Monday Poster Session
Category: Liver
P3790 - Epidemiology and Outcomes of Hepatic Veno-Occlusive Disease in Allogenic Stem Cell Transplant Recipients in the United States
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Aditya Sharma, MD (he/him/his)
Wayne State University School of Medicine / Detroit Medical Center
Detroit, MI
Presenting Author(s)
Aditya Sharma, MD1, Sarvani Surapaneni, MD2, Aditi Sharma, MD3, Ayman Soubani, MD1
1Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 2Trinity Health Ann Arbor Hospital, Ann Arbor, MI; 3Karmanos Cancer Institute, Detroit, MI
Introduction: Hepatic veno-occlusive disease (HVOD), or sinusoidal obstruction syndrome (SOS), is a potentially liefe-threatening complication following allogeneic stem cell transplantation (allo-SCT). Historically, HVOD affected up to 60% of allo-SCT recipients, with mortality rates over 75% in severe cases. The approval of defibrotide in 2016 represented a major therapeutic milestone, significantly improving outcomes in high-risk patients. Despite this, large-scale data on HVOD epidemiology & outcomes in allo-SCT recipients remain limited.
Methods: We utilized National Inpatient Sample (2016-2020) to examine factors associated with HVOD in allo-SCT recipients. Admissions for allo-SCT & HVOD were identified using ICD 10 codes. Baseline characteristics, including patient demographics, hospital characteristics, comorbidities, complications & outcomes were compared between allo-SCT admissions with & without HVOD. Categorical variables were analyzed by χ² test (%), & continuous variables by adjusted Wald’s test (mean±SD).
Results: During the study period, 200 allo-SCT admissions with HVOD were identified. HVOD admissions were younger (45.05 vs. 52.42 years; P=0.0045) & were more likely to be female (43.72% vs. 25%; P=0.0191). They had higher rates of acute graft-versus-host disease (GVHD) (17.5% vs. 6.47%; P=0.0043), acute respiratory failure (32.5% vs. 8.37%; P< 0.001), & acute kidney injury (50% vs. 20.66%; P< 0.001). Hepatic complications, including portal hypertension (7.5% vs. 0.52%; P< 0.001), hepatic encephalopathy (12.5% vs. 0.28%; P< 0.001), cirrhosis (7.5% vs. 0.07%; P< 0.001), ascites (37.5% vs. 1.97%; P< 0.001) & spontaneous bacterial peritonitis (2.5% vs. 0.06%; P< 0.001) were also more common in this cohort. HVOD was associated with worse outcomes, including longer hospital stays (45.5 vs. 29.51 days; P< 0.001) & over 6 times higher in-hospital mortality (30% vs. 4.72%; P< 0.001). HVOD also imposed a greater economic burden, with more than double mean total hospitalization charges ($1,321,650 vs. $541,391.1; P< 0.001) & nearly triple hospitalization costs ($358,463.2 vs. $141,464.1; P< 0.001).
Discussion: This large-scale study shows HVOD in allo-SCT drives severe hepatic complications and multi-organ dysfunction, leading to excessively high ( >6x) in-hospital mortality, prolonged hospital stays, and substantially increased (2-3x) healthcare costs. These stark outcomes underscore an urgent need for improved risk stratification models and novel, liver-focused therapeutic strategies
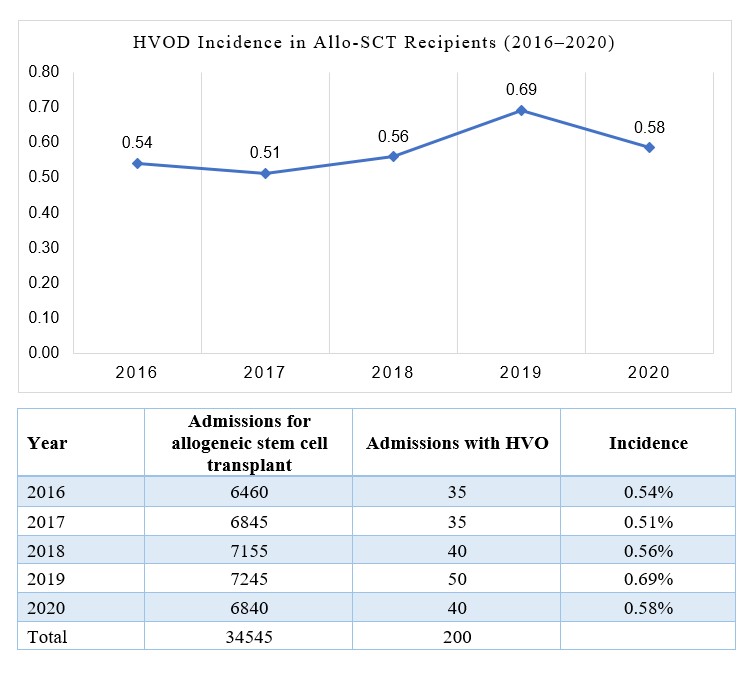
Figure: Table: Baseline Characteristics of Allogeneic Stem Cell Transplant Recipients With & Without Hepatic Veno-Occlusive Disease in the U.S. (2016–2020)
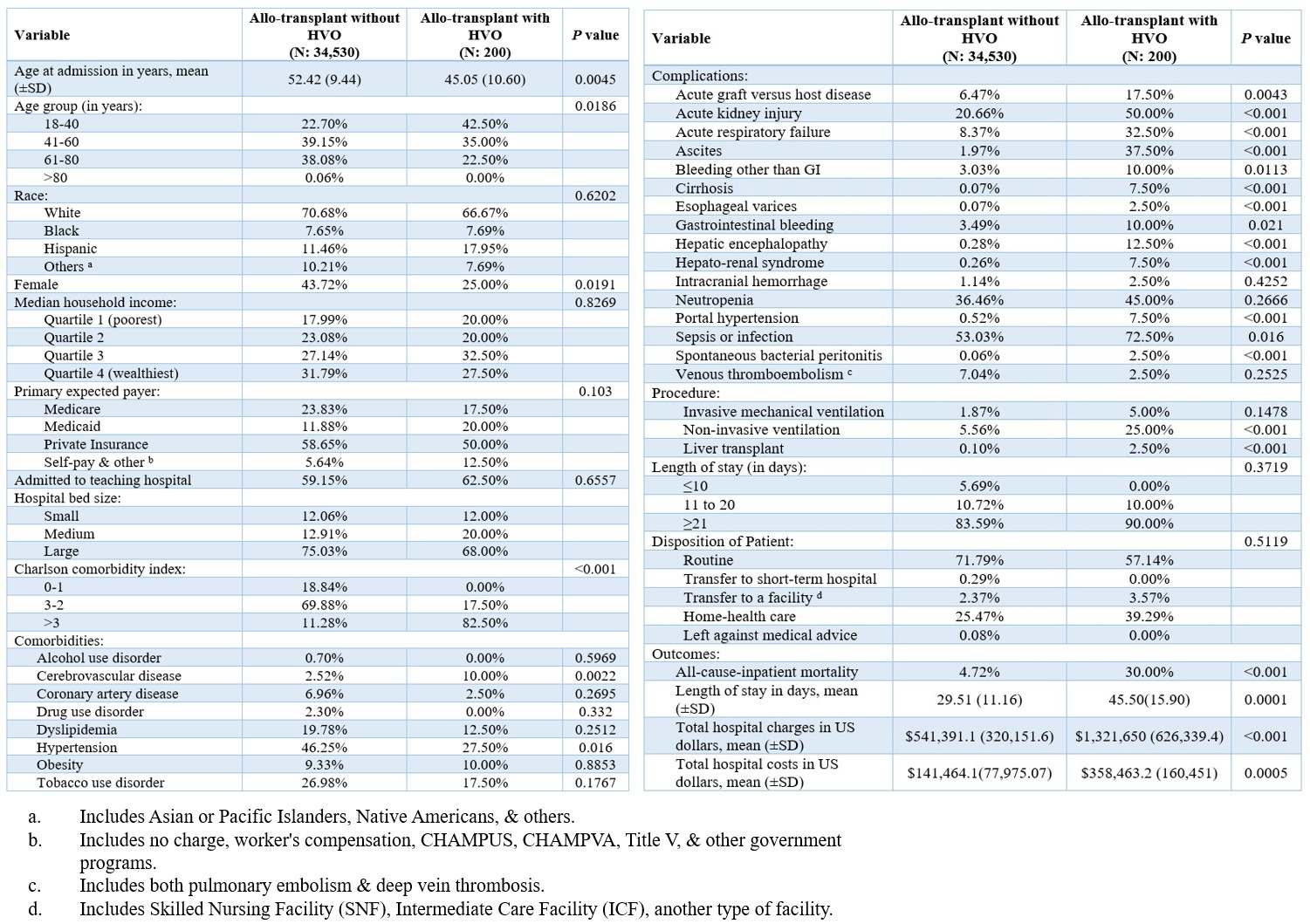
Figure: Figure: Incidence of Hepatic Veno-Occlusive Disease in Allogeneic Stem Cell Transplant Recipients, 2016–2020
Disclosures:
Aditya Sharma indicated no relevant financial relationships.
Sarvani Surapaneni indicated no relevant financial relationships.
Aditi Sharma indicated no relevant financial relationships.
Ayman Soubani indicated no relevant financial relationships.
Aditya Sharma, MD1, Sarvani Surapaneni, MD2, Aditi Sharma, MD3, Ayman Soubani, MD1. P3790 - Epidemiology and Outcomes of Hepatic Veno-Occlusive Disease in Allogenic Stem Cell Transplant Recipients in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 2Trinity Health Ann Arbor Hospital, Ann Arbor, MI; 3Karmanos Cancer Institute, Detroit, MI
Introduction: Hepatic veno-occlusive disease (HVOD), or sinusoidal obstruction syndrome (SOS), is a potentially liefe-threatening complication following allogeneic stem cell transplantation (allo-SCT). Historically, HVOD affected up to 60% of allo-SCT recipients, with mortality rates over 75% in severe cases. The approval of defibrotide in 2016 represented a major therapeutic milestone, significantly improving outcomes in high-risk patients. Despite this, large-scale data on HVOD epidemiology & outcomes in allo-SCT recipients remain limited.
Methods: We utilized National Inpatient Sample (2016-2020) to examine factors associated with HVOD in allo-SCT recipients. Admissions for allo-SCT & HVOD were identified using ICD 10 codes. Baseline characteristics, including patient demographics, hospital characteristics, comorbidities, complications & outcomes were compared between allo-SCT admissions with & without HVOD. Categorical variables were analyzed by χ² test (%), & continuous variables by adjusted Wald’s test (mean±SD).
Results: During the study period, 200 allo-SCT admissions with HVOD were identified. HVOD admissions were younger (45.05 vs. 52.42 years; P=0.0045) & were more likely to be female (43.72% vs. 25%; P=0.0191). They had higher rates of acute graft-versus-host disease (GVHD) (17.5% vs. 6.47%; P=0.0043), acute respiratory failure (32.5% vs. 8.37%; P< 0.001), & acute kidney injury (50% vs. 20.66%; P< 0.001). Hepatic complications, including portal hypertension (7.5% vs. 0.52%; P< 0.001), hepatic encephalopathy (12.5% vs. 0.28%; P< 0.001), cirrhosis (7.5% vs. 0.07%; P< 0.001), ascites (37.5% vs. 1.97%; P< 0.001) & spontaneous bacterial peritonitis (2.5% vs. 0.06%; P< 0.001) were also more common in this cohort. HVOD was associated with worse outcomes, including longer hospital stays (45.5 vs. 29.51 days; P< 0.001) & over 6 times higher in-hospital mortality (30% vs. 4.72%; P< 0.001). HVOD also imposed a greater economic burden, with more than double mean total hospitalization charges ($1,321,650 vs. $541,391.1; P< 0.001) & nearly triple hospitalization costs ($358,463.2 vs. $141,464.1; P< 0.001).
Discussion: This large-scale study shows HVOD in allo-SCT drives severe hepatic complications and multi-organ dysfunction, leading to excessively high ( >6x) in-hospital mortality, prolonged hospital stays, and substantially increased (2-3x) healthcare costs. These stark outcomes underscore an urgent need for improved risk stratification models and novel, liver-focused therapeutic strategies
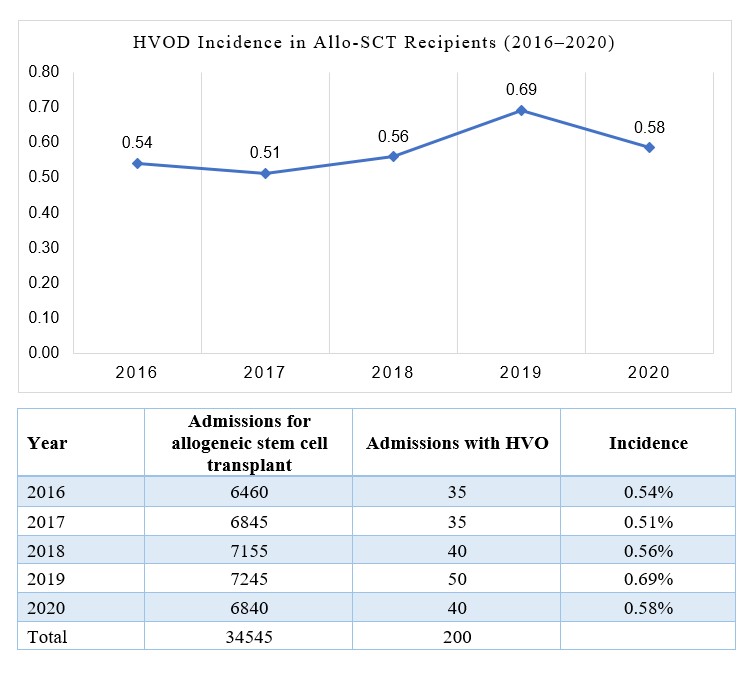
Figure: Table: Baseline Characteristics of Allogeneic Stem Cell Transplant Recipients With & Without Hepatic Veno-Occlusive Disease in the U.S. (2016–2020)
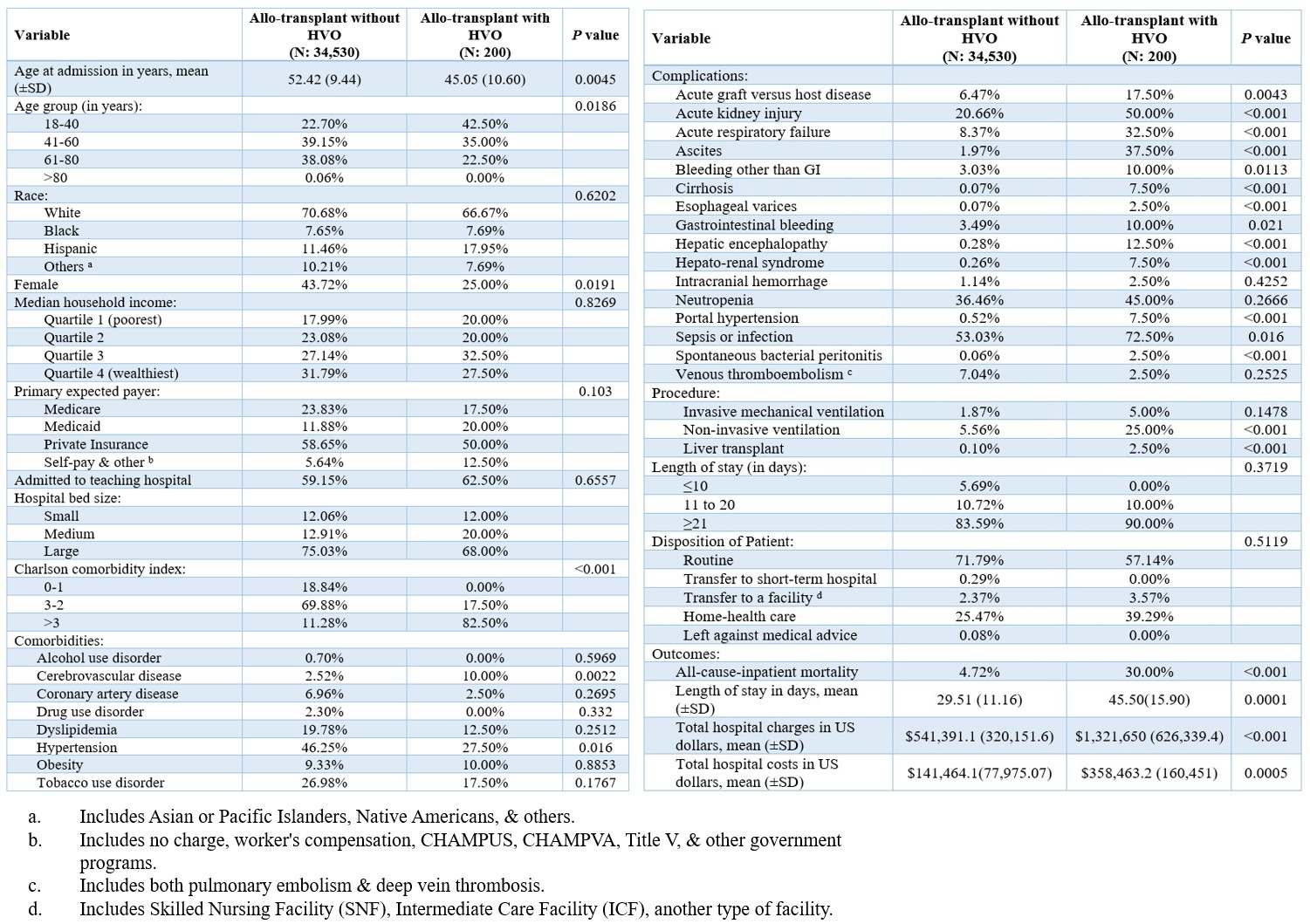
Figure: Figure: Incidence of Hepatic Veno-Occlusive Disease in Allogeneic Stem Cell Transplant Recipients, 2016–2020
Disclosures:
Aditya Sharma indicated no relevant financial relationships.
Sarvani Surapaneni indicated no relevant financial relationships.
Aditi Sharma indicated no relevant financial relationships.
Ayman Soubani indicated no relevant financial relationships.
Aditya Sharma, MD1, Sarvani Surapaneni, MD2, Aditi Sharma, MD3, Ayman Soubani, MD1. P3790 - Epidemiology and Outcomes of Hepatic Veno-Occlusive Disease in Allogenic Stem Cell Transplant Recipients in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
