Monday Poster Session
Category: Liver
P3722 - Nosocomial Spontaneous Bacterial Peritonitis Is Associated With Increased In-Hospital Mortality Compared to Community-Acquired Spontaneous Bacterial Peritonitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- LL
Laura Lavette, MD (she/her/hers)
University of Virginia Medical Center
Charlottesville, VA
Presenting Author(s)
Laura Lavette, MD, Nicolas Intagliata, MD, Zachary Henry, MD
University of Virginia Medical Center, Charlottesville, VA
Introduction: Spontaneous bacterial peritonitis (SBP) is one of the most common causes of infection in decompensated cirrhosis and is associated with high morbidity and mortality. Nosocomial infections have been associated with increased mortality in studies conducted in Europe and Asia; however, data are limited for patients in the United States (US). Through a retrospective analysis of a US cohort, we examined the relative impact of nosocomial SBP (n-SBP) compared to community acquired SBP (ca-SBP) on mortality.
Methods: Adult patients with decompensated cirrhosis and SBP were retrospectively enrolled over an 8-year period at a tertiary care hospital. SBP was defined as ascites fluid with >250 PMN/mm3 without an alternative explanation for peritonitis. Nosocomial infection was defined as SBP occurring greater than 48 hours after hospitalization. Significant predictors on univariable analysis (p >0.05) were combined in a multivariable cox-proportional hazards (CPH) model to assess independent predictors of mortality.
Results: Of 1048 patients with cirrhosis, 213 met criteria for SBP: 160 cases with ca-SBP and 53 with n-SBP. There were no significant differences in age, gender, Model for End-Stage Liver Disease (MELD), hepatocellular carcinoma (HCC), or SBP prophylaxis between groups. The ca-SBP group ascitic fluid studies revealed higher segmented cell count (1370 vs 559, p< 0.001) and culture positivity (32% vs 8%, p< 0.001). Patients in the ca-SBP group had significantly lower length of stay (LOS), in-hospital, and 30-day mortality. However, there was no significant difference in 90-day, 6-month, or 1-year mortality between groups. On multivariable analysis, n-SBP, MELD score, and admission to the intensive care unit (ICU) were independent predictors of in-hospital mortality while only MELD score and admission to ICU were independent predictors at 30 days.
Discussion: Our results suggest that n-SBP increases the risk of in-hospital mortality but thereafter the mortality effects wane. These results are disparate from those of other countries in which n-SBP has been suggested to have a larger impact on mortality. Due to the retrospective nature of this study, it is difficult to isolate the exact impact of antibiotic choices and multidrug resistant organisms on in-hospital mortality. In the future, a prospective, multi-center trial should be considered to further explore the risk of n-SBP in a US population.
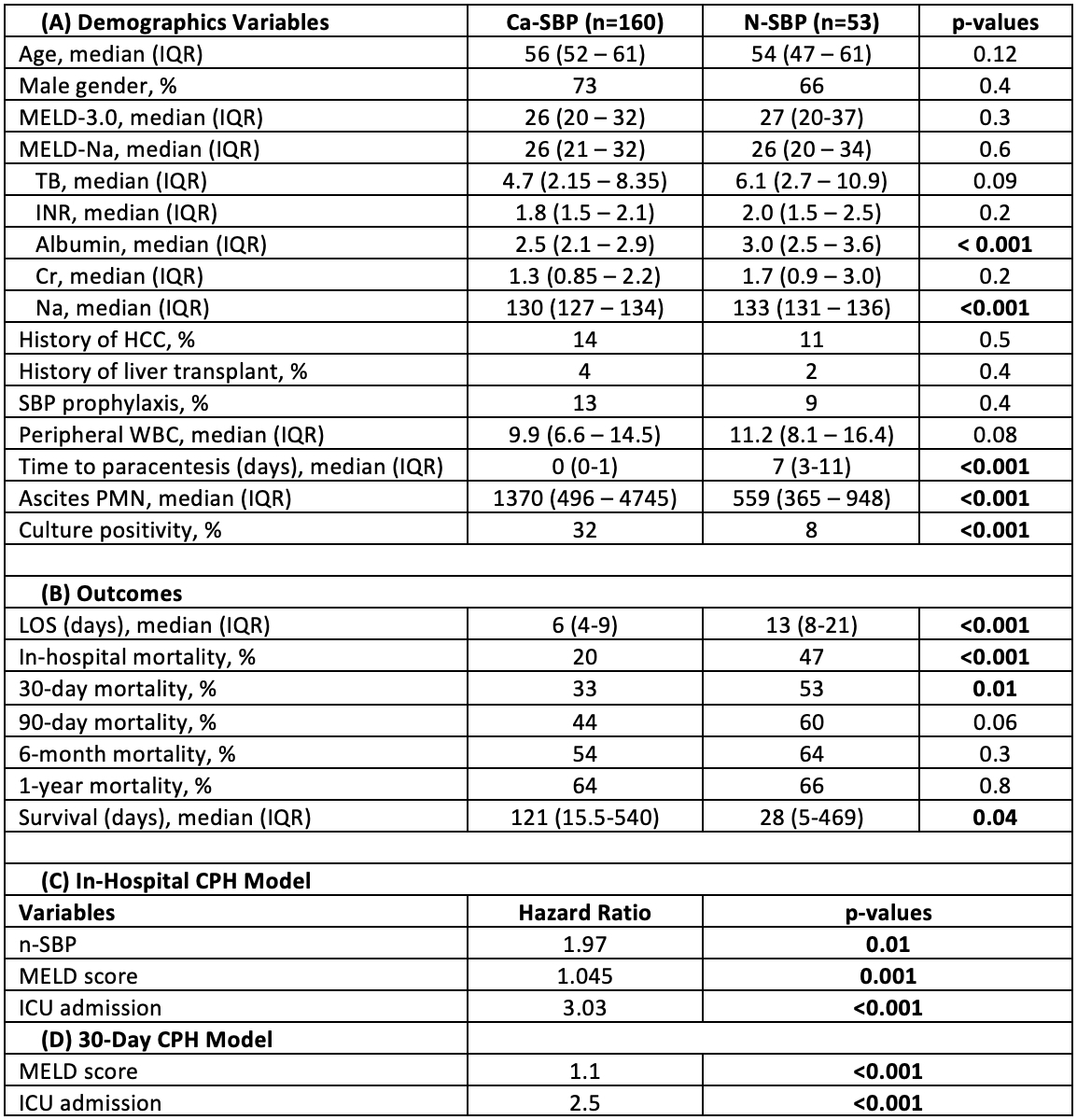
Figure: Demographic (A) and outcome (B) data compared between ca-SBP and n-SBP groups with associated p-values. Cox-Proportional Hazards Models for in-hospital (C) and 30-day (D) mortality with associated hazard ratios and p-values.
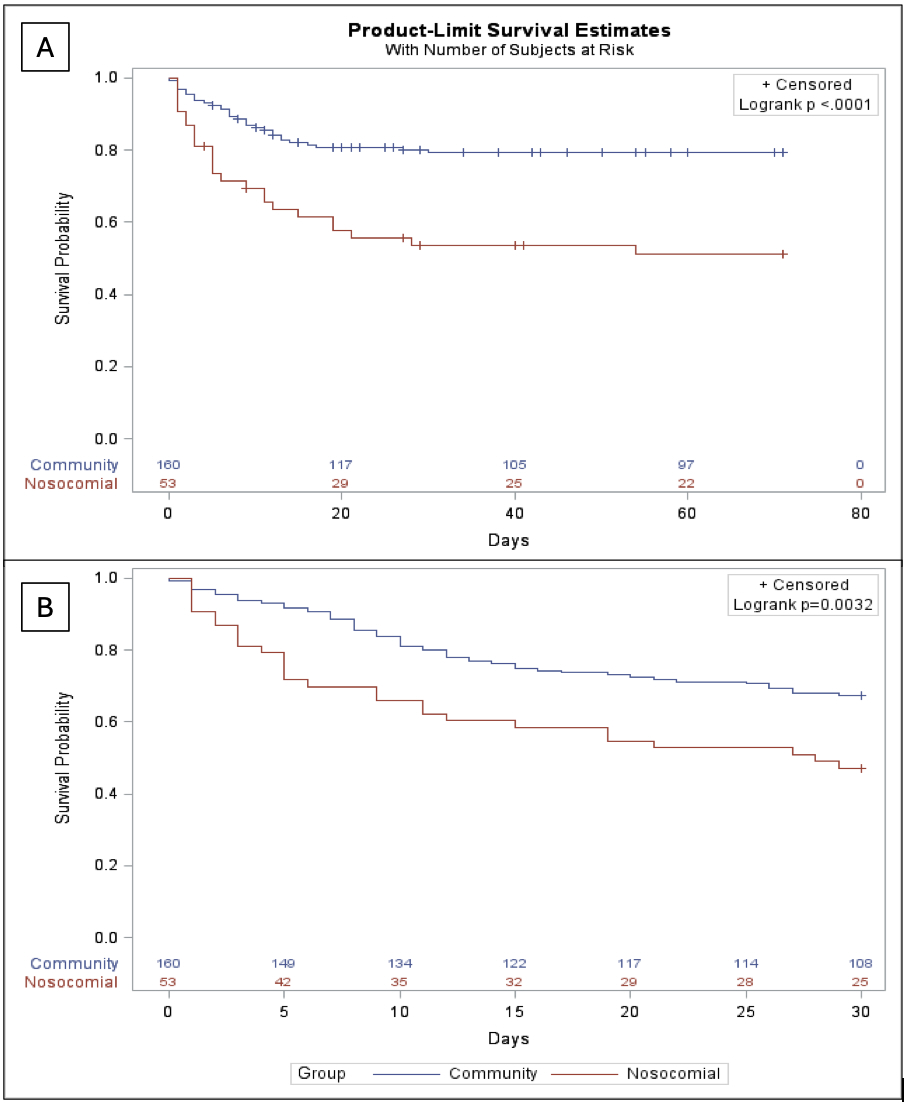
Figure: Kaplan-Meier curves comparing ca-SBP and n-SBP for in-hospital (A) and 30-day (B) mortality.
Disclosures:
Laura Lavette indicated no relevant financial relationships.
Nicolas Intagliata indicated no relevant financial relationships.
Zachary Henry indicated no relevant financial relationships.
Laura Lavette, MD, Nicolas Intagliata, MD, Zachary Henry, MD. P3722 - Nosocomial Spontaneous Bacterial Peritonitis Is Associated With Increased In-Hospital Mortality Compared to Community-Acquired Spontaneous Bacterial Peritonitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Virginia Medical Center, Charlottesville, VA
Introduction: Spontaneous bacterial peritonitis (SBP) is one of the most common causes of infection in decompensated cirrhosis and is associated with high morbidity and mortality. Nosocomial infections have been associated with increased mortality in studies conducted in Europe and Asia; however, data are limited for patients in the United States (US). Through a retrospective analysis of a US cohort, we examined the relative impact of nosocomial SBP (n-SBP) compared to community acquired SBP (ca-SBP) on mortality.
Methods: Adult patients with decompensated cirrhosis and SBP were retrospectively enrolled over an 8-year period at a tertiary care hospital. SBP was defined as ascites fluid with >250 PMN/mm3 without an alternative explanation for peritonitis. Nosocomial infection was defined as SBP occurring greater than 48 hours after hospitalization. Significant predictors on univariable analysis (p >0.05) were combined in a multivariable cox-proportional hazards (CPH) model to assess independent predictors of mortality.
Results: Of 1048 patients with cirrhosis, 213 met criteria for SBP: 160 cases with ca-SBP and 53 with n-SBP. There were no significant differences in age, gender, Model for End-Stage Liver Disease (MELD), hepatocellular carcinoma (HCC), or SBP prophylaxis between groups. The ca-SBP group ascitic fluid studies revealed higher segmented cell count (1370 vs 559, p< 0.001) and culture positivity (32% vs 8%, p< 0.001). Patients in the ca-SBP group had significantly lower length of stay (LOS), in-hospital, and 30-day mortality. However, there was no significant difference in 90-day, 6-month, or 1-year mortality between groups. On multivariable analysis, n-SBP, MELD score, and admission to the intensive care unit (ICU) were independent predictors of in-hospital mortality while only MELD score and admission to ICU were independent predictors at 30 days.
Discussion: Our results suggest that n-SBP increases the risk of in-hospital mortality but thereafter the mortality effects wane. These results are disparate from those of other countries in which n-SBP has been suggested to have a larger impact on mortality. Due to the retrospective nature of this study, it is difficult to isolate the exact impact of antibiotic choices and multidrug resistant organisms on in-hospital mortality. In the future, a prospective, multi-center trial should be considered to further explore the risk of n-SBP in a US population.
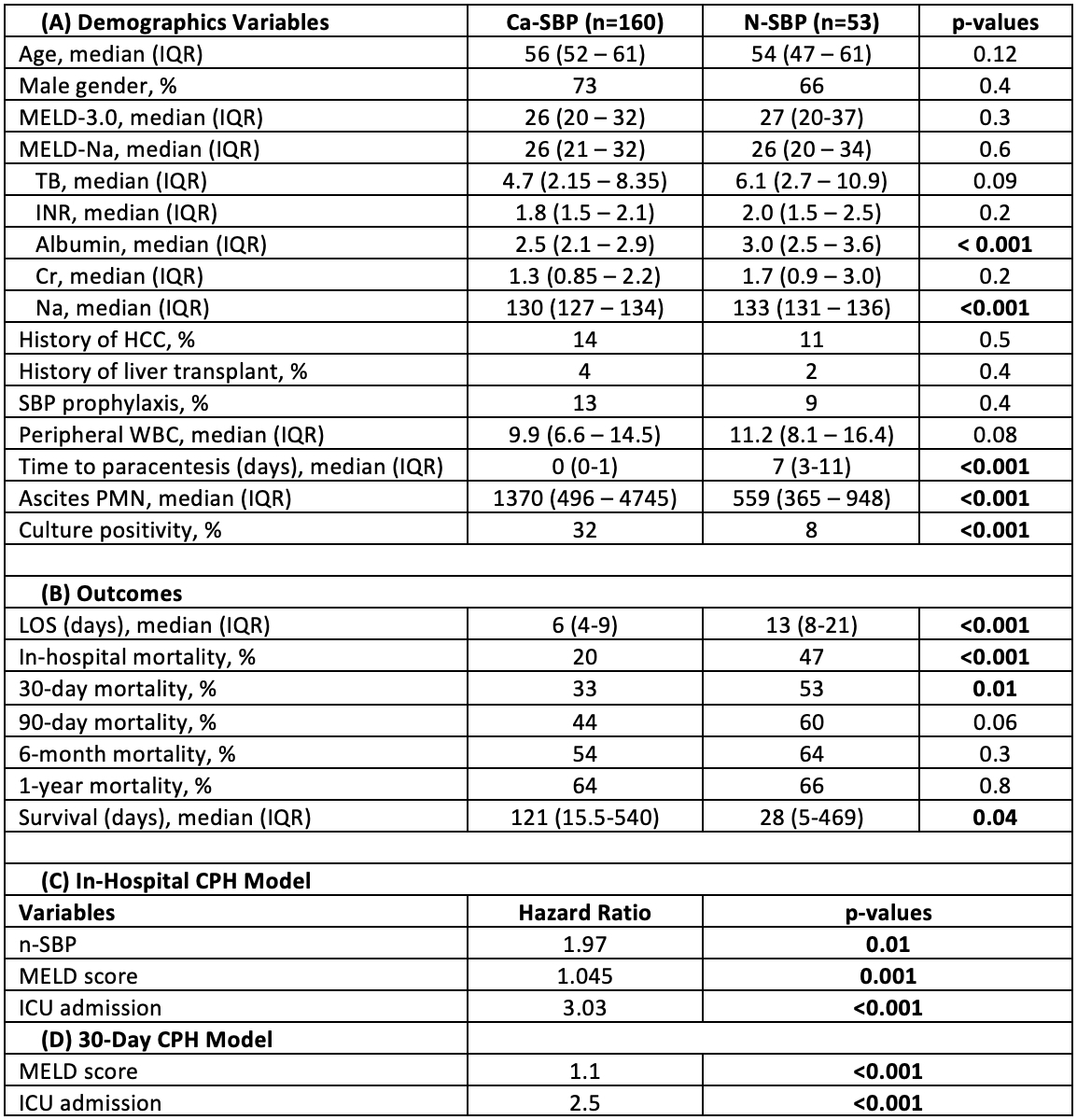
Figure: Demographic (A) and outcome (B) data compared between ca-SBP and n-SBP groups with associated p-values. Cox-Proportional Hazards Models for in-hospital (C) and 30-day (D) mortality with associated hazard ratios and p-values.
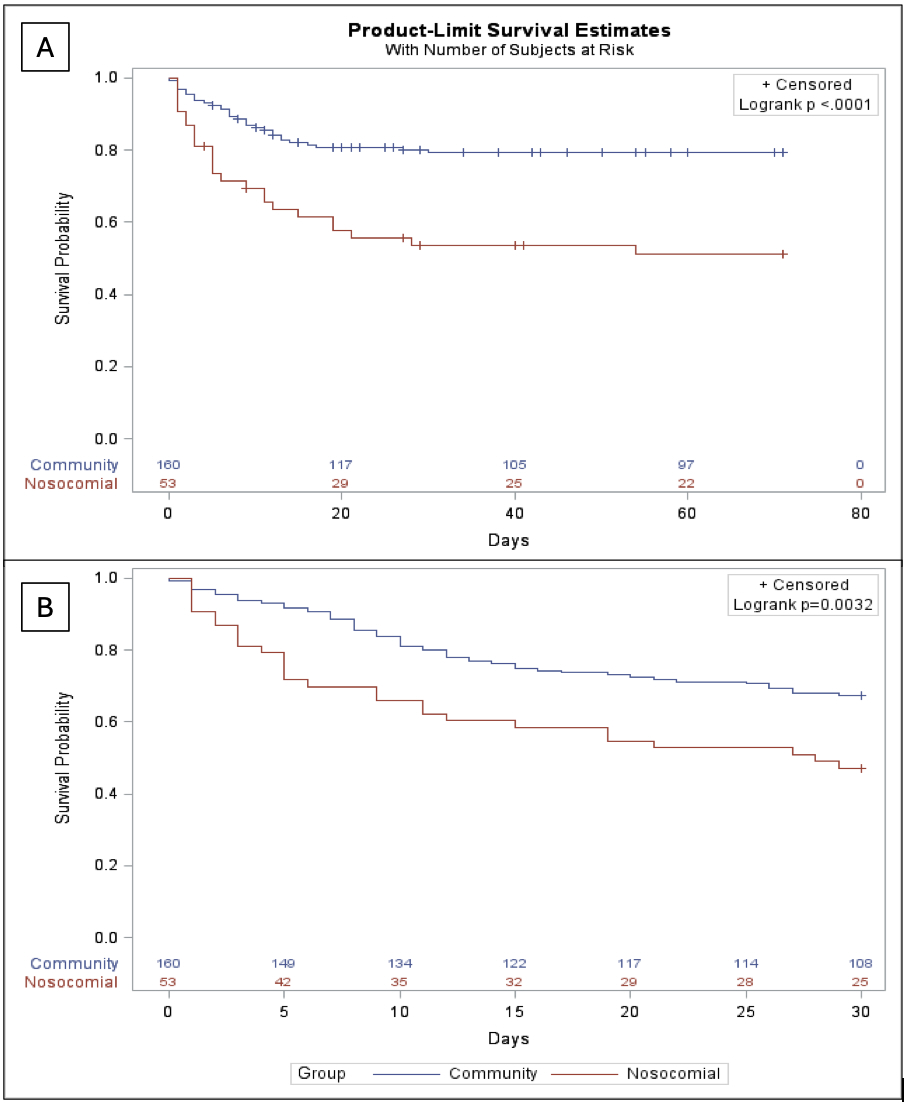
Figure: Kaplan-Meier curves comparing ca-SBP and n-SBP for in-hospital (A) and 30-day (B) mortality.
Disclosures:
Laura Lavette indicated no relevant financial relationships.
Nicolas Intagliata indicated no relevant financial relationships.
Zachary Henry indicated no relevant financial relationships.
Laura Lavette, MD, Nicolas Intagliata, MD, Zachary Henry, MD. P3722 - Nosocomial Spontaneous Bacterial Peritonitis Is Associated With Increased In-Hospital Mortality Compared to Community-Acquired Spontaneous Bacterial Peritonitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
