Monday Poster Session
Category: Liver
P3628 - Survival Following Transjugular Intrahepatic Portosystemic Shunt in MASLD and Non-MASLD Cirrhosis: A Retrospective Study From 2000-2023
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Amish M. Khan, MD, MSCI (he/him/his)
University of Pittsburgh Medical Center
Pittsburgh, PA
Presenting Author(s)
Amish M. Khan, MD, MSCI1, Nadeen Sarsour, MD1, Ricardo J. Cabello, MD2, Lee Vareles, MD3, Mordechai Rabinovitz, MD1, Paula Novelli, MD1, Philip Orons, DO1, Shahid Malik, MD1
1University of Pittsburgh Medical Center, Pittsburgh, PA; 2Inova Health System, Fairfax, VA; 3University of Pittsburgh Medical Center, Portland, OR
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD) is the leading cause of chronic liver disease globally, with a growing number of patients progressing to cirrhosis. Transjugular intrahepatic portsytemic shunt (TIPS) is a key intervention for managing complications of portal hypertension in cirrhosis. However, the impact of cirrhosis etiology on post-TIPS survival remains unexplored. Given the distinct cardiometabolic profiles of MASLD patients, understanding the impact of MASLD on survival following TIPS is critical for clinical decision-making.
Methods: We conducted a retrospective cohort study of 877 adults with cirrhosis undergoing TIPS at an academic center from 2000 to 2023. Cirrhosis etiology was classified as MASLD or non-MASLD. The primary outcome was overall survival after TIPS placement. Covariates included demographics, comorbidities, medications, decompensating events, indication for TIPS, mean pre- and post-TIPS gradient, stent diameter, post-TIPS complications. Overall survival was assessed using Kaplan-Meier analysis and multivariate Cox regression.
Results: Among the 877 patients, the mean (±SD) age was 55 (12). The cohort was predominantly male 542 (62%) and white 831 (94%). 193 (22%) patients had MASLD. MASLD patients were older (61 vs. 53 years; OR 1.07, 95% CI 1.06 to 1.09), more frequently female (56% vs. 33%; OR 2.6, 95% CI 1.9 to 3.5), had higher rates of metabolic comorbidities including diabetes mellitus (78% vs. 22%; OR 12.7, 95% CI 8.7 to 18.8), hypertension (69% vs. 32%; OR 4.8, 95% CI: 3.4 to 6.9), and obesity (76% vs. 25%; OR 9.3, 95% CI: 6.5 to 13.7) (Table 1). In adjusted Cox analysis, MASLD was not independently associated with mortality (aHR 0.88, 95% CI: 0.68 to 1.1). Independent predictors of mortality included age (aHR 1.03, 95% CI: 1.02 to 1.04), MELD score (aHR 1.06, 95% CI: 1.05 to 1.08), and Child-Pugh class (C vs. A: aHR 2.7, 95% CI: 1.3 to 5.4).
Discussion: Despite a greater burden of cardiometabolic comorbidity, MASLD etiology did not confer worse survival post-TIPS. These findings support the use of TIPS in appropriately selected MASLD patients and suggest that cirrhosis severity, rather than etiology, may drive differences in outcomes. As MASLD prevalence continues to rise globally, these results offer important guidance for TIPS referral.
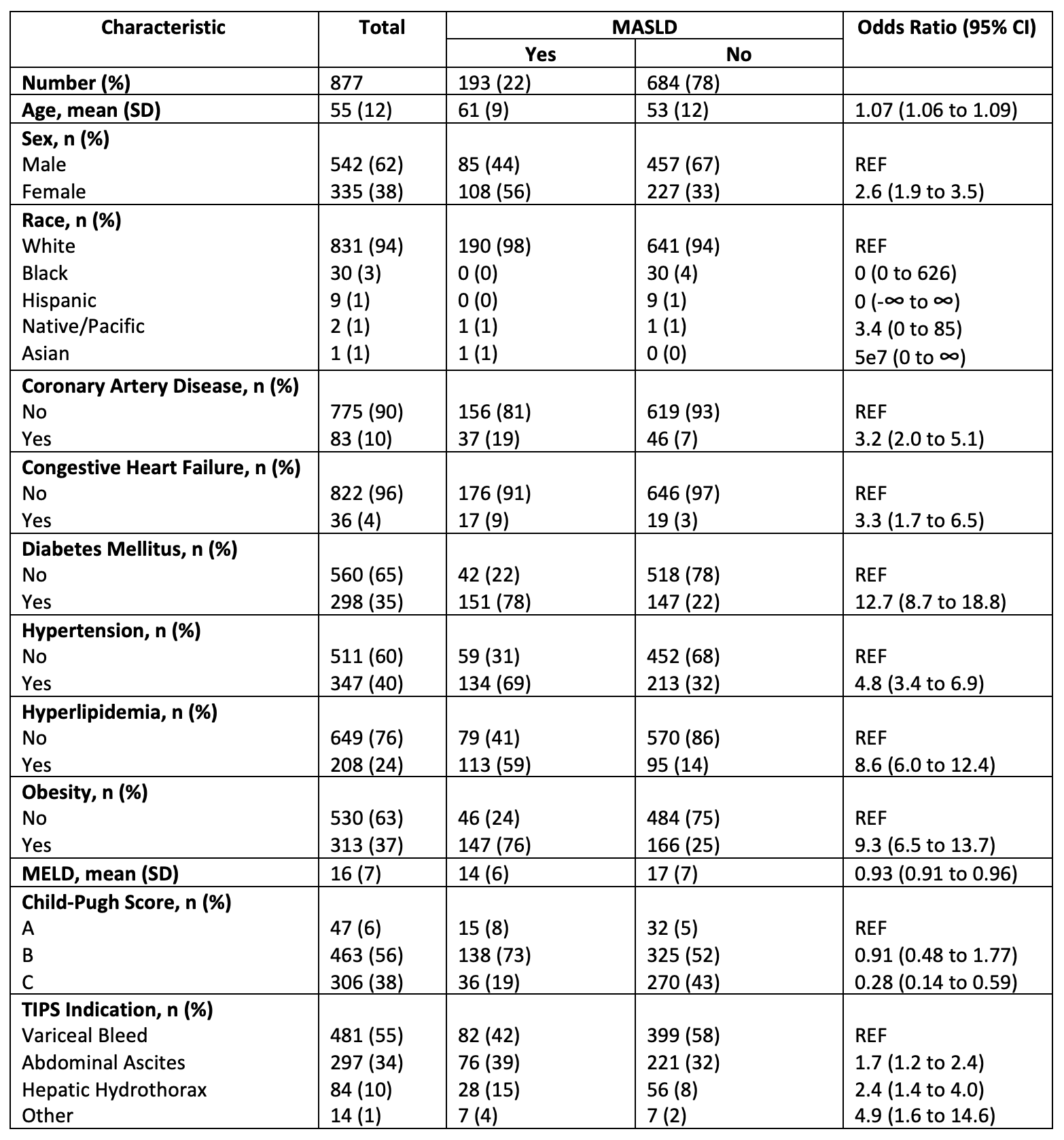
Figure: Figure 1. Kaplan-Meier survival curves comparing MASLD (blue) and non-MASLD (red) patients following TIPS placement. The MASLD group illustrated marginally higher survival probability across time, but the curves remained broadly similar without meaningful divergence (Log-Rank p = 0.1) . The number at risk is shown at 50-month intervals.
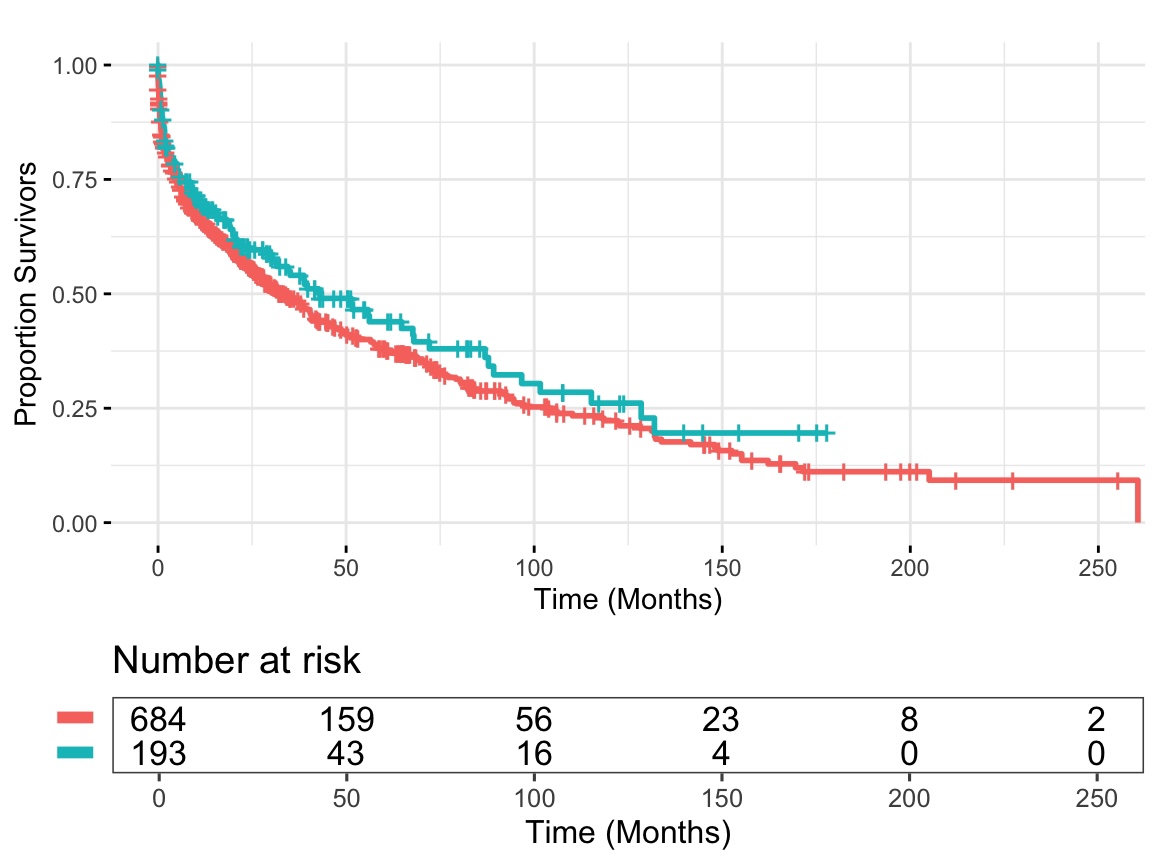
Figure: Table 1. Description of baseline demographic and clinical characteristics of patients with and without MASLD. Odds ratios (OR) with 95% confidence intervals (CI) reflect the association between each covariate and the presence of MASLD. Reference categories (REF) are noted. Table is abridged for brevity.
Disclosures:
Amish Khan indicated no relevant financial relationships.
Nadeen Sarsour indicated no relevant financial relationships.
Ricardo Cabello indicated no relevant financial relationships.
Lee Vareles indicated no relevant financial relationships.
Mordechai Rabinovitz indicated no relevant financial relationships.
Paula Novelli indicated no relevant financial relationships.
Philip Orons indicated no relevant financial relationships.
Shahid Malik indicated no relevant financial relationships.
Amish M. Khan, MD, MSCI1, Nadeen Sarsour, MD1, Ricardo J. Cabello, MD2, Lee Vareles, MD3, Mordechai Rabinovitz, MD1, Paula Novelli, MD1, Philip Orons, DO1, Shahid Malik, MD1. P3628 - Survival Following Transjugular Intrahepatic Portosystemic Shunt in MASLD and Non-MASLD Cirrhosis: A Retrospective Study From 2000-2023, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Pittsburgh Medical Center, Pittsburgh, PA; 2Inova Health System, Fairfax, VA; 3University of Pittsburgh Medical Center, Portland, OR
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD) is the leading cause of chronic liver disease globally, with a growing number of patients progressing to cirrhosis. Transjugular intrahepatic portsytemic shunt (TIPS) is a key intervention for managing complications of portal hypertension in cirrhosis. However, the impact of cirrhosis etiology on post-TIPS survival remains unexplored. Given the distinct cardiometabolic profiles of MASLD patients, understanding the impact of MASLD on survival following TIPS is critical for clinical decision-making.
Methods: We conducted a retrospective cohort study of 877 adults with cirrhosis undergoing TIPS at an academic center from 2000 to 2023. Cirrhosis etiology was classified as MASLD or non-MASLD. The primary outcome was overall survival after TIPS placement. Covariates included demographics, comorbidities, medications, decompensating events, indication for TIPS, mean pre- and post-TIPS gradient, stent diameter, post-TIPS complications. Overall survival was assessed using Kaplan-Meier analysis and multivariate Cox regression.
Results: Among the 877 patients, the mean (±SD) age was 55 (12). The cohort was predominantly male 542 (62%) and white 831 (94%). 193 (22%) patients had MASLD. MASLD patients were older (61 vs. 53 years; OR 1.07, 95% CI 1.06 to 1.09), more frequently female (56% vs. 33%; OR 2.6, 95% CI 1.9 to 3.5), had higher rates of metabolic comorbidities including diabetes mellitus (78% vs. 22%; OR 12.7, 95% CI 8.7 to 18.8), hypertension (69% vs. 32%; OR 4.8, 95% CI: 3.4 to 6.9), and obesity (76% vs. 25%; OR 9.3, 95% CI: 6.5 to 13.7) (Table 1). In adjusted Cox analysis, MASLD was not independently associated with mortality (aHR 0.88, 95% CI: 0.68 to 1.1). Independent predictors of mortality included age (aHR 1.03, 95% CI: 1.02 to 1.04), MELD score (aHR 1.06, 95% CI: 1.05 to 1.08), and Child-Pugh class (C vs. A: aHR 2.7, 95% CI: 1.3 to 5.4).
Discussion: Despite a greater burden of cardiometabolic comorbidity, MASLD etiology did not confer worse survival post-TIPS. These findings support the use of TIPS in appropriately selected MASLD patients and suggest that cirrhosis severity, rather than etiology, may drive differences in outcomes. As MASLD prevalence continues to rise globally, these results offer important guidance for TIPS referral.
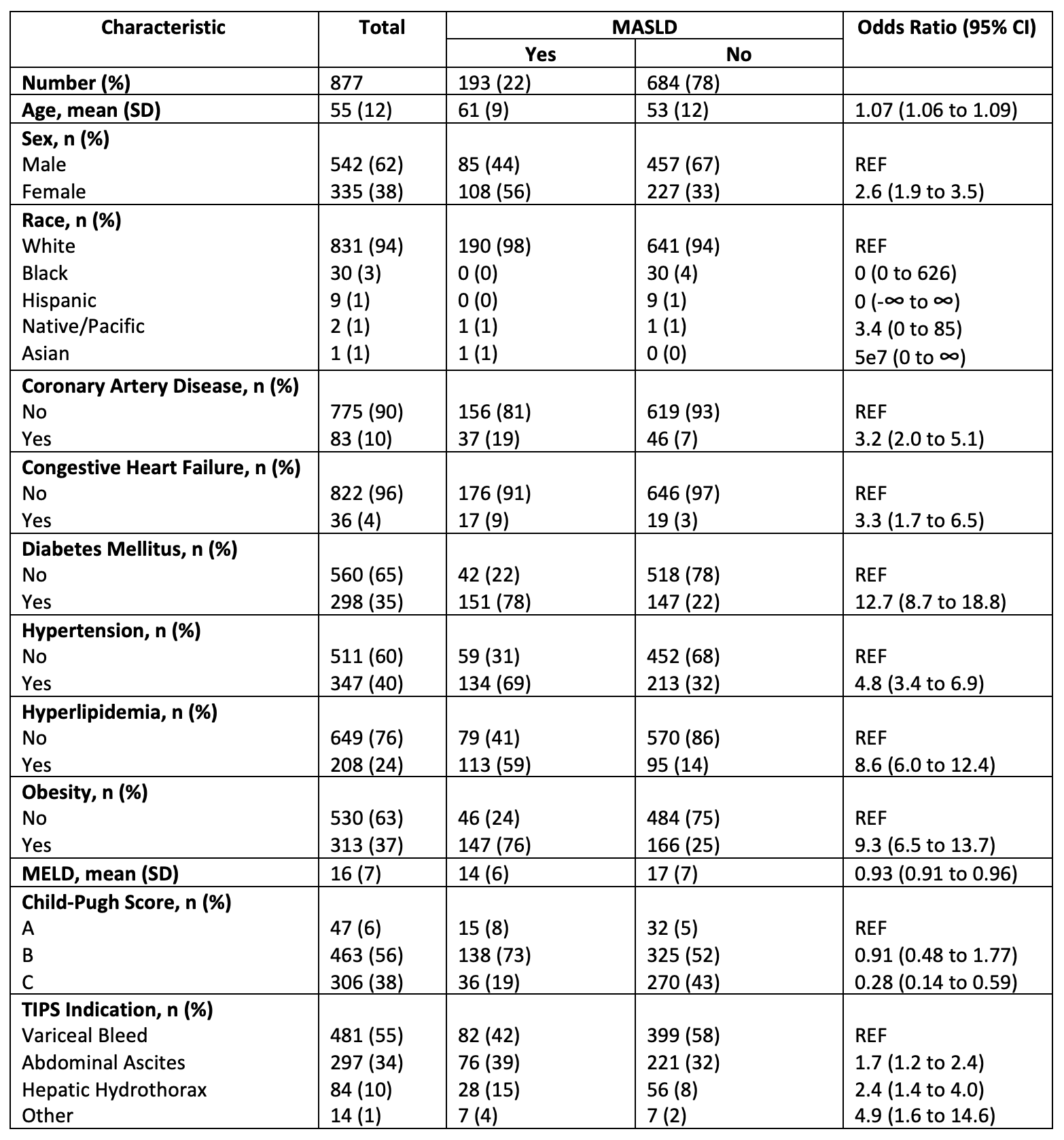
Figure: Figure 1. Kaplan-Meier survival curves comparing MASLD (blue) and non-MASLD (red) patients following TIPS placement. The MASLD group illustrated marginally higher survival probability across time, but the curves remained broadly similar without meaningful divergence (Log-Rank p = 0.1) . The number at risk is shown at 50-month intervals.
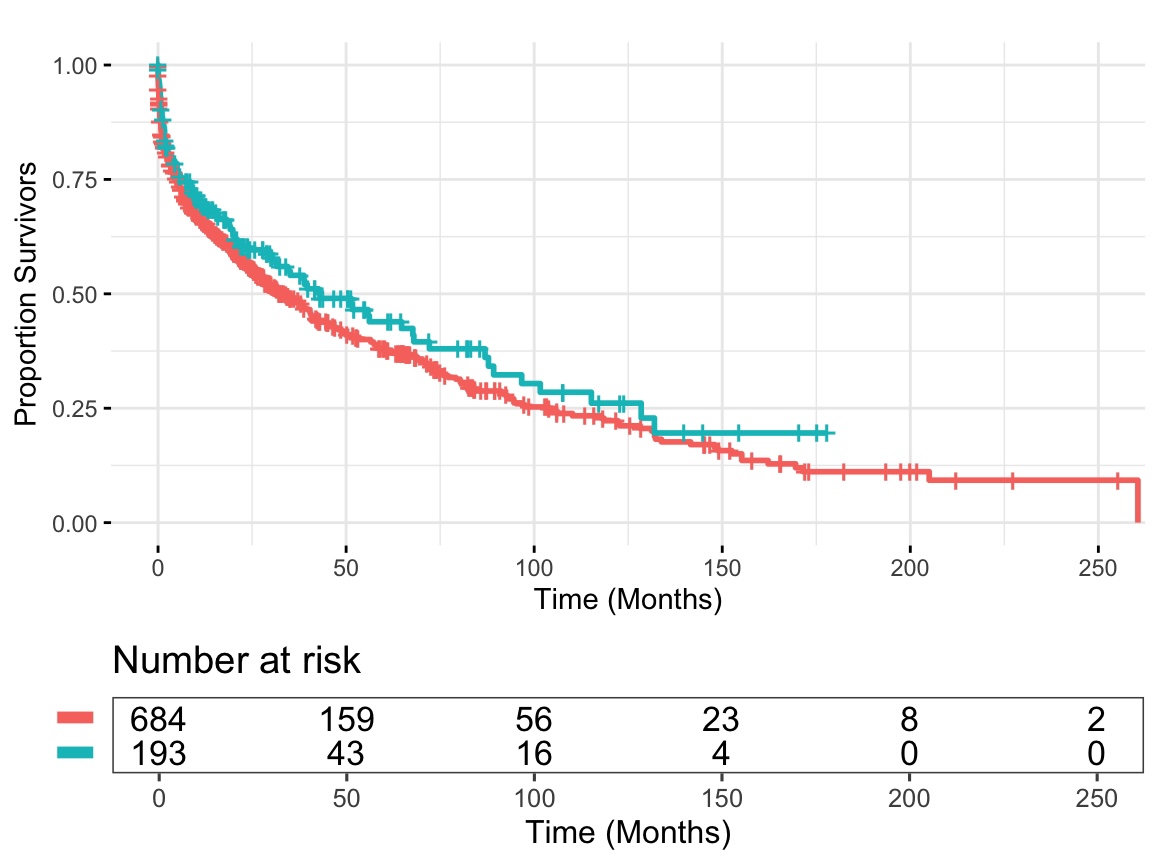
Figure: Table 1. Description of baseline demographic and clinical characteristics of patients with and without MASLD. Odds ratios (OR) with 95% confidence intervals (CI) reflect the association between each covariate and the presence of MASLD. Reference categories (REF) are noted. Table is abridged for brevity.
Disclosures:
Amish Khan indicated no relevant financial relationships.
Nadeen Sarsour indicated no relevant financial relationships.
Ricardo Cabello indicated no relevant financial relationships.
Lee Vareles indicated no relevant financial relationships.
Mordechai Rabinovitz indicated no relevant financial relationships.
Paula Novelli indicated no relevant financial relationships.
Philip Orons indicated no relevant financial relationships.
Shahid Malik indicated no relevant financial relationships.
Amish M. Khan, MD, MSCI1, Nadeen Sarsour, MD1, Ricardo J. Cabello, MD2, Lee Vareles, MD3, Mordechai Rabinovitz, MD1, Paula Novelli, MD1, Philip Orons, DO1, Shahid Malik, MD1. P3628 - Survival Following Transjugular Intrahepatic Portosystemic Shunt in MASLD and Non-MASLD Cirrhosis: A Retrospective Study From 2000-2023, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

