Monday Poster Session
Category: Liver
P3706 - Percutaneous Transluminal Angioplasty vs Stenting for Hepatic Artery Stenosis After Liver Transplantation in Adults
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MS
Mahmoud Shaaban Abdelgalil, MD (he/him/his)
Ain Shams University
Cairo, Al Qahirah, Egypt
Presenting Author(s)
Mahmoud Shaaban Abdelgalil, MD1, Ahmad Abdelrazek, MD2, Sara Metwally, MD3, Sadia Fatima Paracha, MBBS4, Amro Ammar, MD2, Adam Hraybi, 5, Marwa Hassnien, MBBCh6, Abid A. Wazir, 7, Abdelrahman Abdelrazek, MBBCh8, Hammad A. Tanoli, 9, Akram Elegili, MBBCh10, Mahmoud Hassanein, MBBCh11
1Ain Shams University, Cairo, Al Qahirah, Egypt; 2Hartford HealthCare - St. Vincent's Hospital, Bridgeport, CT; 3Corewell Health, Rochester Hills, MI; 4Massachusetts General Hospital, Boston, MA; 5University of Michigan, Dearborn Heights, MI; 6Assiut University, Asyut, Asyut, Egypt; 7University of Michigan, Farmington Hills, MI; 8October 6 University- Faculty of Medicine, 6th of October, Al Qahirah, Egypt; 9Wayne State University, Albuquerque, NM; 10Misr university for science and technology - faculty of medicine, 6th of October, Al Jizah, Egypt; 11Assiut National University, Asyut, Asyut, Egypt
Introduction: Hepatic artery stenosis (HAS) is a serious complication of liver transplantation (LT), with no established guidelines for choosing between percutaneous transluminal Angioplasty (PTA) and stent. This study compared their outcomes to inform clinical practice.
Methods: We searched PubMed, SCOPUS, Cochrane library, and Web of Science for studies comparing PTA and stenting in HAS patients after liver transplantation. The primary outcome was primary patency rate at 6 months, 12 months, and the end of follow-up. Secondary outcomes included technical success, major complications, Hepatic artery thrombosis (HAT) incidence, reintervention rates, and time to recurrent HAS. We also conducted a subgroup analysis based on major complication types, specifically artery dissection and rupture. Study quality was assessed using the Newcastle–Ottawa scale, and data analysis was performed using REVMAN 5.4.1.
Results: Nine observational studies, including 325 patients with HAS after LT, were analyzed, with 140 treated with PTA alone and 197 with stents. No significant differences were found between stenting and PTA in primary patency rates at 6 months, 12 months, and the end of follow-up, as well as in technical success, major complications, artery dissection, artery rupture, and HAT incidence. However, stenting was significantly associated with a lower reintervention rate (RR = 0.57, 95% CI [0.36, 0.89], P = 0.01) and a longer time to recurrent HAS compared to PTA (MD = 36.42, 95% CI [14.14, 58.70], P = 0.001).
Discussion: Both PTA and stenting demonstrate comparable primary patency rates and safety outcomes, making them viable options for HAS treatment after liver transplantation. However, stenting was associated with a lower reintervention rate and a longer time to recurrent HAS, suggesting potential long-term benefits. Treatment selection should be individualized, considering anatomical factors, stenosis morphology, and operator expertise.
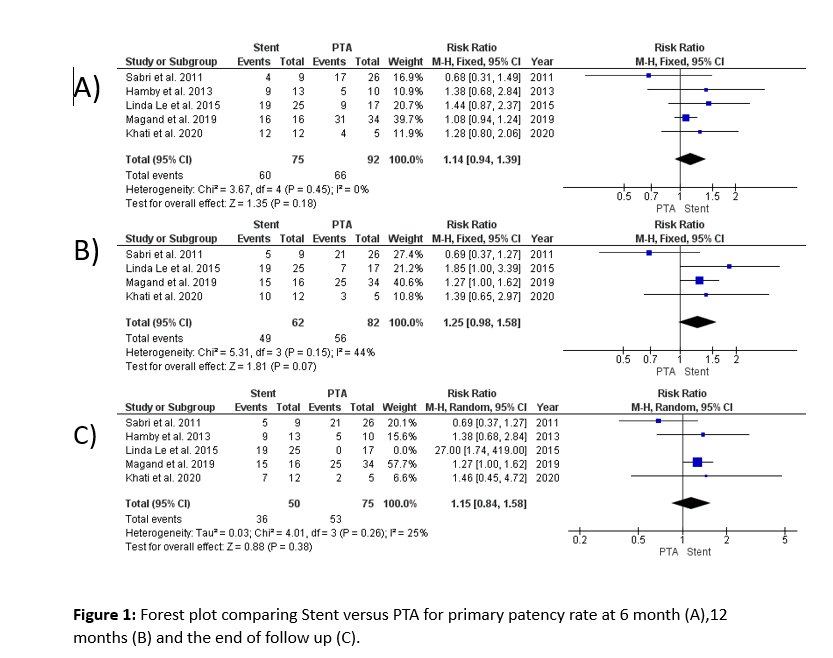
Figure: (A)
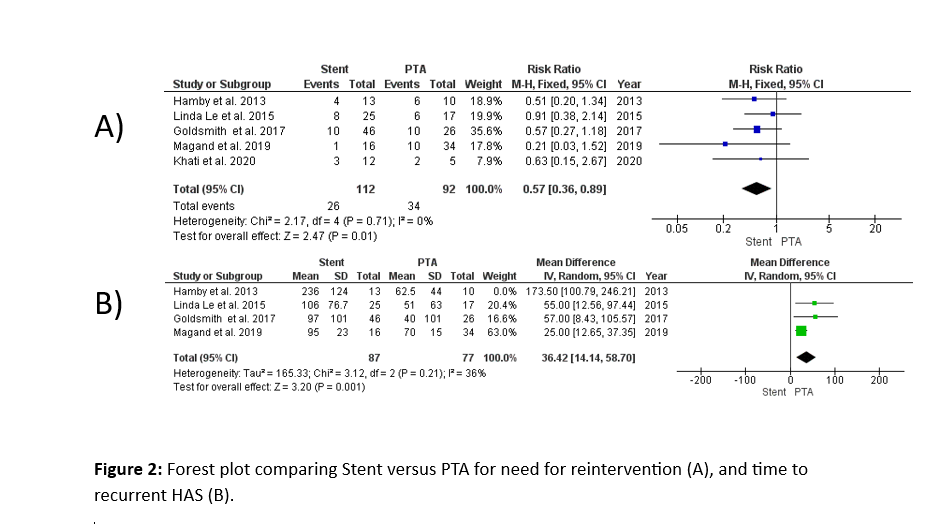
Figure: (B)
Disclosures:
Mahmoud Shaaban Abdelgalil indicated no relevant financial relationships.
Ahmad Abdelrazek indicated no relevant financial relationships.
Sara Metwally indicated no relevant financial relationships.
Sadia Fatima Paracha indicated no relevant financial relationships.
Amro Ammar indicated no relevant financial relationships.
Adam Hraybi indicated no relevant financial relationships.
Marwa Hassnien indicated no relevant financial relationships.
Abid Wazir indicated no relevant financial relationships.
Abdelrahman Abdelrazek indicated no relevant financial relationships.
Hammad Tanoli indicated no relevant financial relationships.
Akram Elegili indicated no relevant financial relationships.
Mahmoud Hassanein indicated no relevant financial relationships.
Mahmoud Shaaban Abdelgalil, MD1, Ahmad Abdelrazek, MD2, Sara Metwally, MD3, Sadia Fatima Paracha, MBBS4, Amro Ammar, MD2, Adam Hraybi, 5, Marwa Hassnien, MBBCh6, Abid A. Wazir, 7, Abdelrahman Abdelrazek, MBBCh8, Hammad A. Tanoli, 9, Akram Elegili, MBBCh10, Mahmoud Hassanein, MBBCh11. P3706 - Percutaneous Transluminal Angioplasty vs Stenting for Hepatic Artery Stenosis After Liver Transplantation in Adults, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Ain Shams University, Cairo, Al Qahirah, Egypt; 2Hartford HealthCare - St. Vincent's Hospital, Bridgeport, CT; 3Corewell Health, Rochester Hills, MI; 4Massachusetts General Hospital, Boston, MA; 5University of Michigan, Dearborn Heights, MI; 6Assiut University, Asyut, Asyut, Egypt; 7University of Michigan, Farmington Hills, MI; 8October 6 University- Faculty of Medicine, 6th of October, Al Qahirah, Egypt; 9Wayne State University, Albuquerque, NM; 10Misr university for science and technology - faculty of medicine, 6th of October, Al Jizah, Egypt; 11Assiut National University, Asyut, Asyut, Egypt
Introduction: Hepatic artery stenosis (HAS) is a serious complication of liver transplantation (LT), with no established guidelines for choosing between percutaneous transluminal Angioplasty (PTA) and stent. This study compared their outcomes to inform clinical practice.
Methods: We searched PubMed, SCOPUS, Cochrane library, and Web of Science for studies comparing PTA and stenting in HAS patients after liver transplantation. The primary outcome was primary patency rate at 6 months, 12 months, and the end of follow-up. Secondary outcomes included technical success, major complications, Hepatic artery thrombosis (HAT) incidence, reintervention rates, and time to recurrent HAS. We also conducted a subgroup analysis based on major complication types, specifically artery dissection and rupture. Study quality was assessed using the Newcastle–Ottawa scale, and data analysis was performed using REVMAN 5.4.1.
Results: Nine observational studies, including 325 patients with HAS after LT, were analyzed, with 140 treated with PTA alone and 197 with stents. No significant differences were found between stenting and PTA in primary patency rates at 6 months, 12 months, and the end of follow-up, as well as in technical success, major complications, artery dissection, artery rupture, and HAT incidence. However, stenting was significantly associated with a lower reintervention rate (RR = 0.57, 95% CI [0.36, 0.89], P = 0.01) and a longer time to recurrent HAS compared to PTA (MD = 36.42, 95% CI [14.14, 58.70], P = 0.001).
Discussion: Both PTA and stenting demonstrate comparable primary patency rates and safety outcomes, making them viable options for HAS treatment after liver transplantation. However, stenting was associated with a lower reintervention rate and a longer time to recurrent HAS, suggesting potential long-term benefits. Treatment selection should be individualized, considering anatomical factors, stenosis morphology, and operator expertise.
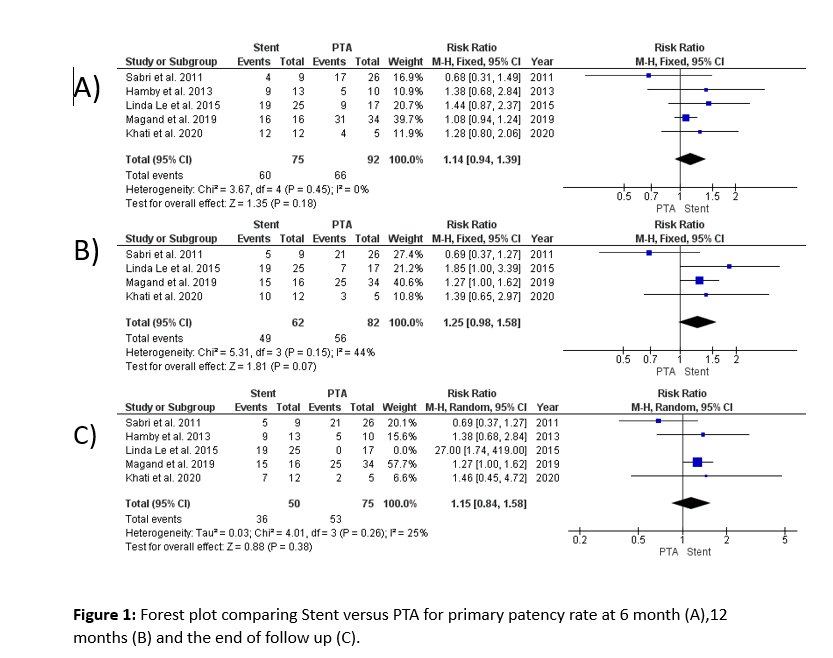
Figure: (A)
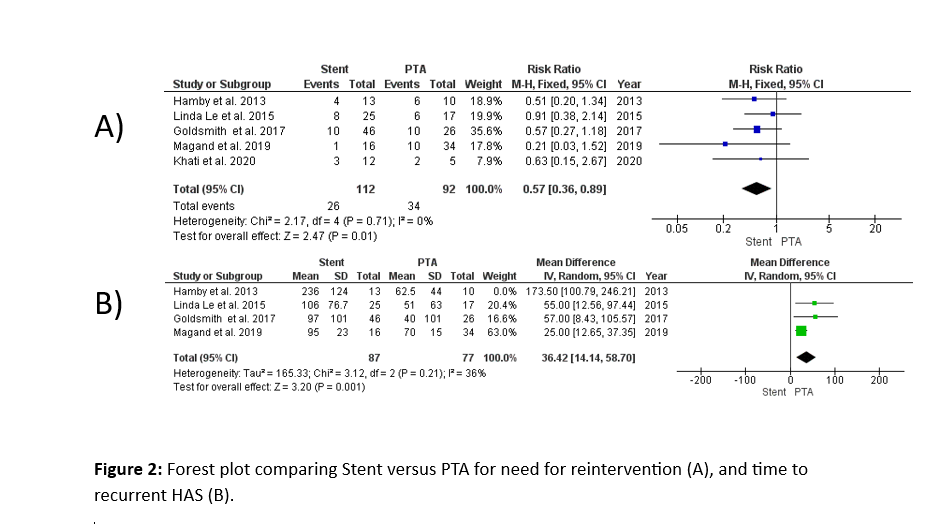
Figure: (B)
Disclosures:
Mahmoud Shaaban Abdelgalil indicated no relevant financial relationships.
Ahmad Abdelrazek indicated no relevant financial relationships.
Sara Metwally indicated no relevant financial relationships.
Sadia Fatima Paracha indicated no relevant financial relationships.
Amro Ammar indicated no relevant financial relationships.
Adam Hraybi indicated no relevant financial relationships.
Marwa Hassnien indicated no relevant financial relationships.
Abid Wazir indicated no relevant financial relationships.
Abdelrahman Abdelrazek indicated no relevant financial relationships.
Hammad Tanoli indicated no relevant financial relationships.
Akram Elegili indicated no relevant financial relationships.
Mahmoud Hassanein indicated no relevant financial relationships.
Mahmoud Shaaban Abdelgalil, MD1, Ahmad Abdelrazek, MD2, Sara Metwally, MD3, Sadia Fatima Paracha, MBBS4, Amro Ammar, MD2, Adam Hraybi, 5, Marwa Hassnien, MBBCh6, Abid A. Wazir, 7, Abdelrahman Abdelrazek, MBBCh8, Hammad A. Tanoli, 9, Akram Elegili, MBBCh10, Mahmoud Hassanein, MBBCh11. P3706 - Percutaneous Transluminal Angioplasty vs Stenting for Hepatic Artery Stenosis After Liver Transplantation in Adults, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
