Monday Poster Session
Category: Liver
P3629 - Association Between Subclinical Hypothyroidism and Metabolic Dysfunction-Associated Steatotic Liver Disease: A Systematic Review and Meta-Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Gedion Yilma Amdetsion, MD (he/him/his)
Cook County Health
Chicago, IL
Presenting Author(s)
Gedion Yilma Amdetsion, MD1, Chun-wei Pan, MD1, Hiwot G. Tebeje, MD, MPH2, Abhin Sapkota, MBBS3, Shreyas Nandyal, MD1, Vikram Kotwal, MD3
1Cook County Health, Chicago, IL; 2Washington University in St. Louis, Saint Louis, MO; 3John H. Stroger, Jr. Hospital of Cook County, Chicago, IL
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD) is a prevalent condition that may progress to cirrhosis and hepatocellular carcinoma. While overt hypothyroidism has been linked to MASLD, the relationship between subclinical hypothyroidism (SCH) and MASLD remains controversial.
Methods: We systematically searched PubMed, Embase, Cochrane, ClinicalTrials.gov, and Web of Science up to 12 February 2025 for studies evaluating the association between SCH and MASLD. Random-effects meta-analyses were performed on eligible cross-sectional and longitudinal studies. Heterogeneity was assessed using the I² statistic, and publication bias was evaluated with funnel plots and Egger’s test. Sensitivity analyses, including leave-one-out approaches and trim-and-fill methods, were conducted to gauge robustness.
Results: After examining the titles and abstracts of these publications and excluding duplicates, we identified 191 potentially eligible studies from five large electronic databases (PubMed, Web of Science, Embase, Cochrane, clinicaltrials.gov) from the inception to February 22, 2025. After comparing those 191 studies with our inclusion and exclusion criteria, we ended up selecting Ten high-quality, peer-reviewed studies involving 75,618 patients were included (six cross-sectional, four longitudinal). In cross-sectional analyses (n=40,063), SCH was associated with a 42% higher odds of MASLD (pooled OR=1.42, 95% CI 1.15–1.60; I²=0%). Among four longitudinal studies (n=31,541), SCH conferred a 65% increased risk of incident MASLD (pooled HR=1.65, 95% CI 1.02–2.67) but with substantial heterogeneity (I²=84%). Egger’s regression showed a significantly nonzero intercept (β₁ = 3.00, z = 2.38, p = 0.0171), and the funnel plot was visibly asymmetric, pointing to small‐study or publication bias. Therefore a leave one out test was done by leaving out one of the studies that improved both the effect size (HR=1.88, 95% CI 1.45–2.44) and reduced heterogeneity (I²=0%).
Discussion: This meta-analysis provides evidence that SCH is associated with both higher odds of prevalent MASLD and increased risk of incident MASLD. Clinicians should consider routine screening for MASLD in patients with SCH and vice versa. Future research is needed to determine whether therapeutic interventions for SCH can prevent or slow MASLD progression.
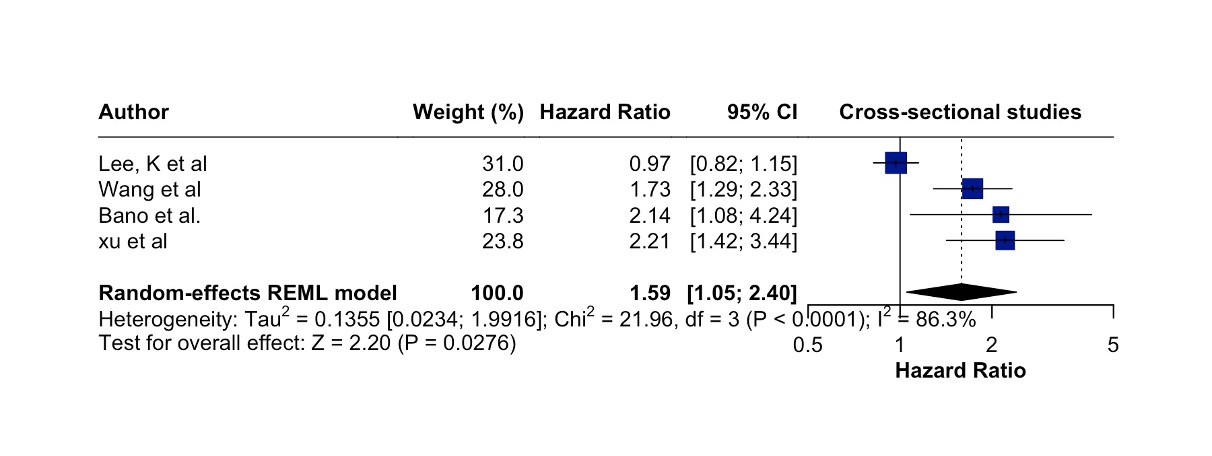
Figure: Fig. 1. Forrest plot of longitudinal studies showing relationship between MASLD and Subclinical hypothyroidism
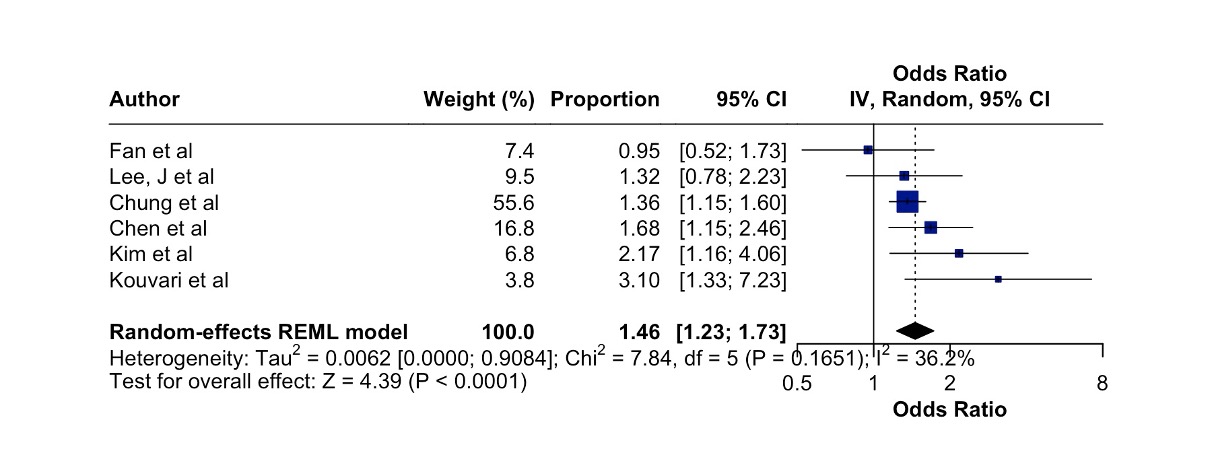
Figure: Fig 2. Forrest plot of cross-sectional studies showing the relationship between Subclinical hypothyroidism and MASLD
Disclosures:
Gedion Yilma Amdetsion indicated no relevant financial relationships.
Chun-wei Pan indicated no relevant financial relationships.
Hiwot Tebeje indicated no relevant financial relationships.
Abhin Sapkota indicated no relevant financial relationships.
Shreyas Nandyal indicated no relevant financial relationships.
Vikram Kotwal indicated no relevant financial relationships.
Gedion Yilma Amdetsion, MD1, Chun-wei Pan, MD1, Hiwot G. Tebeje, MD, MPH2, Abhin Sapkota, MBBS3, Shreyas Nandyal, MD1, Vikram Kotwal, MD3. P3629 - Association Between Subclinical Hypothyroidism and Metabolic Dysfunction-Associated Steatotic Liver Disease: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cook County Health, Chicago, IL; 2Washington University in St. Louis, Saint Louis, MO; 3John H. Stroger, Jr. Hospital of Cook County, Chicago, IL
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD) is a prevalent condition that may progress to cirrhosis and hepatocellular carcinoma. While overt hypothyroidism has been linked to MASLD, the relationship between subclinical hypothyroidism (SCH) and MASLD remains controversial.
Methods: We systematically searched PubMed, Embase, Cochrane, ClinicalTrials.gov, and Web of Science up to 12 February 2025 for studies evaluating the association between SCH and MASLD. Random-effects meta-analyses were performed on eligible cross-sectional and longitudinal studies. Heterogeneity was assessed using the I² statistic, and publication bias was evaluated with funnel plots and Egger’s test. Sensitivity analyses, including leave-one-out approaches and trim-and-fill methods, were conducted to gauge robustness.
Results: After examining the titles and abstracts of these publications and excluding duplicates, we identified 191 potentially eligible studies from five large electronic databases (PubMed, Web of Science, Embase, Cochrane, clinicaltrials.gov) from the inception to February 22, 2025. After comparing those 191 studies with our inclusion and exclusion criteria, we ended up selecting Ten high-quality, peer-reviewed studies involving 75,618 patients were included (six cross-sectional, four longitudinal). In cross-sectional analyses (n=40,063), SCH was associated with a 42% higher odds of MASLD (pooled OR=1.42, 95% CI 1.15–1.60; I²=0%). Among four longitudinal studies (n=31,541), SCH conferred a 65% increased risk of incident MASLD (pooled HR=1.65, 95% CI 1.02–2.67) but with substantial heterogeneity (I²=84%). Egger’s regression showed a significantly nonzero intercept (β₁ = 3.00, z = 2.38, p = 0.0171), and the funnel plot was visibly asymmetric, pointing to small‐study or publication bias. Therefore a leave one out test was done by leaving out one of the studies that improved both the effect size (HR=1.88, 95% CI 1.45–2.44) and reduced heterogeneity (I²=0%).
Discussion: This meta-analysis provides evidence that SCH is associated with both higher odds of prevalent MASLD and increased risk of incident MASLD. Clinicians should consider routine screening for MASLD in patients with SCH and vice versa. Future research is needed to determine whether therapeutic interventions for SCH can prevent or slow MASLD progression.
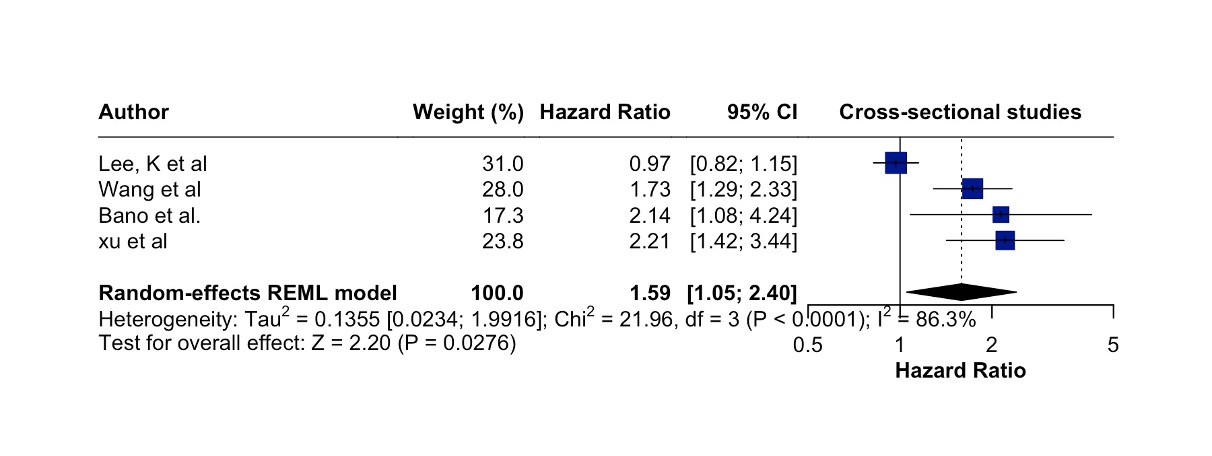
Figure: Fig. 1. Forrest plot of longitudinal studies showing relationship between MASLD and Subclinical hypothyroidism
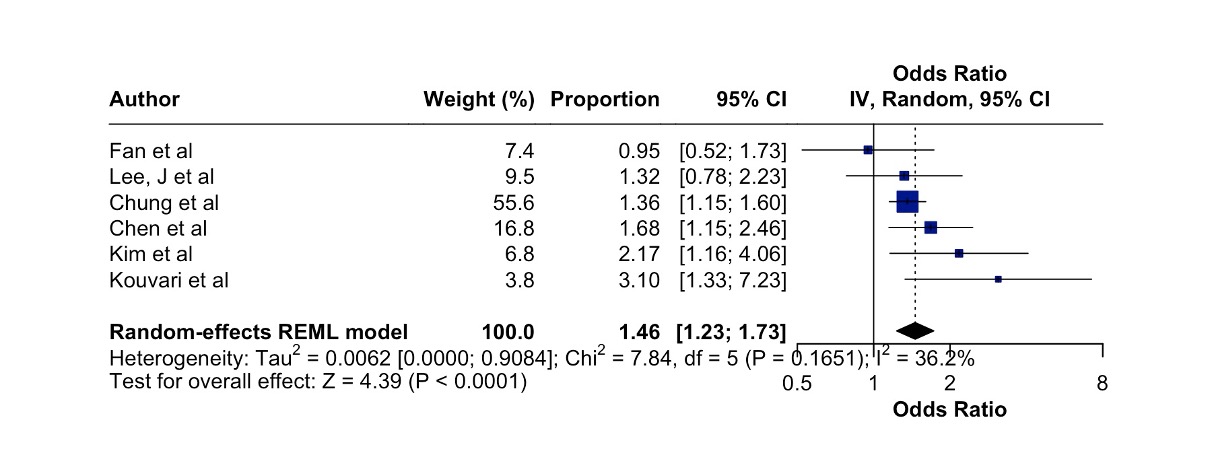
Figure: Fig 2. Forrest plot of cross-sectional studies showing the relationship between Subclinical hypothyroidism and MASLD
Disclosures:
Gedion Yilma Amdetsion indicated no relevant financial relationships.
Chun-wei Pan indicated no relevant financial relationships.
Hiwot Tebeje indicated no relevant financial relationships.
Abhin Sapkota indicated no relevant financial relationships.
Shreyas Nandyal indicated no relevant financial relationships.
Vikram Kotwal indicated no relevant financial relationships.
Gedion Yilma Amdetsion, MD1, Chun-wei Pan, MD1, Hiwot G. Tebeje, MD, MPH2, Abhin Sapkota, MBBS3, Shreyas Nandyal, MD1, Vikram Kotwal, MD3. P3629 - Association Between Subclinical Hypothyroidism and Metabolic Dysfunction-Associated Steatotic Liver Disease: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
