Monday Poster Session
Category: Liver
P3772 - Characterization of Cirrhosis Prevalence and Disparities in Linkage to Care Among Underinsured Sexual and Gender Minorities in a Large Public Health System
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Shawn Wen, MD, MS (she/her/hers)
NYU Langone Health, NY
Presenting Author(s)
Shawn Wen, MD, MS, Kripali Gautam, MD, AnnMarie Liapakis, MD
NYU Langone Health, New York, NY
Introduction: Sexual and gender minorities (SGM) are disproportionately affected by conditions that increase chronic liver disease risk, including viral hepatitis, alcohol use, diabetes, and obesity. However, data on cirrhosis prevalence among SGM is limited. This is the first study to describe cirrhosis prevalence, etiologies, and linkage to care in a predominantly Medicaid-insured SGM population.
Methods: In our large, urban public hospital system, we identified adults with an ICD diagnosis of cirrhosis and self-reported sexual orientation and gender identity (SOGI) data from January 1, 2000 to May 1, 2025. Charts were reviewed to confirm cirrhosis (by imaging, elastography, or biopsy), determine etiology, and assess linkage to care defined as a gastroenterology or hepatology clinic visit in the last year. These outcomes were analyzed with descriptive statistics and compared to a non-SGM straight, cisgender cohort.
Results: Of 7,451,107 adult patients in the system during the study period, 758,840 (10.2%) had SOGI data. 44,507 (5.9% of patients with SOGI data) identified as SGM. Ninety-five SGM and 2,506 non-SGM patients had cirrhosis. The SGM group was younger (mean age 53.2 vs. 60.3 years, p< 0.05). Both cohorts were predominantly Hispanic (53.7% SGM vs. 57.5% non-SGM), male sex at birth (77.9% vs. 68.9%), and Medicaid-enrolled (62.1% vs. 55.7%) (Table 1). Gay (47.4%) and cisgender men (62.1%) were the most represented identities in the SGM cohort.
SGM had a lower cirrhosis prevalence (213 per 100,000; 95% CI 175–261) than non-SGM (351 per 100,000; CI 337–365). Leading causes in SGM were alcohol (54.7%, CI 44.7–64.4%) and viral hepatitis (26.3%, CI 18.5–36.0%), similar to non-SGM (Tables 2 & 3). Linkage to liver specialty care was low in both groups (37.9% SGM, CI 28.8–47.9%; 36.7% non-SGM, CI 34.8–38.6%).
Discussion: Despite lower observed cirrhosis prevalence in SGM, the figure is likely underestimated. Only 10% of patients had SOGI data, underscoring the need for expanded SOGI collection. This study is a critical step in understanding cirrhosis among SGM individuals with intersecting minority identities (SGM, Hispanic, underinsured) that impact access to care. Two-thirds of SGM patients with cirrhosis are not linked to specialty care. Future work includes expanding SOGI collection and developing targeted pathways to close care gaps. The younger age in SGM with cirrhosis also warrants further study, as it may reflect earlier exposure to risk factors leading to accelerated disease progression.
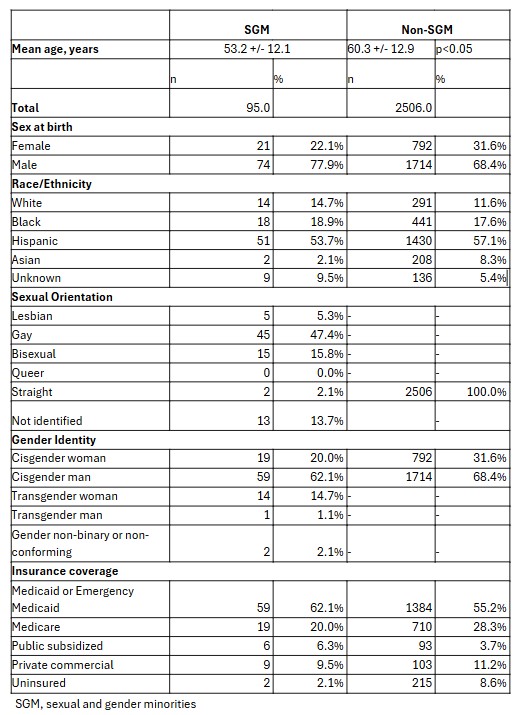
Figure: Table 1: Demographic Characteristics
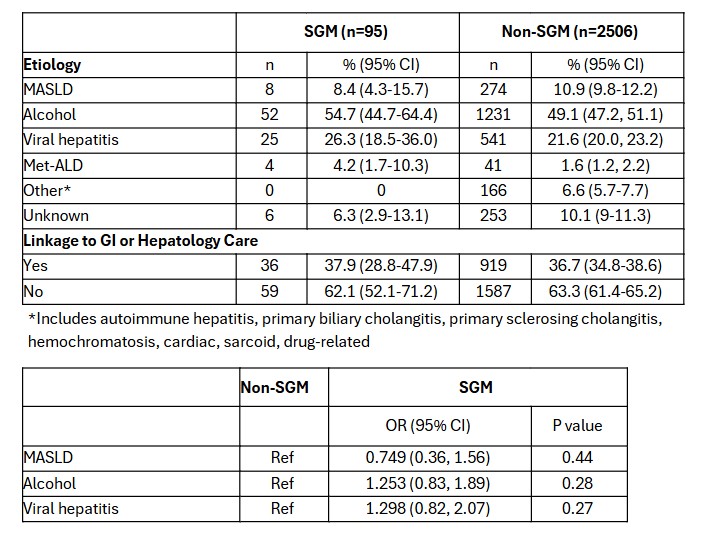
Figure: Table 2: Etiologies of Cirrhosis and Care Linkage
Table 3: Odds Ratios of Leading Cirrhosis Etiologies
Disclosures:
Shawn Wen indicated no relevant financial relationships.
Kripali Gautam indicated no relevant financial relationships.
AnnMarie Liapakis indicated no relevant financial relationships.
Shawn Wen, MD, MS, Kripali Gautam, MD, AnnMarie Liapakis, MD. P3772 - Characterization of Cirrhosis Prevalence and Disparities in Linkage to Care Among Underinsured Sexual and Gender Minorities in a Large Public Health System, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
NYU Langone Health, New York, NY
Introduction: Sexual and gender minorities (SGM) are disproportionately affected by conditions that increase chronic liver disease risk, including viral hepatitis, alcohol use, diabetes, and obesity. However, data on cirrhosis prevalence among SGM is limited. This is the first study to describe cirrhosis prevalence, etiologies, and linkage to care in a predominantly Medicaid-insured SGM population.
Methods: In our large, urban public hospital system, we identified adults with an ICD diagnosis of cirrhosis and self-reported sexual orientation and gender identity (SOGI) data from January 1, 2000 to May 1, 2025. Charts were reviewed to confirm cirrhosis (by imaging, elastography, or biopsy), determine etiology, and assess linkage to care defined as a gastroenterology or hepatology clinic visit in the last year. These outcomes were analyzed with descriptive statistics and compared to a non-SGM straight, cisgender cohort.
Results: Of 7,451,107 adult patients in the system during the study period, 758,840 (10.2%) had SOGI data. 44,507 (5.9% of patients with SOGI data) identified as SGM. Ninety-five SGM and 2,506 non-SGM patients had cirrhosis. The SGM group was younger (mean age 53.2 vs. 60.3 years, p< 0.05). Both cohorts were predominantly Hispanic (53.7% SGM vs. 57.5% non-SGM), male sex at birth (77.9% vs. 68.9%), and Medicaid-enrolled (62.1% vs. 55.7%) (Table 1). Gay (47.4%) and cisgender men (62.1%) were the most represented identities in the SGM cohort.
SGM had a lower cirrhosis prevalence (213 per 100,000; 95% CI 175–261) than non-SGM (351 per 100,000; CI 337–365). Leading causes in SGM were alcohol (54.7%, CI 44.7–64.4%) and viral hepatitis (26.3%, CI 18.5–36.0%), similar to non-SGM (Tables 2 & 3). Linkage to liver specialty care was low in both groups (37.9% SGM, CI 28.8–47.9%; 36.7% non-SGM, CI 34.8–38.6%).
Discussion: Despite lower observed cirrhosis prevalence in SGM, the figure is likely underestimated. Only 10% of patients had SOGI data, underscoring the need for expanded SOGI collection. This study is a critical step in understanding cirrhosis among SGM individuals with intersecting minority identities (SGM, Hispanic, underinsured) that impact access to care. Two-thirds of SGM patients with cirrhosis are not linked to specialty care. Future work includes expanding SOGI collection and developing targeted pathways to close care gaps. The younger age in SGM with cirrhosis also warrants further study, as it may reflect earlier exposure to risk factors leading to accelerated disease progression.
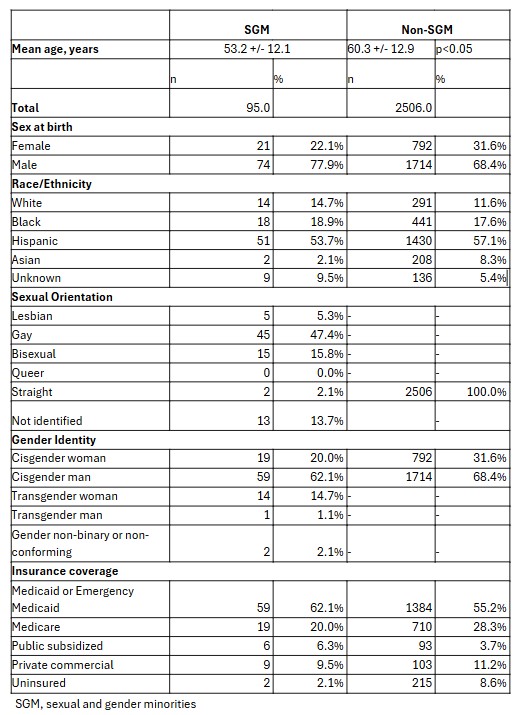
Figure: Table 1: Demographic Characteristics
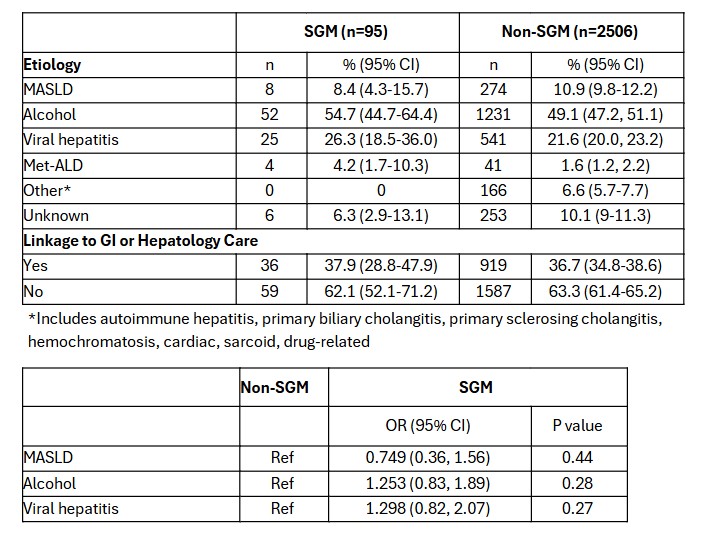
Figure: Table 2: Etiologies of Cirrhosis and Care Linkage
Table 3: Odds Ratios of Leading Cirrhosis Etiologies
Disclosures:
Shawn Wen indicated no relevant financial relationships.
Kripali Gautam indicated no relevant financial relationships.
AnnMarie Liapakis indicated no relevant financial relationships.
Shawn Wen, MD, MS, Kripali Gautam, MD, AnnMarie Liapakis, MD. P3772 - Characterization of Cirrhosis Prevalence and Disparities in Linkage to Care Among Underinsured Sexual and Gender Minorities in a Large Public Health System, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
