Monday Poster Session
Category: Liver
P3631 - Metabolic Dysfunction-Associated Fatty Liver Disease as a Predictor of Critical Illness and Mortality in Heart Failure Hospitalizations: A Nationwide Inpatient Sample Study (2016-2022)
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Gedion Yilma Amdetsion, MD (he/him/his)
Cook County Health
Chicago, IL
Presenting Author(s)
Gedion Yilma Amdetsion, MD1, Chun-wei Pan, MD1, Hiwot G. Tebeje, MD, MPH2, Michael G. Tebeje, MD, MPH3, Shreyas Nandyal, MD1, Tsegabrhan Gebrewahid Weldegiorgis, MD4, Paras Singh Chandi, MBBS5, Seema Gandhi, MD6
1Cook County Health, Chicago, IL; 2Washington University in St. Louis, Saint Louis, MO; 3Washington University in St. Louis, St. Louis, MO; 4Yekatit 12 Hospital medical college, Addis Ababa, Adis Abeba, Ethiopia; 5Cook County Health and Hospital Systems, Chicago, IL; 6John H. Stroger Hospital of Cook Co, Chicago, IL
Introduction: MASLD, the hepatic manifestation of systemic metabolic derangement, affects up to one‑quarter of adults and frequently coexists with cardiovascular disease, but its influence on outcomes during acute heart‑failure (HF) hospitalizations isn’t conclusive.
Methods: We queried the 2016‑2022 Nationwide Inpatient Sample for adult discharges with a principal HF diagnosis. MASLD was identified with validated ICD‑10 codes. Design‑adjusted logistic regression assessed the association between MASLD and five inpatient outcomes—mechanical ventilation, acute kidney injury (AKI), new dialysis, vasopressor use, and in‑hospital death—controlling for demographics, lifestyle factors, and 14 comorbidities: smoking, diabetes, obesity, coronary artery disease, hypertension, dyslipidemia, atrial fibrillation, valvular disease, COPD, chronic kidney disease (CKD), anemia, alcohol use disorder, peripheral vascular disease, and sleep‑disordered breathing.
Results: Among 313 418 HF admissions, MASLD co‑occurred in 1.6 % of HF admissions. After full adjustment, MAFLD was independently associated with higher odds of mechanical ventilation (adjusted odds ratio [aOR] 1.13, 95 % CI 1.08–1.18), AKI (aOR 1.48, 95 % CI 1.45–1.51), vasopressor use (aOR 1.54, 95 % CI 1.40–1.70), and in‑hospital mortality (aOR 1.13, 95 % CI 1.07–1.19), all p< 0.001.
After full multivariable adjustment, hospitalizations with MASLD had a 0.6‑day longer median LOS than HF admissions without MAFLD (β = +0.62 days, 95 % CI 0.34–0.89; p < 0.001).
Discussion: Although present in only approximately 1 in 60 heart failure hospitalizations, MASLD is associated with a clinically significant increase in critical illness markers, prolonged hospital stay, and higher in-hospital mortality. The unexpected inverse association with dialysis initiation warrants further investigation. Systematic identification of MASLD in this population may aid in risk stratification, and future research can further explore its prognostic implications and underlying mechanisms.
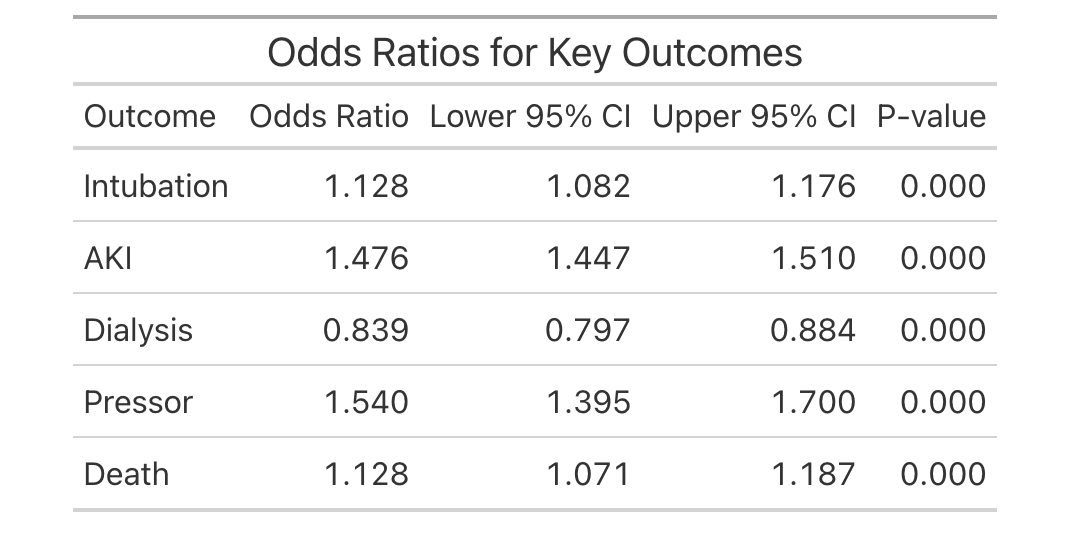
Figure: Fig. 1. Odds ratio for key outcomes
Disclosures:
Gedion Yilma Amdetsion indicated no relevant financial relationships.
Chun-wei Pan indicated no relevant financial relationships.
Hiwot Tebeje indicated no relevant financial relationships.
Michael Tebeje indicated no relevant financial relationships.
Shreyas Nandyal indicated no relevant financial relationships.
Tsegabrhan Gebrewahid Weldegiorgis indicated no relevant financial relationships.
Paras Singh Chandi indicated no relevant financial relationships.
Seema Gandhi indicated no relevant financial relationships.
Gedion Yilma Amdetsion, MD1, Chun-wei Pan, MD1, Hiwot G. Tebeje, MD, MPH2, Michael G. Tebeje, MD, MPH3, Shreyas Nandyal, MD1, Tsegabrhan Gebrewahid Weldegiorgis, MD4, Paras Singh Chandi, MBBS5, Seema Gandhi, MD6. P3631 - Metabolic Dysfunction-Associated Fatty Liver Disease as a Predictor of Critical Illness and Mortality in Heart Failure Hospitalizations: A Nationwide Inpatient Sample Study (2016-2022), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cook County Health, Chicago, IL; 2Washington University in St. Louis, Saint Louis, MO; 3Washington University in St. Louis, St. Louis, MO; 4Yekatit 12 Hospital medical college, Addis Ababa, Adis Abeba, Ethiopia; 5Cook County Health and Hospital Systems, Chicago, IL; 6John H. Stroger Hospital of Cook Co, Chicago, IL
Introduction: MASLD, the hepatic manifestation of systemic metabolic derangement, affects up to one‑quarter of adults and frequently coexists with cardiovascular disease, but its influence on outcomes during acute heart‑failure (HF) hospitalizations isn’t conclusive.
Methods: We queried the 2016‑2022 Nationwide Inpatient Sample for adult discharges with a principal HF diagnosis. MASLD was identified with validated ICD‑10 codes. Design‑adjusted logistic regression assessed the association between MASLD and five inpatient outcomes—mechanical ventilation, acute kidney injury (AKI), new dialysis, vasopressor use, and in‑hospital death—controlling for demographics, lifestyle factors, and 14 comorbidities: smoking, diabetes, obesity, coronary artery disease, hypertension, dyslipidemia, atrial fibrillation, valvular disease, COPD, chronic kidney disease (CKD), anemia, alcohol use disorder, peripheral vascular disease, and sleep‑disordered breathing.
Results: Among 313 418 HF admissions, MASLD co‑occurred in 1.6 % of HF admissions. After full adjustment, MAFLD was independently associated with higher odds of mechanical ventilation (adjusted odds ratio [aOR] 1.13, 95 % CI 1.08–1.18), AKI (aOR 1.48, 95 % CI 1.45–1.51), vasopressor use (aOR 1.54, 95 % CI 1.40–1.70), and in‑hospital mortality (aOR 1.13, 95 % CI 1.07–1.19), all p< 0.001.
After full multivariable adjustment, hospitalizations with MASLD had a 0.6‑day longer median LOS than HF admissions without MAFLD (β = +0.62 days, 95 % CI 0.34–0.89; p < 0.001).
Discussion: Although present in only approximately 1 in 60 heart failure hospitalizations, MASLD is associated with a clinically significant increase in critical illness markers, prolonged hospital stay, and higher in-hospital mortality. The unexpected inverse association with dialysis initiation warrants further investigation. Systematic identification of MASLD in this population may aid in risk stratification, and future research can further explore its prognostic implications and underlying mechanisms.
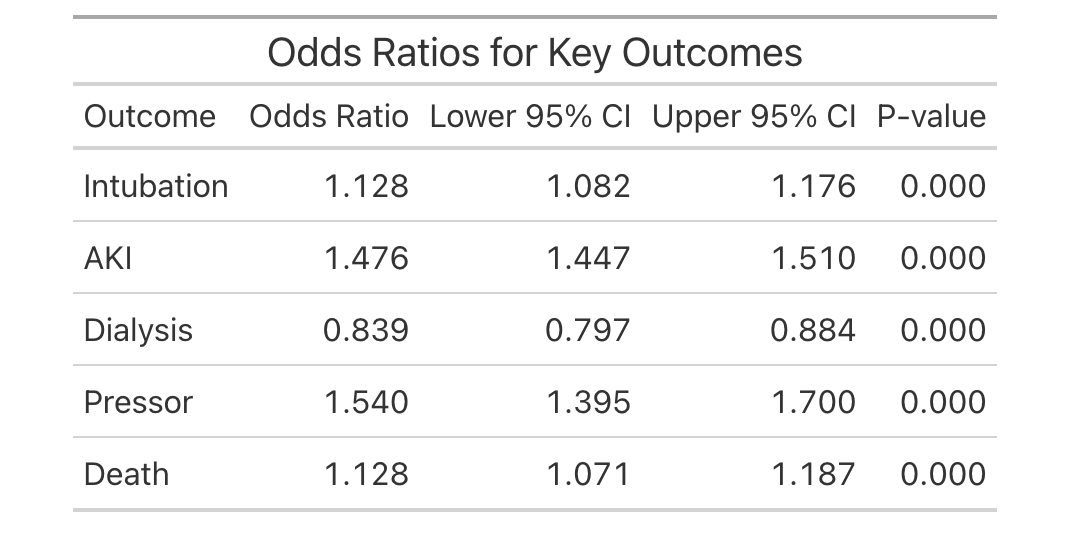
Figure: Fig. 1. Odds ratio for key outcomes
Disclosures:
Gedion Yilma Amdetsion indicated no relevant financial relationships.
Chun-wei Pan indicated no relevant financial relationships.
Hiwot Tebeje indicated no relevant financial relationships.
Michael Tebeje indicated no relevant financial relationships.
Shreyas Nandyal indicated no relevant financial relationships.
Tsegabrhan Gebrewahid Weldegiorgis indicated no relevant financial relationships.
Paras Singh Chandi indicated no relevant financial relationships.
Seema Gandhi indicated no relevant financial relationships.
Gedion Yilma Amdetsion, MD1, Chun-wei Pan, MD1, Hiwot G. Tebeje, MD, MPH2, Michael G. Tebeje, MD, MPH3, Shreyas Nandyal, MD1, Tsegabrhan Gebrewahid Weldegiorgis, MD4, Paras Singh Chandi, MBBS5, Seema Gandhi, MD6. P3631 - Metabolic Dysfunction-Associated Fatty Liver Disease as a Predictor of Critical Illness and Mortality in Heart Failure Hospitalizations: A Nationwide Inpatient Sample Study (2016-2022), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
