Monday Poster Session
Category: Liver
P3787 - Outcomes of Septic Shock in Liver Transplant Recipients: A Nationwide Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hameed Ullah, MD
St. Luke's Hospital
Chesterfield, MO
Presenting Author(s)
Hameed Ullah, MD1, Shahryar Khan, MD2, Mustafa Shah, MD3, Muhammad Arsalan, MD1, Wagmah Javed. Khan, MD1, Osama Sherjeel Khan, MD4, Ijaz Ali, MD5, Kamran Qureshi, MD6
1St. Luke's Hospital, Chesterfield, MO; 2University of Kansas Medical Center, Kansas City, KS; 3Geisinger Health System, Danville, PA; 4Cleveland Clinic Florida, Weston, FL; 5Trinity Health Oakland / Wayne State University School of Medicine, Pontiac, MI; 6Saint Louis University School of Medicine, Saint Louis, MO
Introduction: While some observational studies have suggested potentially favorable outcomes for solid organ transplant recipients with sepsis, this study specifically investigates the impact of liver transplant recipient status on outcomes in patients diagnosed with septic shock.
Methods: We conducted a retrospective cohort study using the 2020-2022 NIS database. The study population comprised adult patients (≥18 years) with a principal diagnosis of septic shock. The exposure group included those with a history of liver transplant (n=3,575), and the control group consisted of patients with septic shock without a liver transplant history (n=1,623,049). We examined multiple baseline characteristics including sex, race, age, and Charlson comorbidity index. Multivariate regression analyses, adjusted for relevant covariates, were performed to compare in-hospital mortality, LOS, total hospital charges, acute kidney injury (AKI), cardiac arrest, acute hypoxic respiratory failure (AHRF), and the need for intubation between the two groups.
Results: Baseline characteristics are listed in table 1. The crude in-hospital mortality rate was significantly lower in liver transplant recipients (28.4%) compared to the general septic shock population (33.7%, p=0.002). After adjusting for confounders, liver transplant recipients with septic shock exhibited a significantly lower odds of in-hospital mortality (aOR = 0.79, p=0.005), cardiac arrest (aOR = 0.62, p=0.003), and AHRF (aOR = 0.73, p< 0.001) compared to the general population with septic shock. There was no significant difference in LOS (Adjusted Coefficient = 0.34 days, p=0.58) and total hospital charges (Adjusted Coefficient = 22457 USD, p=0.1) between the two groups. While the odds of developing AKI and the need for intubation were numerically different between the two groups, these differences did not reach statistical significance.
Discussion: In this large national analysis focused specifically on patients with septic shock, liver transplant recipients presented with distinct baseline characteristics and a lower crude mortality rate. After adjustment, they demonstrated a lower risk of in-hospital
mortality, cardiac arrest, and acute hypoxic respiratory failure. There was no significant difference in LOS, total hospital charges, AKI, and the need for intubation between the two groups. These findings validate previous smaller observational studies and highlight the complex interplay of factors influencing outcomes in liver transplant recipients.
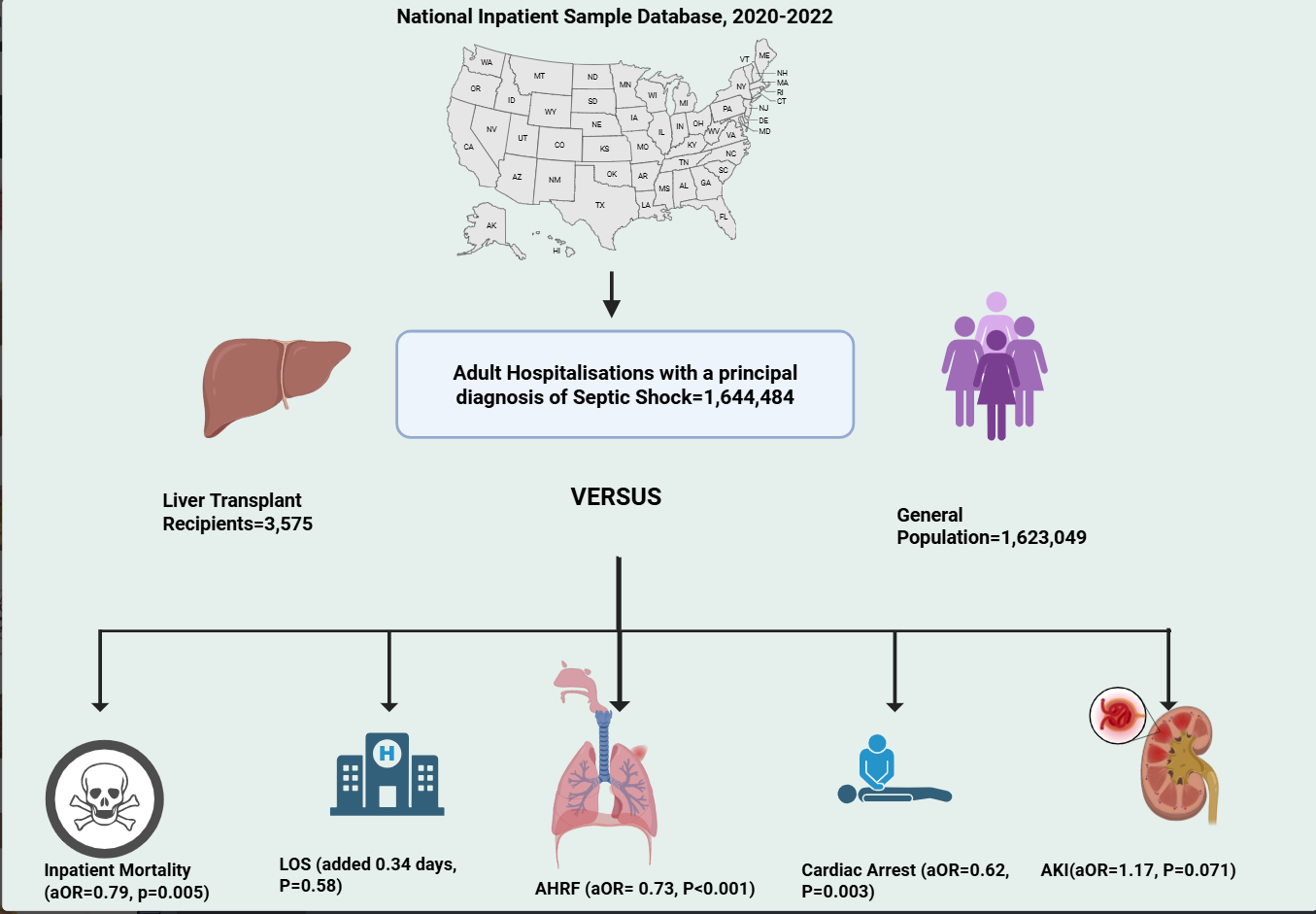
Figure: Table. 1: Baseline Characteristics
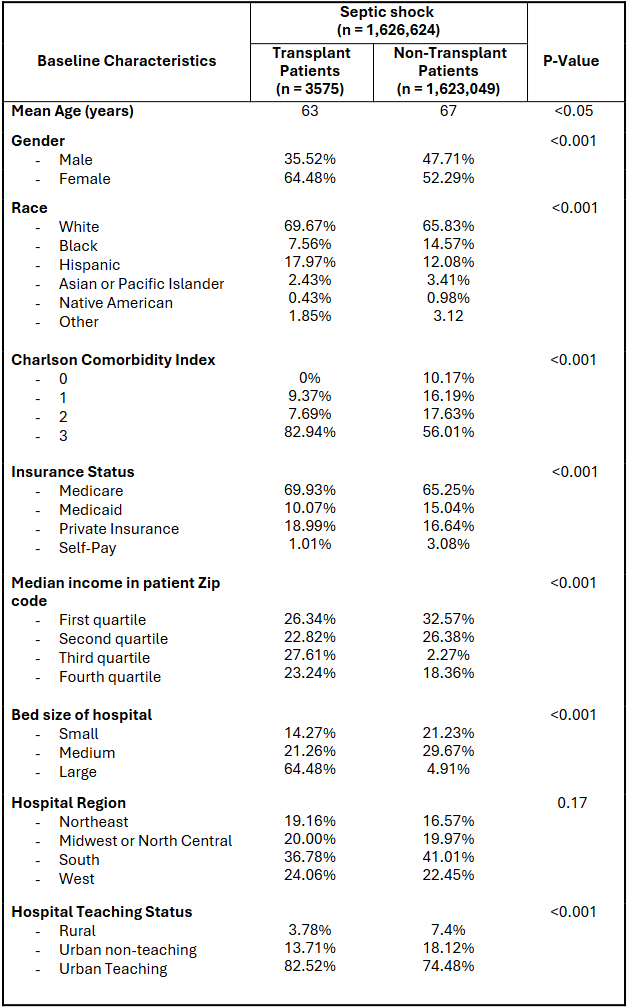
Figure: Inpatient Outcomes Adjusted for Covariates
Disclosures:
Hameed Ullah indicated no relevant financial relationships.
Shahryar Khan indicated no relevant financial relationships.
Mustafa Shah indicated no relevant financial relationships.
Muhammad Arsalan indicated no relevant financial relationships.
Wagmah Khan indicated no relevant financial relationships.
Osama Sherjeel Khan indicated no relevant financial relationships.
Ijaz Ali indicated no relevant financial relationships.
Kamran Qureshi: Gilead Sciences – Speakers Bureau. Intercept Pharmaceuticals – Speakers Bureau. Madrigal Pharmaceuticals – Speakers Bureau. Phathom Pharmaceuticals – Speakers Bureau. Salix Pharmaceuticals – Speakers Bureau.
Hameed Ullah, MD1, Shahryar Khan, MD2, Mustafa Shah, MD3, Muhammad Arsalan, MD1, Wagmah Javed. Khan, MD1, Osama Sherjeel Khan, MD4, Ijaz Ali, MD5, Kamran Qureshi, MD6. P3787 - Outcomes of Septic Shock in Liver Transplant Recipients: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Luke's Hospital, Chesterfield, MO; 2University of Kansas Medical Center, Kansas City, KS; 3Geisinger Health System, Danville, PA; 4Cleveland Clinic Florida, Weston, FL; 5Trinity Health Oakland / Wayne State University School of Medicine, Pontiac, MI; 6Saint Louis University School of Medicine, Saint Louis, MO
Introduction: While some observational studies have suggested potentially favorable outcomes for solid organ transplant recipients with sepsis, this study specifically investigates the impact of liver transplant recipient status on outcomes in patients diagnosed with septic shock.
Methods: We conducted a retrospective cohort study using the 2020-2022 NIS database. The study population comprised adult patients (≥18 years) with a principal diagnosis of septic shock. The exposure group included those with a history of liver transplant (n=3,575), and the control group consisted of patients with septic shock without a liver transplant history (n=1,623,049). We examined multiple baseline characteristics including sex, race, age, and Charlson comorbidity index. Multivariate regression analyses, adjusted for relevant covariates, were performed to compare in-hospital mortality, LOS, total hospital charges, acute kidney injury (AKI), cardiac arrest, acute hypoxic respiratory failure (AHRF), and the need for intubation between the two groups.
Results: Baseline characteristics are listed in table 1. The crude in-hospital mortality rate was significantly lower in liver transplant recipients (28.4%) compared to the general septic shock population (33.7%, p=0.002). After adjusting for confounders, liver transplant recipients with septic shock exhibited a significantly lower odds of in-hospital mortality (aOR = 0.79, p=0.005), cardiac arrest (aOR = 0.62, p=0.003), and AHRF (aOR = 0.73, p< 0.001) compared to the general population with septic shock. There was no significant difference in LOS (Adjusted Coefficient = 0.34 days, p=0.58) and total hospital charges (Adjusted Coefficient = 22457 USD, p=0.1) between the two groups. While the odds of developing AKI and the need for intubation were numerically different between the two groups, these differences did not reach statistical significance.
Discussion: In this large national analysis focused specifically on patients with septic shock, liver transplant recipients presented with distinct baseline characteristics and a lower crude mortality rate. After adjustment, they demonstrated a lower risk of in-hospital
mortality, cardiac arrest, and acute hypoxic respiratory failure. There was no significant difference in LOS, total hospital charges, AKI, and the need for intubation between the two groups. These findings validate previous smaller observational studies and highlight the complex interplay of factors influencing outcomes in liver transplant recipients.
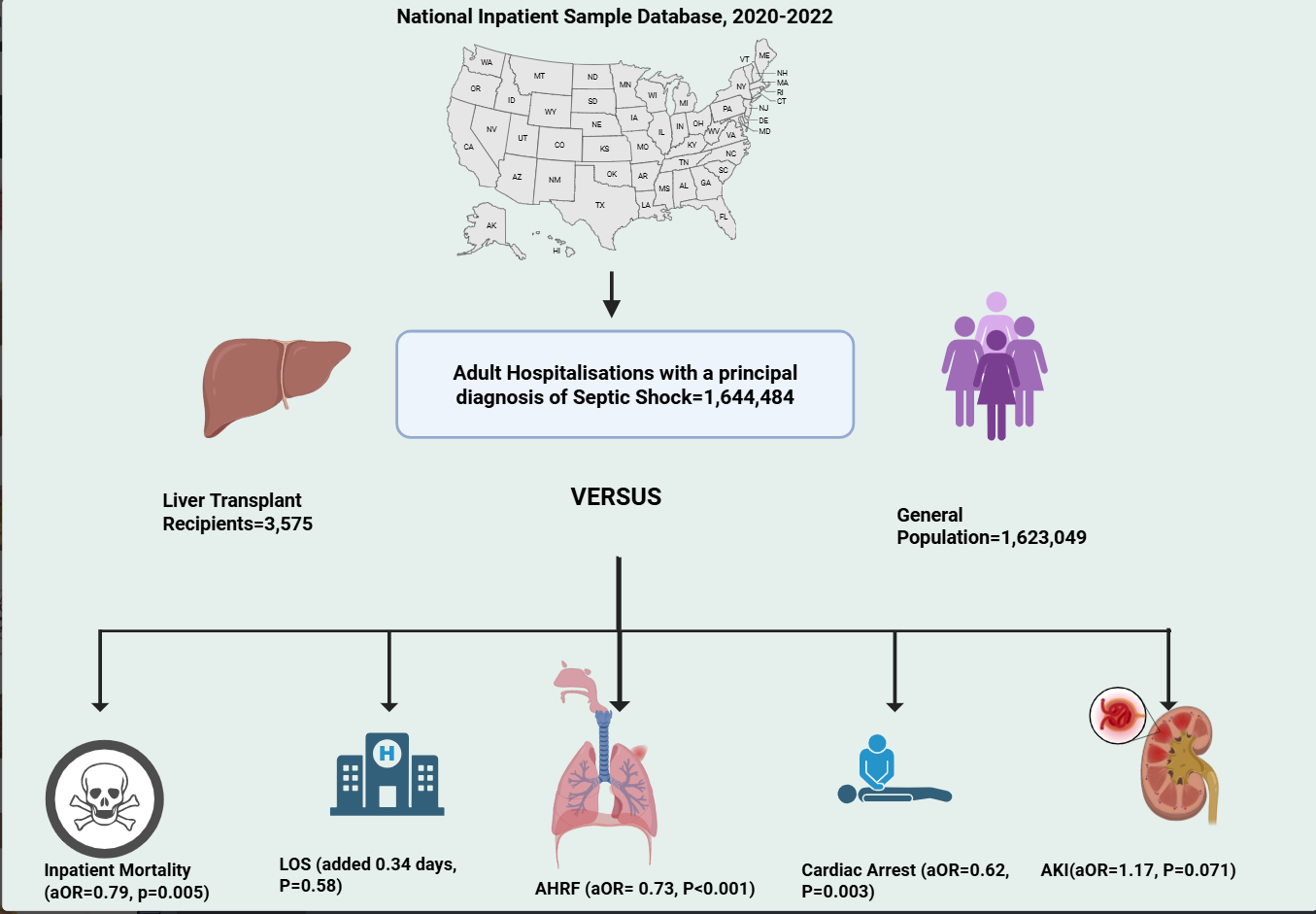
Figure: Table. 1: Baseline Characteristics
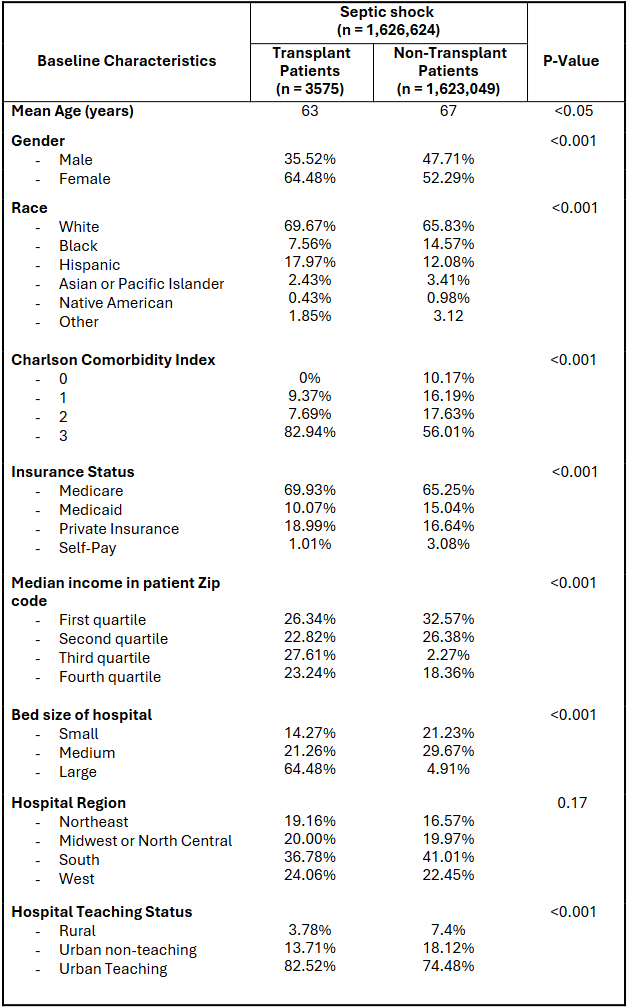
Figure: Inpatient Outcomes Adjusted for Covariates
Disclosures:
Hameed Ullah indicated no relevant financial relationships.
Shahryar Khan indicated no relevant financial relationships.
Mustafa Shah indicated no relevant financial relationships.
Muhammad Arsalan indicated no relevant financial relationships.
Wagmah Khan indicated no relevant financial relationships.
Osama Sherjeel Khan indicated no relevant financial relationships.
Ijaz Ali indicated no relevant financial relationships.
Kamran Qureshi: Gilead Sciences – Speakers Bureau. Intercept Pharmaceuticals – Speakers Bureau. Madrigal Pharmaceuticals – Speakers Bureau. Phathom Pharmaceuticals – Speakers Bureau. Salix Pharmaceuticals – Speakers Bureau.
Hameed Ullah, MD1, Shahryar Khan, MD2, Mustafa Shah, MD3, Muhammad Arsalan, MD1, Wagmah Javed. Khan, MD1, Osama Sherjeel Khan, MD4, Ijaz Ali, MD5, Kamran Qureshi, MD6. P3787 - Outcomes of Septic Shock in Liver Transplant Recipients: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
