Monday Poster Session
Category: Liver
P3775 - Evaluating Outcomes in Patients With MASLD and Vitamin D Deficiency
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Tiana Dodd, DO
Charleston Area Medical Center
Charleston, WV
Presenting Author(s)
Tiana Dodd, DO1, Nisar Amin, MD1, Ebubekir Daglilar, MD1, Nikki Duong, MD2
1Charleston Area Medical Center, Charleston, WV; 2Stanford University, Stanford, CA
Introduction: Vitamin D modulates the expression of receptors and mediators of inflammation in a cell-and-tissue-dependent manner. Patients with MASLD have been found to have lower levels of vitamin D compared to matched controls, with an inverse relationship observed between vitamin D levels and disease severity. This study aims to evaluate outcomes in patients with MASLD with normal vitamin D levels compared to patients with MASLD and vitamin D deficiency.
Methods: This study utilized the TriNetX Research Network and included patients with MASLD or MASH between January 2006- January 2024. The cohorts were defined by a) normal vitamin D levels >30ng/ml and b) vitamin D deficiency defined as < 20 ng/ml. Propensity score matching was performed for the following covariates (age, sex, race, malignancy, heart failure, HTN, COPD, ischemic heart disease, CKD). The primary outcomes were: mortality, hospital readmissions, ICU admissions, and development of cirrhosis at 1 year and 5-year follow-up.
Results: A total of 12,204 patients with MASLD had normal vitamin D levels and 8,933 patients with MASLD had vitamin D deficiency. After 1:1 propensity matching 6,959 patients were included in each group. Patients with vitamin D deficiency were more likely to have hospital readmissions compared to patients with normal vitamin D levels at 1 and 5 years, 10% vs 6.0% (p=0.01) and 15% vs 10% (p=0.01), respectively. Rates of ICU care were increased in patients with vitamin D deficiency at 1 and 5 years, 2.6% vs 1.2% (p=0.01) and 4.4% vs 2.4%, respectively. Progression to cirrhosis was not significant between groups. Mortality rates were increased in patients with vitamin D deficiency compared to patients with normal vitamin D levels at 1 and 5 years 1.5% vs 0.5% (p=0.01) and 3.2% vs 1.3% (p=0.01), respectively.
Discussion: Among patients with MASLD, those with vitamin D deficiency experienced significantly higher rates of hospital readmissions, ICU care, and all-cause mortality at both one- and five-year follow-up compared to those with normal vitamin D levels. These results have identified vitamin D deficiency as a possible risk factor for worse outcomes in patients admitted with MASLD. Future studies are needed to further investigate vitamin D deficiency in patients with liver disease.
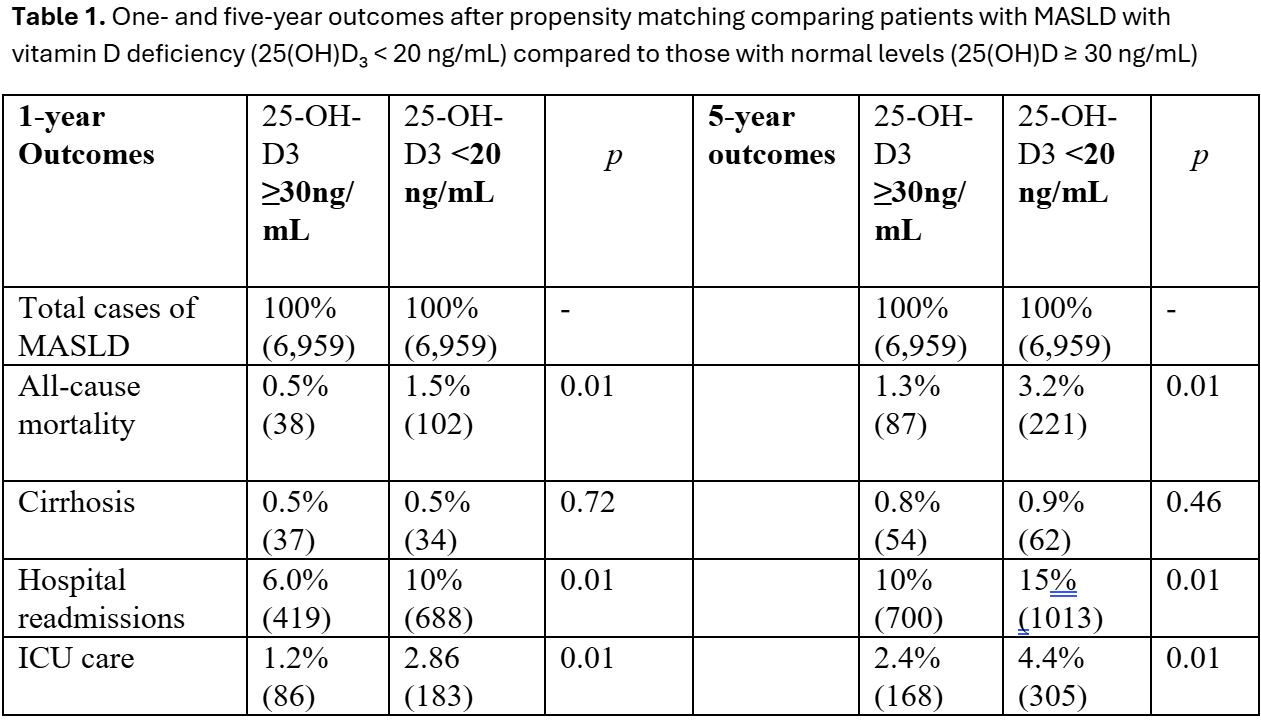
Figure: Table 1. One- and five-year outcomes after propensity matching comparing patients with MASLD with vitamin D deficiency (25(OH)D₃ < 20 ng/mL) compared to those with normal levels (25(OH)D ≥ 30 ng/mL)
Disclosures:
Tiana Dodd indicated no relevant financial relationships.
Nisar Amin indicated no relevant financial relationships.
Ebubekir Daglilar indicated no relevant financial relationships.
Nikki Duong indicated no relevant financial relationships.
Tiana Dodd, DO1, Nisar Amin, MD1, Ebubekir Daglilar, MD1, Nikki Duong, MD2. P3775 - Evaluating Outcomes in Patients With MASLD and Vitamin D Deficiency, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Charleston Area Medical Center, Charleston, WV; 2Stanford University, Stanford, CA
Introduction: Vitamin D modulates the expression of receptors and mediators of inflammation in a cell-and-tissue-dependent manner. Patients with MASLD have been found to have lower levels of vitamin D compared to matched controls, with an inverse relationship observed between vitamin D levels and disease severity. This study aims to evaluate outcomes in patients with MASLD with normal vitamin D levels compared to patients with MASLD and vitamin D deficiency.
Methods: This study utilized the TriNetX Research Network and included patients with MASLD or MASH between January 2006- January 2024. The cohorts were defined by a) normal vitamin D levels >30ng/ml and b) vitamin D deficiency defined as < 20 ng/ml. Propensity score matching was performed for the following covariates (age, sex, race, malignancy, heart failure, HTN, COPD, ischemic heart disease, CKD). The primary outcomes were: mortality, hospital readmissions, ICU admissions, and development of cirrhosis at 1 year and 5-year follow-up.
Results: A total of 12,204 patients with MASLD had normal vitamin D levels and 8,933 patients with MASLD had vitamin D deficiency. After 1:1 propensity matching 6,959 patients were included in each group. Patients with vitamin D deficiency were more likely to have hospital readmissions compared to patients with normal vitamin D levels at 1 and 5 years, 10% vs 6.0% (p=0.01) and 15% vs 10% (p=0.01), respectively. Rates of ICU care were increased in patients with vitamin D deficiency at 1 and 5 years, 2.6% vs 1.2% (p=0.01) and 4.4% vs 2.4%, respectively. Progression to cirrhosis was not significant between groups. Mortality rates were increased in patients with vitamin D deficiency compared to patients with normal vitamin D levels at 1 and 5 years 1.5% vs 0.5% (p=0.01) and 3.2% vs 1.3% (p=0.01), respectively.
Discussion: Among patients with MASLD, those with vitamin D deficiency experienced significantly higher rates of hospital readmissions, ICU care, and all-cause mortality at both one- and five-year follow-up compared to those with normal vitamin D levels. These results have identified vitamin D deficiency as a possible risk factor for worse outcomes in patients admitted with MASLD. Future studies are needed to further investigate vitamin D deficiency in patients with liver disease.
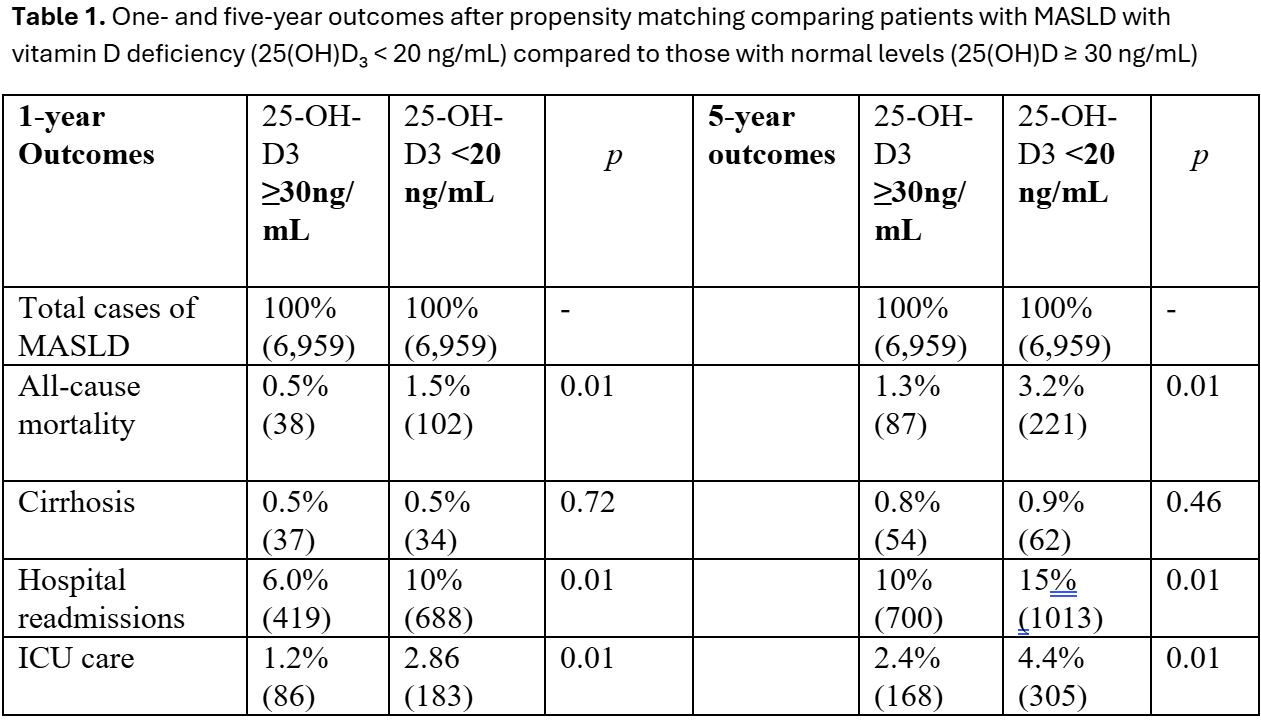
Figure: Table 1. One- and five-year outcomes after propensity matching comparing patients with MASLD with vitamin D deficiency (25(OH)D₃ < 20 ng/mL) compared to those with normal levels (25(OH)D ≥ 30 ng/mL)
Disclosures:
Tiana Dodd indicated no relevant financial relationships.
Nisar Amin indicated no relevant financial relationships.
Ebubekir Daglilar indicated no relevant financial relationships.
Nikki Duong indicated no relevant financial relationships.
Tiana Dodd, DO1, Nisar Amin, MD1, Ebubekir Daglilar, MD1, Nikki Duong, MD2. P3775 - Evaluating Outcomes in Patients With MASLD and Vitamin D Deficiency, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

