 95% CI [0.09, 0.87], P=0.03) in the EUS group. There was no statistically significant difference in the odds of need for surgical reintervention (OR 1.60; 95% CI [0.49, 5.40], P=0.44) or post-operative mortality (OR 2.01; 95% CI [0.44, 9.17], P=0.37) between the two groups (Figure 1).
Discussion: Our meta-analysis demonstrates that in terms of post-surgical outcomes, EUS is a feasible and potentially safe alternative to ERCP for PBD. It was associated with shorter lengths of stay and reduced repeat endoscopic interventions without increasing the risk of post-operative complications or mortality. Further prospective studies are required to clarify the utility of EUS in PBD and to establish its comparative safety and efficacy relative to ERCP.
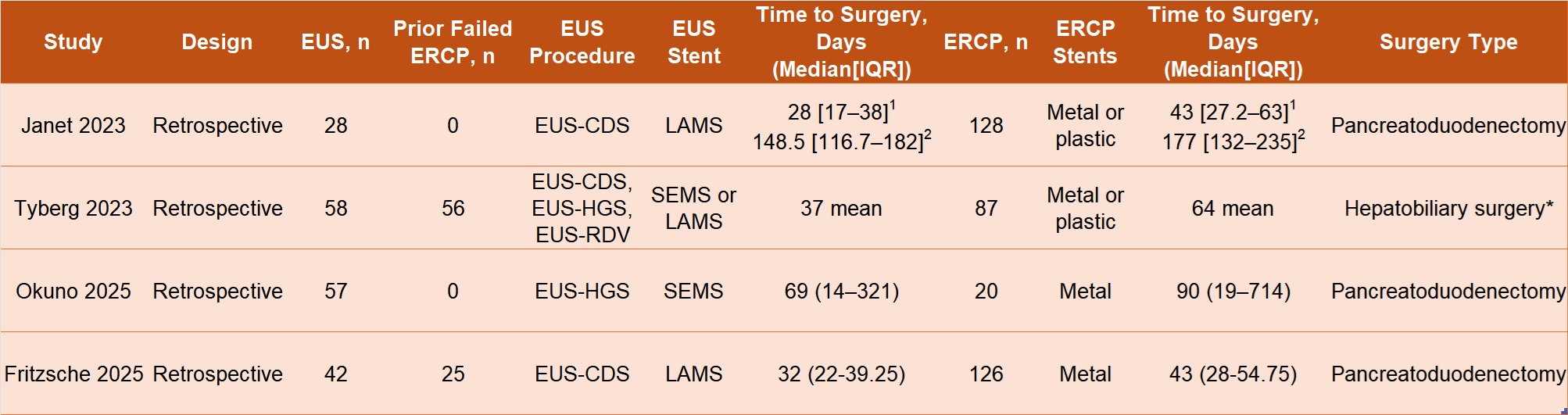
Figure: Table 1. Characteristics of the included studies. EUS-CDS: Endoscopic ultrasound-guided choledochoduodenostomy, EUS-HGS: Endoscopic ultrasound-guided hepaticogastrostomy, EUS-RDV: Endoscopic ultrasound-guided rendezvous, LAMS: Lumen apposing metal stent, SEMS: self-expanding metal stent
*Majority (97/143) were pancreatoduodenectomies. Other surgeries included diagnostic laparoscopy, biliary duct deviation, partial hepatectomy, and gastroenterostomy.
1No neoadjuvant therapy administered between endoscopic drainage and surgery
2Neoadjuvant therapy administered between endoscopic drainage and surgery
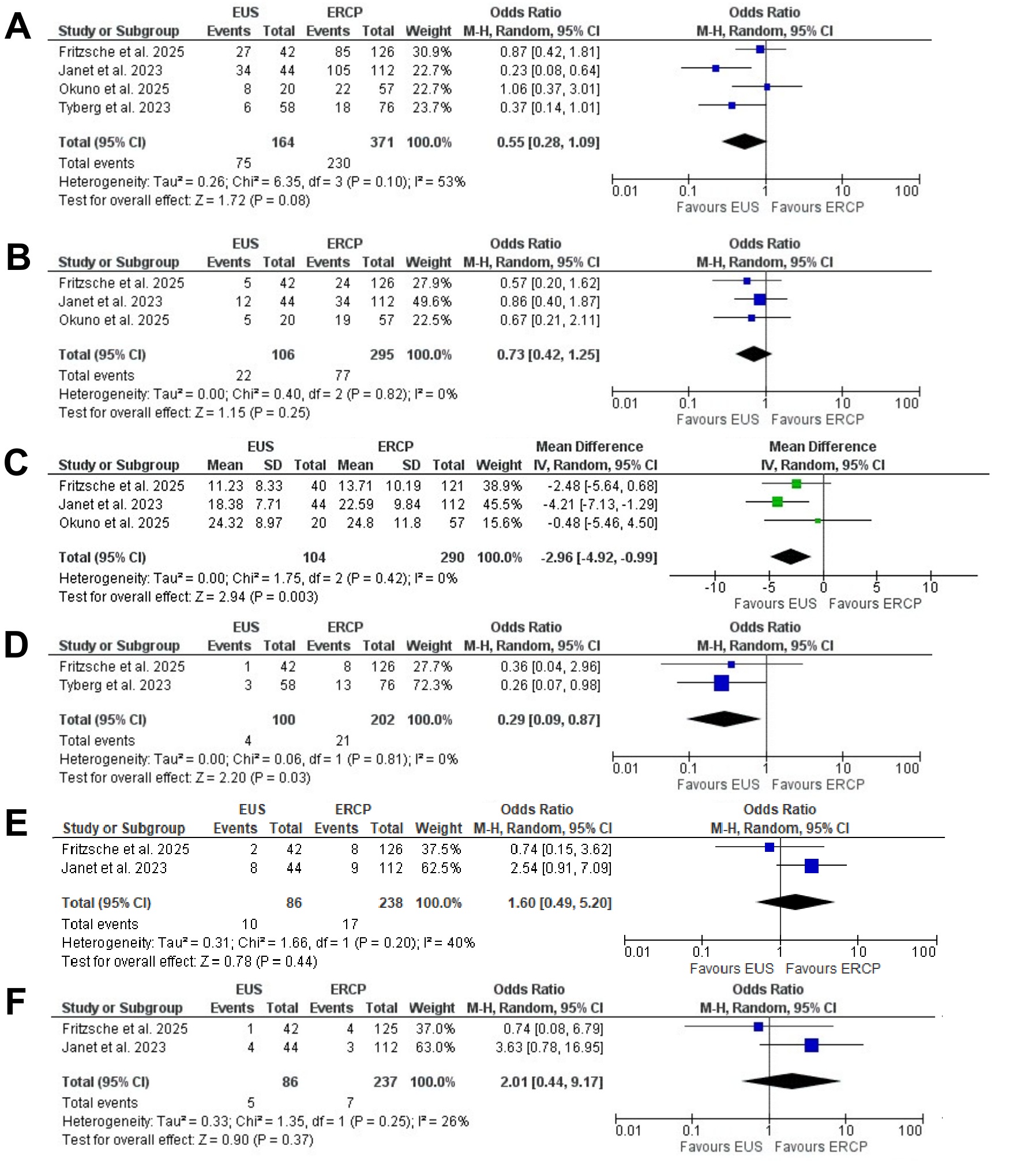
Figure: Figure 1. Forest plots showing the odds ratio/mean difference between the EUS and ERCP groups in terms of post-operative: A - Overall complications, B -Pancreatic fistula formation, C - Length of stay, D - Need for endoscopic re-intervention, E - Need for surgical intervention, F - Mortality
Disclosures:
Tareq Alsaleh indicated no relevant financial relationships.
Abdul Mohammed indicated no relevant financial relationships.
Mohamad Khaled Almujarkesh indicated no relevant financial relationships.
Saurabh Chandan indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
John George indicated no relevant financial relationships.
Maham Hayat indicated no relevant financial relationships.
Deepanshu Jain indicated no relevant financial relationships.
Natalie Cosgrove indicated no relevant financial relationships.
Kambiz Kadkhodayan indicated no relevant financial relationships.
Dennis Yang: 3D-Matrix – Consultant. Apollo Endosurgery – Consultant. ERBE – Consultant. Fujifilm – Consultant. Medtronic – Consultant. MicroTech – Consultant. Olympus – Consultant.
Muhammad Hasan: Boston Scientific – Consultant. MicroTech Endoscopy – Consultant. Olympus America – Consultant.
Mustafa Arain: Boston Scientific – Consultant. Cook Endoscopy – Consultant. Olympus – Consultant.
Tareq Alsaleh, MD1, Abdul Mohammed, MD2, Mohamad Khaled Almujarkesh, MD2, Saurabh Chandan, MD3, Babu P. Mohan, MD4, John George, MD2, Maham Hayat, MD3, Deepanshu Jain, MD3, Natalie Cosgrove, MD3, Kambiz Kadkhodayan, MD3, Dennis Yang, MD, FACG5, Muhammad Hasan, MD, FACG3, Mustafa Arain, MD3. P3543 - Endoscopic Ultrasound versus ERCP for Biliary Drainage Prior to Surgery: A Systematic Review and Meta-Analysis of Surgical Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
