Monday Poster Session
Category: Liver
P3778 - Identifying Deficits in Screening for At-Risk Metabolic Dysfunction-Associated Steatohepatitis in an Academic Primary Care Setting: A Quality Improvement Project
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- FA
Farah Abdul Razzak, MD
Detroit Medical Center/Wayne State University
Detroit, MI
Presenting Author(s)
Malek Shatila, MD, Farah Abdul Razzak, MD, Kenan Abou Chaer, MD, Rachel Konchal, MD, Raya Abu Tawileh, MD, Karan Mathur, MD
Detroit Medical Center/Wayne State University, Detroit, MI
Introduction: Current guidelines on metabolic dysfunction-associated steatotic liver disease (MASLD) recommend non-invasive testing such as the Fibrosis-4 (FIB4) score in primary care to assess for advanced liver fibrosis and at-risk metabolic dysfunction-associated steatohepatitis (MASH). This study aims to identify deficits in MASLD screening at our academic primary care setting as part of a quality improvement initiative.
Methods: A series of dedicated ambulatory lectures on MASLD screening were given to Internal Medicine residents by the gastroenterology (GI) fellows and faculty. The lectures were focused on identifying patients seen in primary care for screening of MASLD and discussion regarding invasive and non-invasive testing modalities to assess advanced liver fibrosis and at-risk MASH patients. A survey study done post-lecture intervention revealed a statistically significant improvement in resident knowledge and confidence regarding MASLD screening. Charts of patients seen in IM resident clinics 5 weeks before and after the lecture intervention were then reviewed. Data on demographics, comorbidities, pertinent lab testing, documentation of FIB4 scores, additional non-invasive testing and referral to GI/Hepatology were collected.
Results: A total of 152 patients were included in this study, 38 in the pre-intervention group and 114 in the post-intervention group. Both groups had predominantly female and African American patients. 87% of patients in the pre-intervention group and 75% patients in the post-intervention group were eligible for MASLD screening. There was no documentation of FIB4 scores in the pre-intervention group compared to only 1% in the post-intervention group. 21% patients in pre-intervention group and 27% patients in post-intervention group warranted additional testing/GI referral. 0/7 patients in the pre-intervention group and only 3/23 eligible patients in the post-intervention group were referred to GI/Hepatology for further care.
Discussion: Our findings suggest a continued deficit in MASLD screening at our primary care clinics despite dedicated educational sessions. Possible reasons include decreased awareness among IM attendings regarding MASLD screening and lack of incorporation of MASLD screening in national Internal Medicine guidelines. Future steps in this quality improvement effort would include automation of electronic health record to identify and screen MASLD patients and continued physician education on the topic.
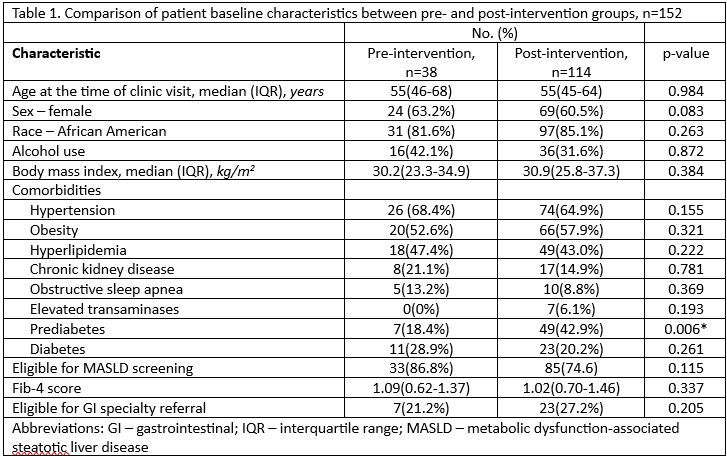
Figure: Figure 1. Patient selection flowchart
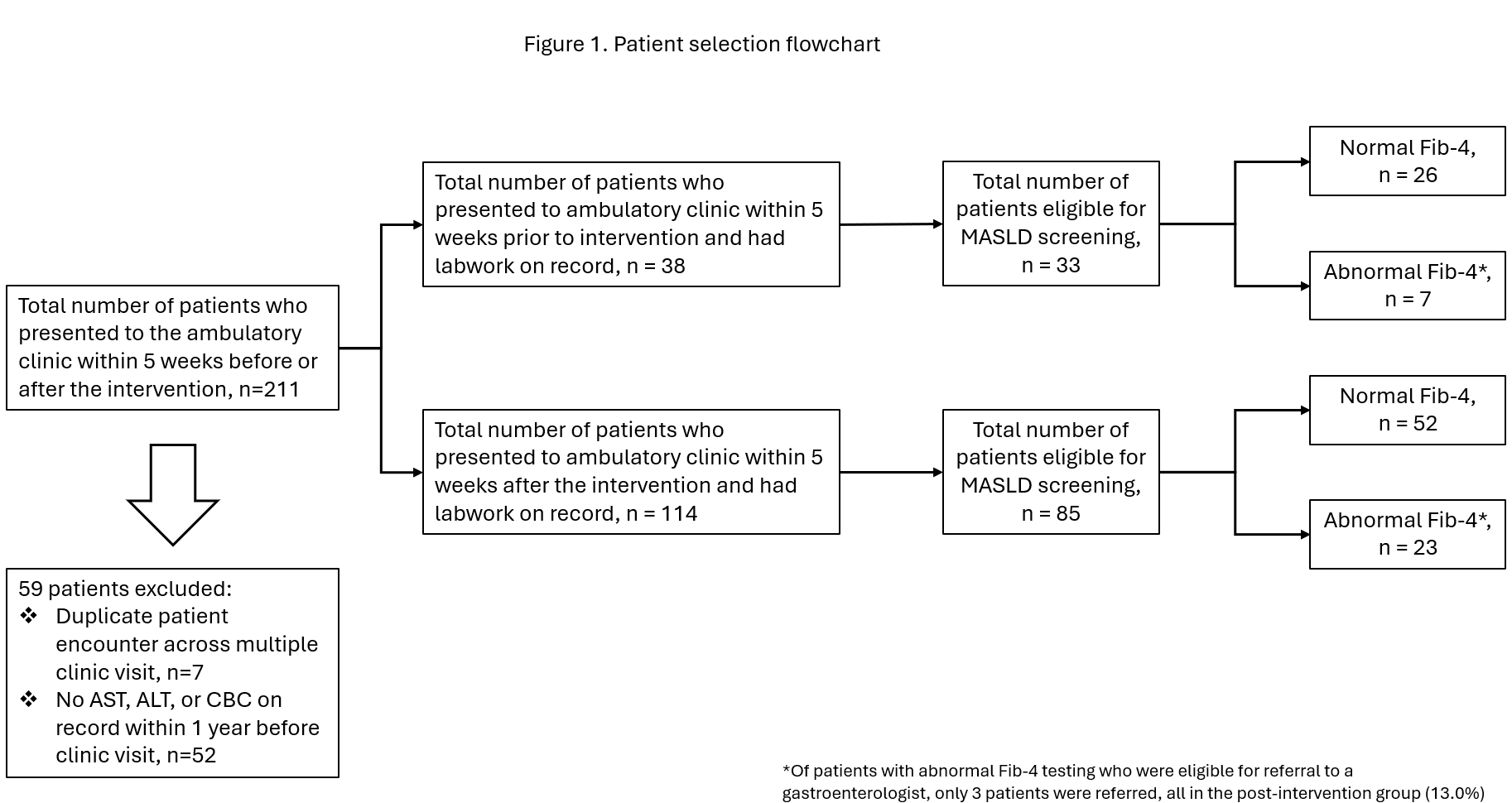
Figure: Table 1. Comparison of patient baseline characteristics between pre- and post-intervention groups
Disclosures:
Malek Shatila indicated no relevant financial relationships.
Farah Abdul Razzak indicated no relevant financial relationships.
Kenan Abou Chaer indicated no relevant financial relationships.
Rachel Konchal indicated no relevant financial relationships.
Raya Abu Tawileh indicated no relevant financial relationships.
Karan Mathur indicated no relevant financial relationships.
Malek Shatila, MD, Farah Abdul Razzak, MD, Kenan Abou Chaer, MD, Rachel Konchal, MD, Raya Abu Tawileh, MD, Karan Mathur, MD. P3778 - Identifying Deficits in Screening for At-Risk Metabolic Dysfunction-Associated Steatohepatitis in an Academic Primary Care Setting: A Quality Improvement Project, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Detroit Medical Center/Wayne State University, Detroit, MI
Introduction: Current guidelines on metabolic dysfunction-associated steatotic liver disease (MASLD) recommend non-invasive testing such as the Fibrosis-4 (FIB4) score in primary care to assess for advanced liver fibrosis and at-risk metabolic dysfunction-associated steatohepatitis (MASH). This study aims to identify deficits in MASLD screening at our academic primary care setting as part of a quality improvement initiative.
Methods: A series of dedicated ambulatory lectures on MASLD screening were given to Internal Medicine residents by the gastroenterology (GI) fellows and faculty. The lectures were focused on identifying patients seen in primary care for screening of MASLD and discussion regarding invasive and non-invasive testing modalities to assess advanced liver fibrosis and at-risk MASH patients. A survey study done post-lecture intervention revealed a statistically significant improvement in resident knowledge and confidence regarding MASLD screening. Charts of patients seen in IM resident clinics 5 weeks before and after the lecture intervention were then reviewed. Data on demographics, comorbidities, pertinent lab testing, documentation of FIB4 scores, additional non-invasive testing and referral to GI/Hepatology were collected.
Results: A total of 152 patients were included in this study, 38 in the pre-intervention group and 114 in the post-intervention group. Both groups had predominantly female and African American patients. 87% of patients in the pre-intervention group and 75% patients in the post-intervention group were eligible for MASLD screening. There was no documentation of FIB4 scores in the pre-intervention group compared to only 1% in the post-intervention group. 21% patients in pre-intervention group and 27% patients in post-intervention group warranted additional testing/GI referral. 0/7 patients in the pre-intervention group and only 3/23 eligible patients in the post-intervention group were referred to GI/Hepatology for further care.
Discussion: Our findings suggest a continued deficit in MASLD screening at our primary care clinics despite dedicated educational sessions. Possible reasons include decreased awareness among IM attendings regarding MASLD screening and lack of incorporation of MASLD screening in national Internal Medicine guidelines. Future steps in this quality improvement effort would include automation of electronic health record to identify and screen MASLD patients and continued physician education on the topic.
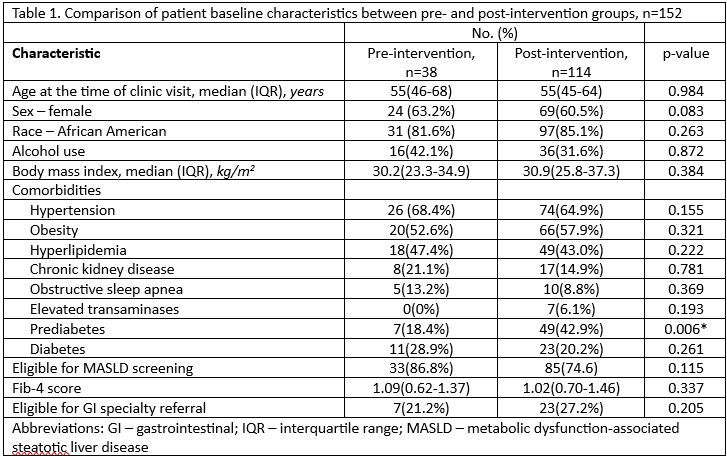
Figure: Figure 1. Patient selection flowchart
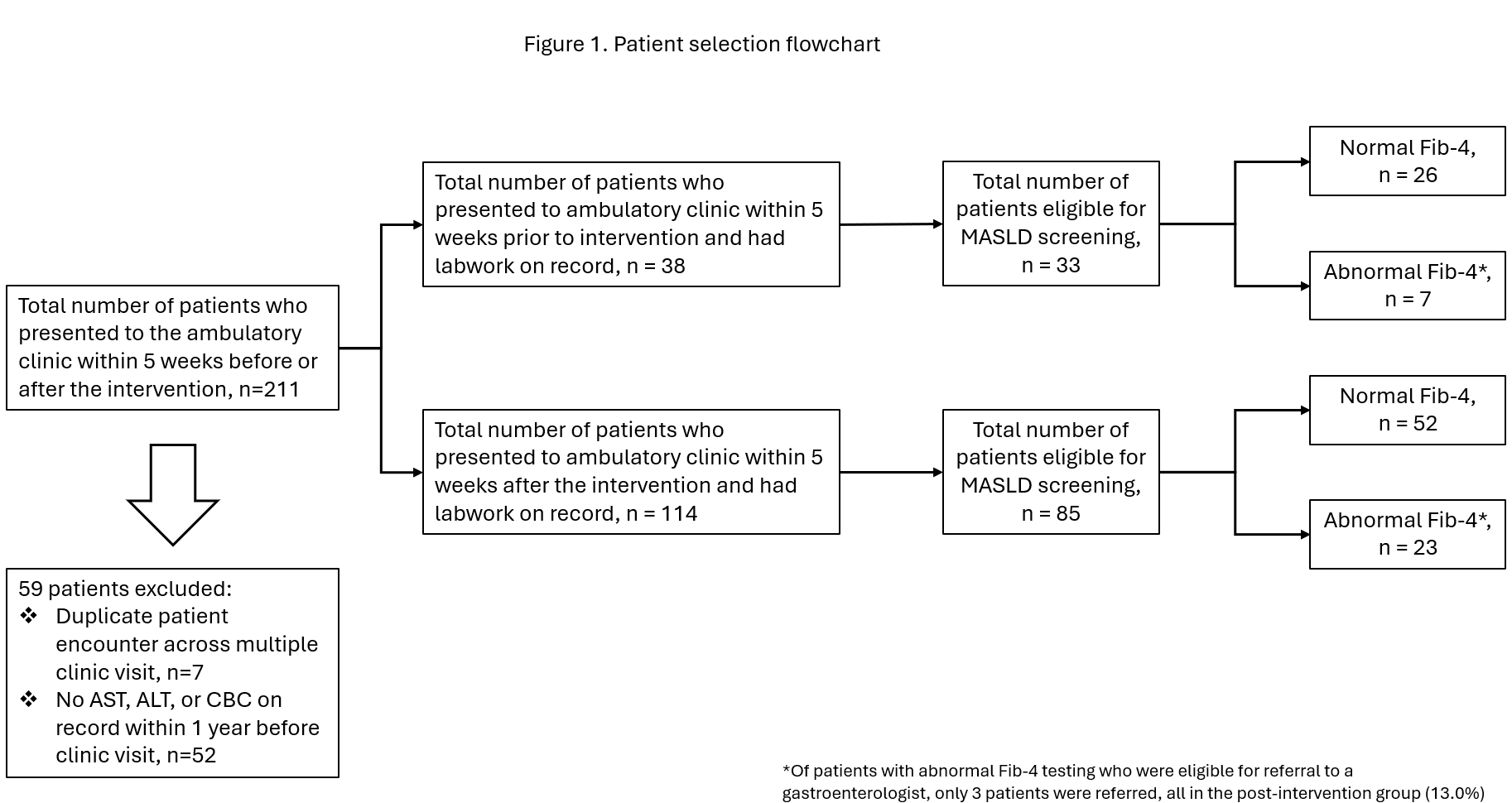
Figure: Table 1. Comparison of patient baseline characteristics between pre- and post-intervention groups
Disclosures:
Malek Shatila indicated no relevant financial relationships.
Farah Abdul Razzak indicated no relevant financial relationships.
Kenan Abou Chaer indicated no relevant financial relationships.
Rachel Konchal indicated no relevant financial relationships.
Raya Abu Tawileh indicated no relevant financial relationships.
Karan Mathur indicated no relevant financial relationships.
Malek Shatila, MD, Farah Abdul Razzak, MD, Kenan Abou Chaer, MD, Rachel Konchal, MD, Raya Abu Tawileh, MD, Karan Mathur, MD. P3778 - Identifying Deficits in Screening for At-Risk Metabolic Dysfunction-Associated Steatohepatitis in an Academic Primary Care Setting: A Quality Improvement Project, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
