Monday Poster Session
Category: Liver
P3871 - Neonatal Acute Liver Failure from Gestational Alloimmune Liver Disease: Distinct Outcomes in Two Infants
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Airam Rangel, MD (she/her/hers)
Memorial Healthcare System
Pembroke Pines, FL
Presenting Author(s)
Airam Rangel, MD1, Palack Agrawal, MD1, Laura Molineros, MD1, Bin Wang, MD, PhD2
1Memorial Healthcare System, Pembroke Pines, FL; 2Memorial Healthcare System, Hollywood, FL
Introduction: Gestational Alloimmune Liver Disease (GALD) is rare but the leading cause of neonatal acute liver failure (NALF), triggered by maternal alloantibodies against fetal hepatocytes. This causes complement mediated hepatocyte injury and systemic iron overload. Despite advances in imaging and immunotherapy (IVIG, exchange transfusion), GALD remains under-recognized and often fatal without timely treatment. We present two cases highlighting variability in presentation, diagnostic challenges, and outcomes.
Case Description/
Methods: Case 1:
A 36-week male born via vaginal delivery for maternal preeclampsia, discharged home on day of life (DOL) 2. On DOL 13, he presented with fussiness and hypothermia but was discharged with reassurance. He returned the next day with jaundice, hypoglycemia (39 mg/dL), and shock. Labs showed total bilirubin 34 mg/dL, INR >8, and ammonia 119 µmol/L. He was admitted to PICU and treated with exchange transfusion, IVIG, and plasma exchange for presumed GALD. Buccal biopsy was negative; MRI on DOL 25 showed diffuse siderosis. He developed multiorgan failure and necrotizing enterocolitis. Care was withdrawn on DOL 36. Postmortem autopsy confirmed GALD.
Case 2:
A 32+1-week female born via cesarean section for oligohydramnios, requiring CPAP and presenting with blueberry muffin lesions. On DOL 1, she developed hypotension, acidosis, and pneumothorax. She received steroids, vasopressors, and IVIG on DOL 2. Liver dysfunction progressed (bilirubin 23.5 mg/dL, INR 2.9). Buccal biopsy on DOL 8 confirmed GALD. She received two additional IVIG doses and one exchange transfusion. Complications included MSSA bacteremia, GI bleeding, and renal failure requiring ultrafiltration. She stabilized and was transferred for transplant evaluation.
Discussion: These cases illustrate the critical importance of early detection and prompt treatment. In Case 1, late presentation (DOL 14) contributed to delayed diagnosis and poorer outcome. Diagnostic delays are common, as GALD may be misattributed to metabolic, infectious, or genetic etiologies. While buccal biopsy is minimally invasive, it may yield false negatives in early or preterm infants due to insufficient or immature glandular tissue. MRI serves as a valuable non-invasive tool for confirmation. The standard treatment involves IVIG, with or without exchange transfusion; therapeutic plasma exchange remains investigational. Maintaining a high index of suspicion is essential for improving survival and reducing the need for liver transplantation.
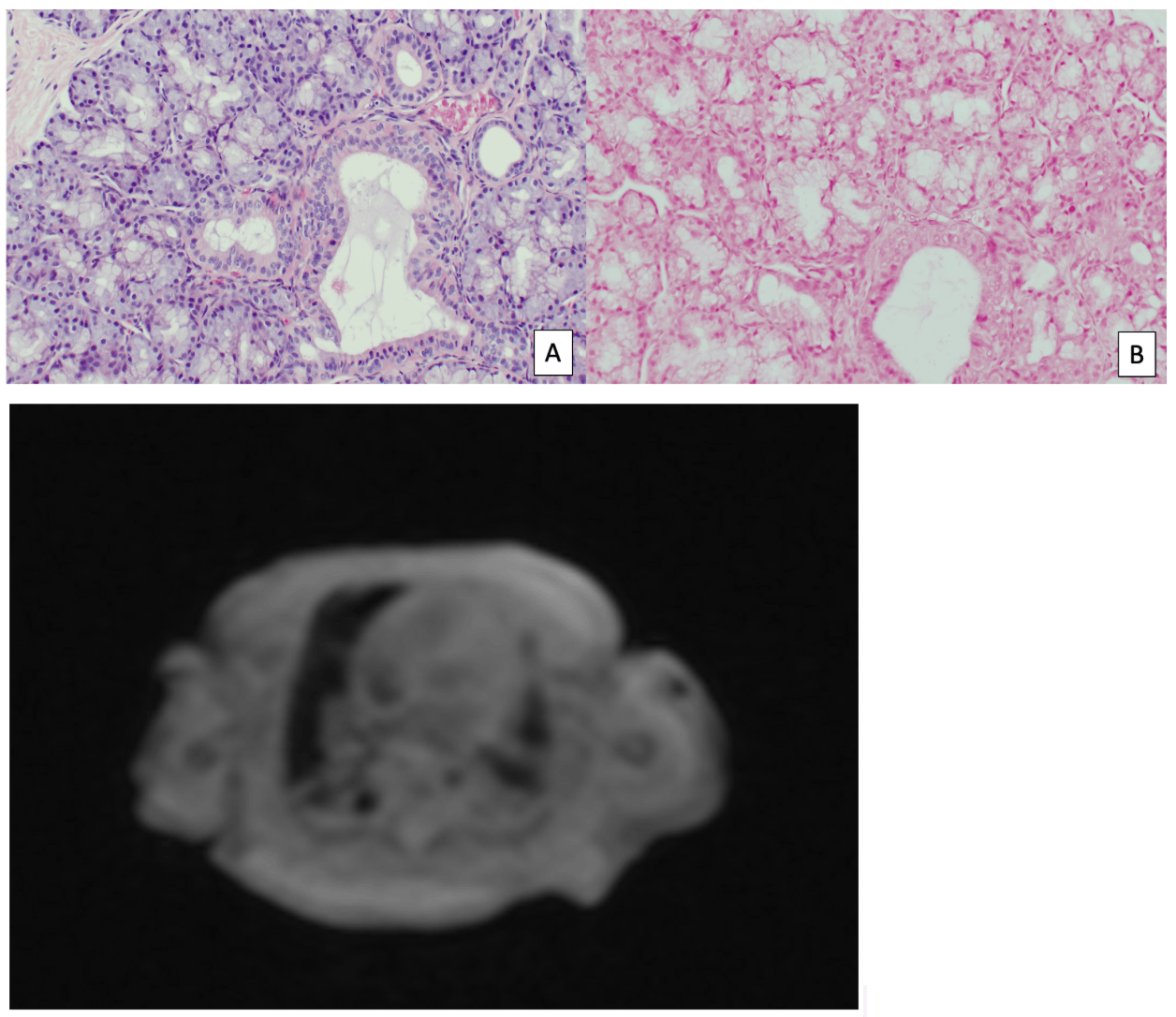
Figure: Case 1- Buccal biopsy: salivary gland with no evidence of iron deposition on Prussian blue iron stained (B)
Abdominal MRI without contrast with decreased T2 signal intensity in the pancreatic head and neck suggesting iron overload.
Figure: Case 2- Buccal biopsy: salivary gland with evidence of iron deposition. B. Prussian blue stain highlights the iron deposition in blue (arrows)
Disclosures:
Airam Rangel indicated no relevant financial relationships.
Palack Agrawal indicated no relevant financial relationships.
Laura Molineros indicated no relevant financial relationships.
Bin Wang indicated no relevant financial relationships.
Airam Rangel, MD1, Palack Agrawal, MD1, Laura Molineros, MD1, Bin Wang, MD, PhD2. P3871 - Neonatal Acute Liver Failure from Gestational Alloimmune Liver Disease: Distinct Outcomes in Two Infants, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Memorial Healthcare System, Pembroke Pines, FL; 2Memorial Healthcare System, Hollywood, FL
Introduction: Gestational Alloimmune Liver Disease (GALD) is rare but the leading cause of neonatal acute liver failure (NALF), triggered by maternal alloantibodies against fetal hepatocytes. This causes complement mediated hepatocyte injury and systemic iron overload. Despite advances in imaging and immunotherapy (IVIG, exchange transfusion), GALD remains under-recognized and often fatal without timely treatment. We present two cases highlighting variability in presentation, diagnostic challenges, and outcomes.
Case Description/
Methods: Case 1:
A 36-week male born via vaginal delivery for maternal preeclampsia, discharged home on day of life (DOL) 2. On DOL 13, he presented with fussiness and hypothermia but was discharged with reassurance. He returned the next day with jaundice, hypoglycemia (39 mg/dL), and shock. Labs showed total bilirubin 34 mg/dL, INR >8, and ammonia 119 µmol/L. He was admitted to PICU and treated with exchange transfusion, IVIG, and plasma exchange for presumed GALD. Buccal biopsy was negative; MRI on DOL 25 showed diffuse siderosis. He developed multiorgan failure and necrotizing enterocolitis. Care was withdrawn on DOL 36. Postmortem autopsy confirmed GALD.
Case 2:
A 32+1-week female born via cesarean section for oligohydramnios, requiring CPAP and presenting with blueberry muffin lesions. On DOL 1, she developed hypotension, acidosis, and pneumothorax. She received steroids, vasopressors, and IVIG on DOL 2. Liver dysfunction progressed (bilirubin 23.5 mg/dL, INR 2.9). Buccal biopsy on DOL 8 confirmed GALD. She received two additional IVIG doses and one exchange transfusion. Complications included MSSA bacteremia, GI bleeding, and renal failure requiring ultrafiltration. She stabilized and was transferred for transplant evaluation.
Discussion: These cases illustrate the critical importance of early detection and prompt treatment. In Case 1, late presentation (DOL 14) contributed to delayed diagnosis and poorer outcome. Diagnostic delays are common, as GALD may be misattributed to metabolic, infectious, or genetic etiologies. While buccal biopsy is minimally invasive, it may yield false negatives in early or preterm infants due to insufficient or immature glandular tissue. MRI serves as a valuable non-invasive tool for confirmation. The standard treatment involves IVIG, with or without exchange transfusion; therapeutic plasma exchange remains investigational. Maintaining a high index of suspicion is essential for improving survival and reducing the need for liver transplantation.
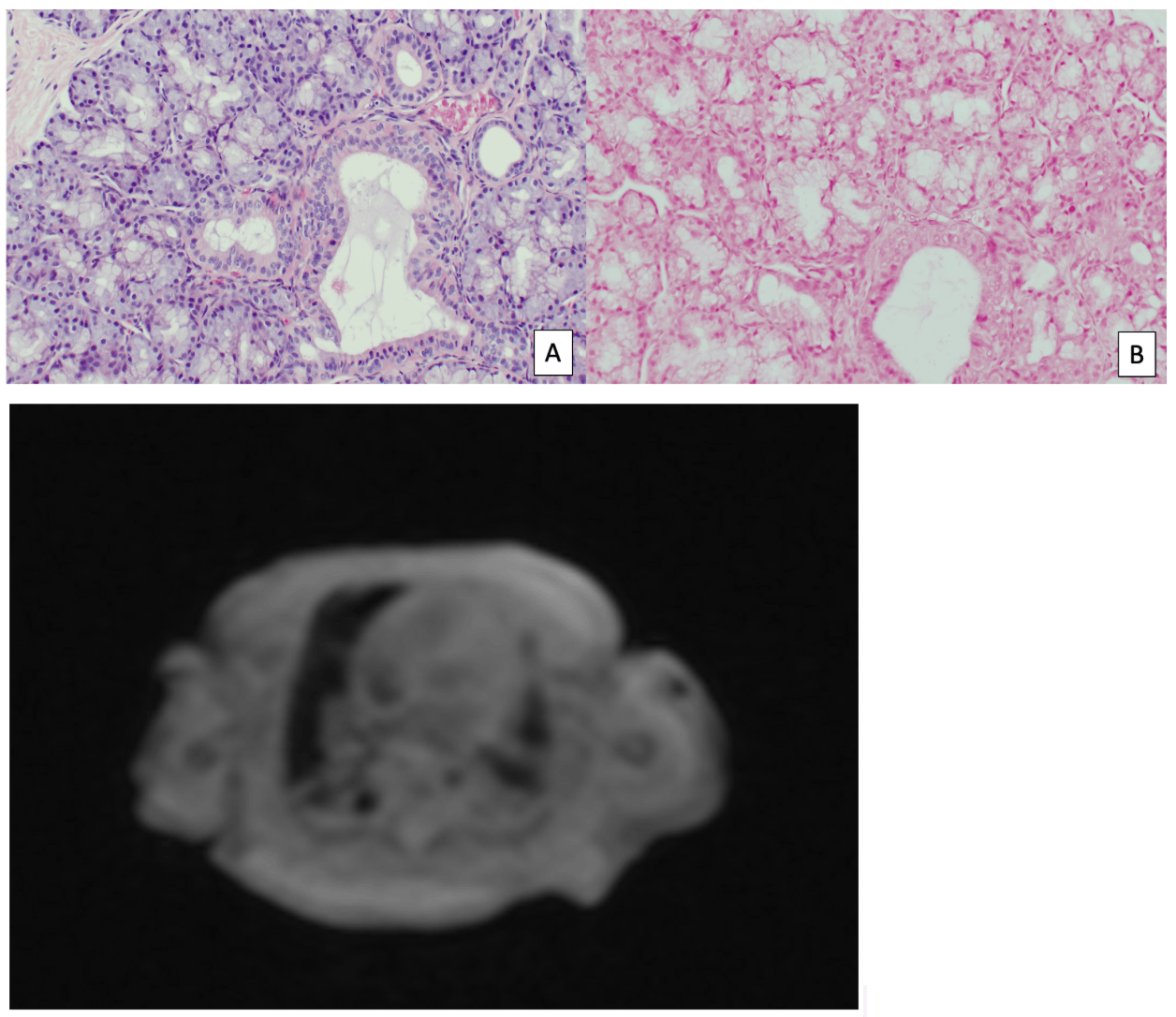
Figure: Case 1- Buccal biopsy: salivary gland with no evidence of iron deposition on Prussian blue iron stained (B)
Abdominal MRI without contrast with decreased T2 signal intensity in the pancreatic head and neck suggesting iron overload.
Figure: Case 2- Buccal biopsy: salivary gland with evidence of iron deposition. B. Prussian blue stain highlights the iron deposition in blue (arrows)
Disclosures:
Airam Rangel indicated no relevant financial relationships.
Palack Agrawal indicated no relevant financial relationships.
Laura Molineros indicated no relevant financial relationships.
Bin Wang indicated no relevant financial relationships.
Airam Rangel, MD1, Palack Agrawal, MD1, Laura Molineros, MD1, Bin Wang, MD, PhD2. P3871 - Neonatal Acute Liver Failure from Gestational Alloimmune Liver Disease: Distinct Outcomes in Two Infants, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
