Monday Poster Session
Category: Liver
P3721 - Rising Trends and Mortality Predictors in MASLD-Associated Cirrhosis: A Nationwide Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Aashutosh Sah, MD (he/him/his)
MacNeal Hospital Loyola Medicine
Brooklyn, NY
Presenting Author(s)
Aashutosh Sah, MD1, Sweta Lohani, MD2, Vaishnavi Modi, MD1, Chaula Desai, MD2, Iyad Al-bustami, MD3, Mahader N. Wossene, MD1
1MacNeal Hospital Loyola Medicine, Berwyn, IL; 2Brooklyn Hospital Center, Brooklyn, NY; 3Brooklyn Hospital Center, Brooklyn, IL
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD) is now the leading cause of chronic liver disease, driven by rising rates of obesity, diabetes, and metabolic syndrome. As MASLD-related cirrhosis becomes more prevalent, hospitalizations and complications such as hepatic encephalopathy and acute-on-chronic liver failure (ACLF) are increasing. Yet, outcome data specific to MASLD-cirrhosis remain limited. This study analyzes national trends, complication rates, and in-hospital mortality predictors in MASLD-associated cirrhosis using a large, representative inpatient dataset.
Methods: A retrospective analysis of the National Inpatient Sample (2018–2022) was conducted. Adult hospitalizations with cirrhosis were identified and stratified by MASLD etiology using ICD-10-CM codes. Outcomes included in-hospital mortality and complications such as acute-on-chronic liver failure (ACLF), hepatic encephalopathy (HE), and hepatocellular carcinoma (HCC). Weighted logistic regression identified independent mortality predictors.
Results: Out of 2.1 million cirrhosis-related hospitalizations, 303,210 (14.4%) involved MASLD. Between 2018 and 2022, ACLF cases in MASLD patients increased by 180% (from 1,565 to 4,385). Despite rising complication rates, in-hospital mortality for MASLD-cirrhosis remained consistently lower than non-MASLD cirrhosis (1.10% vs. 1.40% in 2022).
Multivariate analysis identified adrenal insufficiency (OR 1.75, 95% CI: 1.25–2.45) and congestive heart failure (OR 1.10, 95% CI: 1.00–1.21) as significant predictors of inpatient death. Interestingly, comorbid obesity (OR 0.88), hypertension (OR 0.66), and dyslipidemia (OR 0.62) were independently associated with reduced mortality risk.
Discussion: Despite rising rates of ACLF and other complications, MASLD-cirrhosis patients demonstrated lower inpatient mortality than those with other cirrhosis etiologies. This paradox may reflect earlier detection, differing comorbidity profiles, or improved inpatient management of MASLD-related complications. Notably, adrenal insufficiency emerged as a strong and under-recognized risk factor for mortality, suggesting a gap in current diagnostic and treatment protocols. The identification of CHF as another independent predictor underscores the role of cardiovascular-metabolic interplay in MASLD outcomes. These findings support enhanced inpatient vigilance and multidisciplinary evaluation, including endocrine assessment.
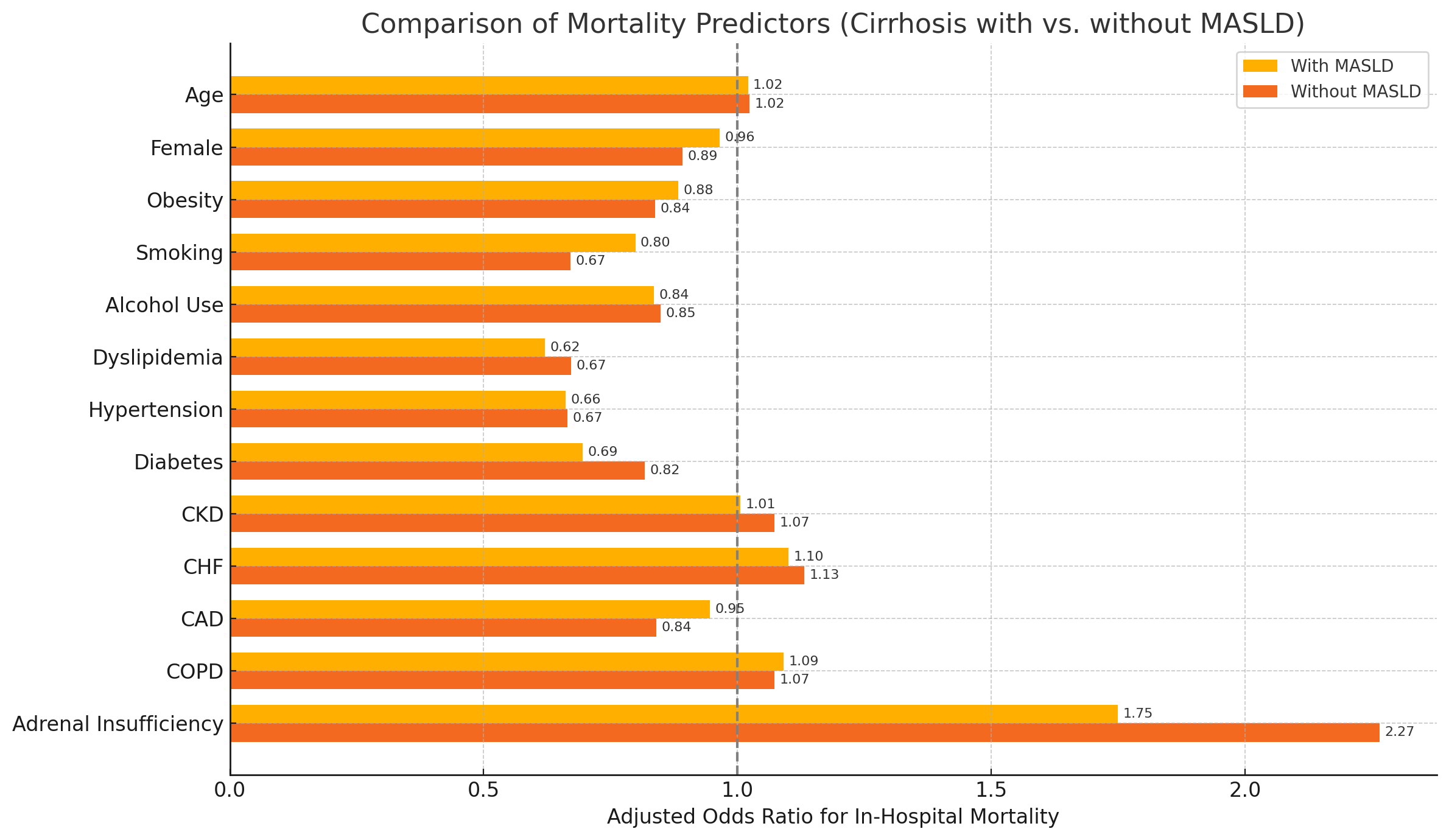
Figure: forrest plot graph
Disclosures:
Aashutosh Sah indicated no relevant financial relationships.
Sweta Lohani indicated no relevant financial relationships.
Vaishnavi Modi indicated no relevant financial relationships.
Chaula Desai indicated no relevant financial relationships.
Iyad Al-bustami indicated no relevant financial relationships.
Mahader Wossene indicated no relevant financial relationships.
Aashutosh Sah, MD1, Sweta Lohani, MD2, Vaishnavi Modi, MD1, Chaula Desai, MD2, Iyad Al-bustami, MD3, Mahader N. Wossene, MD1. P3721 - Rising Trends and Mortality Predictors in MASLD-Associated Cirrhosis: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1MacNeal Hospital Loyola Medicine, Berwyn, IL; 2Brooklyn Hospital Center, Brooklyn, NY; 3Brooklyn Hospital Center, Brooklyn, IL
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD) is now the leading cause of chronic liver disease, driven by rising rates of obesity, diabetes, and metabolic syndrome. As MASLD-related cirrhosis becomes more prevalent, hospitalizations and complications such as hepatic encephalopathy and acute-on-chronic liver failure (ACLF) are increasing. Yet, outcome data specific to MASLD-cirrhosis remain limited. This study analyzes national trends, complication rates, and in-hospital mortality predictors in MASLD-associated cirrhosis using a large, representative inpatient dataset.
Methods: A retrospective analysis of the National Inpatient Sample (2018–2022) was conducted. Adult hospitalizations with cirrhosis were identified and stratified by MASLD etiology using ICD-10-CM codes. Outcomes included in-hospital mortality and complications such as acute-on-chronic liver failure (ACLF), hepatic encephalopathy (HE), and hepatocellular carcinoma (HCC). Weighted logistic regression identified independent mortality predictors.
Results: Out of 2.1 million cirrhosis-related hospitalizations, 303,210 (14.4%) involved MASLD. Between 2018 and 2022, ACLF cases in MASLD patients increased by 180% (from 1,565 to 4,385). Despite rising complication rates, in-hospital mortality for MASLD-cirrhosis remained consistently lower than non-MASLD cirrhosis (1.10% vs. 1.40% in 2022).
Multivariate analysis identified adrenal insufficiency (OR 1.75, 95% CI: 1.25–2.45) and congestive heart failure (OR 1.10, 95% CI: 1.00–1.21) as significant predictors of inpatient death. Interestingly, comorbid obesity (OR 0.88), hypertension (OR 0.66), and dyslipidemia (OR 0.62) were independently associated with reduced mortality risk.
Discussion: Despite rising rates of ACLF and other complications, MASLD-cirrhosis patients demonstrated lower inpatient mortality than those with other cirrhosis etiologies. This paradox may reflect earlier detection, differing comorbidity profiles, or improved inpatient management of MASLD-related complications. Notably, adrenal insufficiency emerged as a strong and under-recognized risk factor for mortality, suggesting a gap in current diagnostic and treatment protocols. The identification of CHF as another independent predictor underscores the role of cardiovascular-metabolic interplay in MASLD outcomes. These findings support enhanced inpatient vigilance and multidisciplinary evaluation, including endocrine assessment.
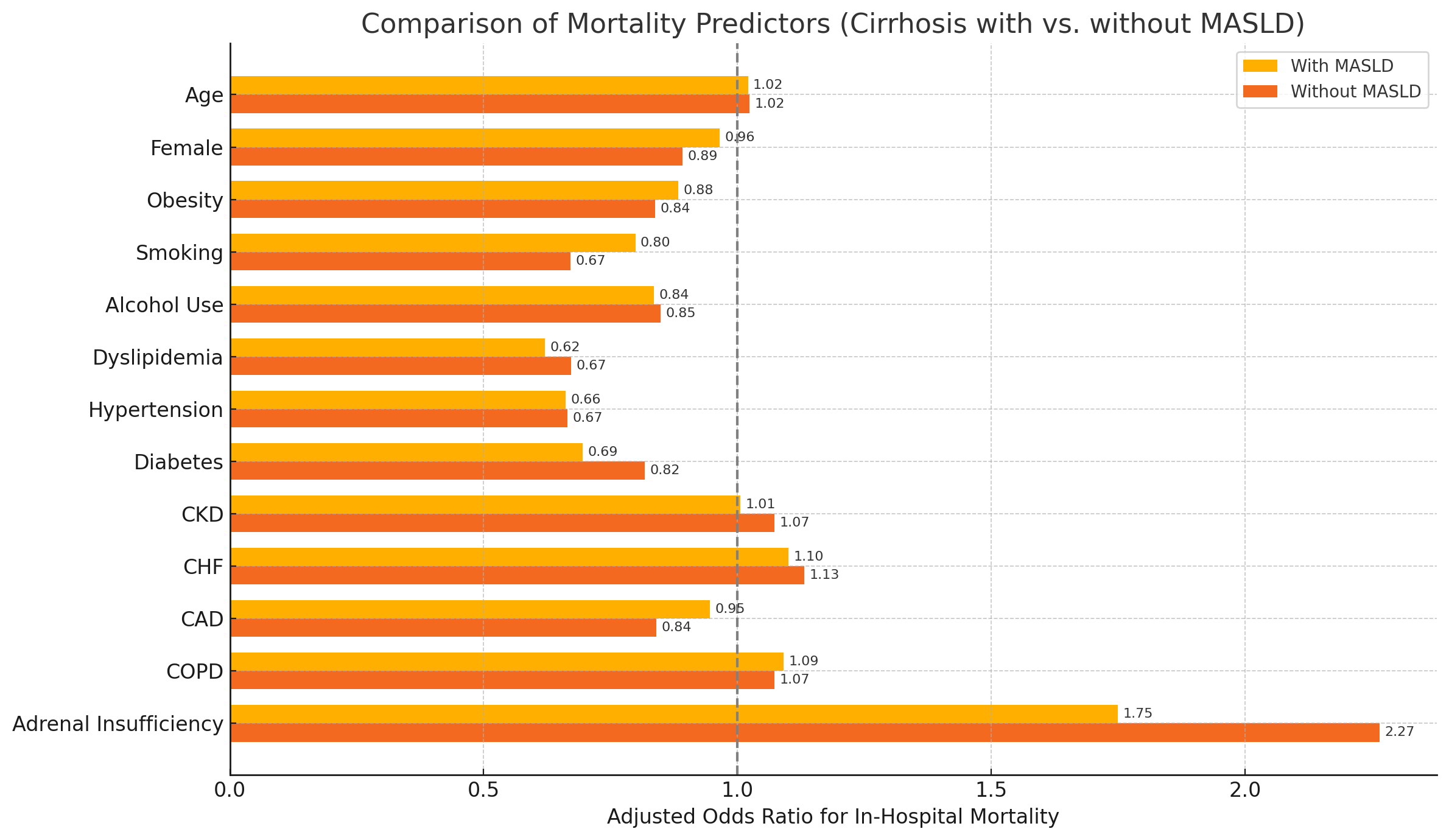
Figure: forrest plot graph
Disclosures:
Aashutosh Sah indicated no relevant financial relationships.
Sweta Lohani indicated no relevant financial relationships.
Vaishnavi Modi indicated no relevant financial relationships.
Chaula Desai indicated no relevant financial relationships.
Iyad Al-bustami indicated no relevant financial relationships.
Mahader Wossene indicated no relevant financial relationships.
Aashutosh Sah, MD1, Sweta Lohani, MD2, Vaishnavi Modi, MD1, Chaula Desai, MD2, Iyad Al-bustami, MD3, Mahader N. Wossene, MD1. P3721 - Rising Trends and Mortality Predictors in MASLD-Associated Cirrhosis: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
