Monday Poster Session
Category: Liver
P3864 - A Double Challenge: Acute Liver Rejection and Subsequent Biliary Stricture After Transplantation
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- NP
Namrata Paladugu, MD (she/her/hers)
University of Mississippi Medical Center
Jackson, MS
Presenting Author(s)
Namrata Paladugu, MD, Anna Lauren G. Winter, MD, Aneeq Muhammad Yousuf, MD, Klara Missling, BA, Yassmin Hegazy, MD, Laura Smart, MD, Faisal A. Bukeirat, MD, Joydeep Chakraborty, MD
University of Mississippi Medical Center, Jackson, MS
Introduction: Both acute liver allograft rejection and biliary obstruction can present with elevated liver enzymes and cholestasis. Though biliary obstruction is not typically directly associated with acute liver allograft rejection, they can rarely coexist and distinguishing between them is critical for management.
Case Description/
Methods: A 67-year-old female with history of decompensated cirrhosis due to metabolic-dysfunction associated steatohepatitis underwent orthotopic deceased donor liver transplant with choledocho-choledochostomy anastomosis 3 years prior. She had no previous history of rejection or biliary issues. On admission, labs showed a mixed pattern of liver injury with R-factor of 2.9, alanine transaminase (ALT) of 438 U/L, alkaline phosphatase (ALP) of 461 U/L, total bilirubin (Tbil) level of 2.1 mg/dL, predominantly direct. Immunosuppression included Tacrolimus within therapeutic goal and mycophenolate mofetil. Infectious and viral workup was negative. Liver ultrasound (US) had patent hepatic vasculature and no biliary dilation. Liver biopsy showed severe acute cellular rejection (ACR) with a Banff Rejection Activity Index (RAI) of 8/9. A total of 3g of methylprednisolone was given, followed by a total of 9 mg/kg of anti-thymocyte globulin (ATG) due to steroid-refractory rejection. ALT improved but ALP and Tbil worsened to a cholestatic pattern with R-factor of 0.7. Repeat liver biopsy revealed resolution of rejection but suspicion of biliary outflow obstruction. Magnetic resonance imaging with magnetic resonance cholangiopancreatography (MRCP) (Image 1) showed mild intrahepatic biliary dilation and choledocholithiasis proximal to the biliary anastomosis. Endoscopic retrograde cholangiopancreatography confirmed a tight biliary anastomotic stricture and small biliary stones (Image 2). After balloon dilation, stone extraction, and plastic stent placement, liver enzymes and Tbil remarkably improved.
Discussion: Our case exemplifies a patient presenting initially with biopsy proven severe ACR but subsequent worsening cholestasis despite appropriate therapy and resolution of ACR on biopsy lead to further evaluation, diagnosis and successful management of biliary anastomotic stricture, leading to clinical recovery. Studies have reported history of graft rejection as a risk factor for biliary anastomotic stricture. US abdomen has lower sensitivity in diagnosing biliary obstruction in post liver transplant patients, therefore MRCP should be utilized for initial evaluation in such cases.

Figure: Image 1. MRCP with evidence of biliary anastomotic stricture (red arrow)
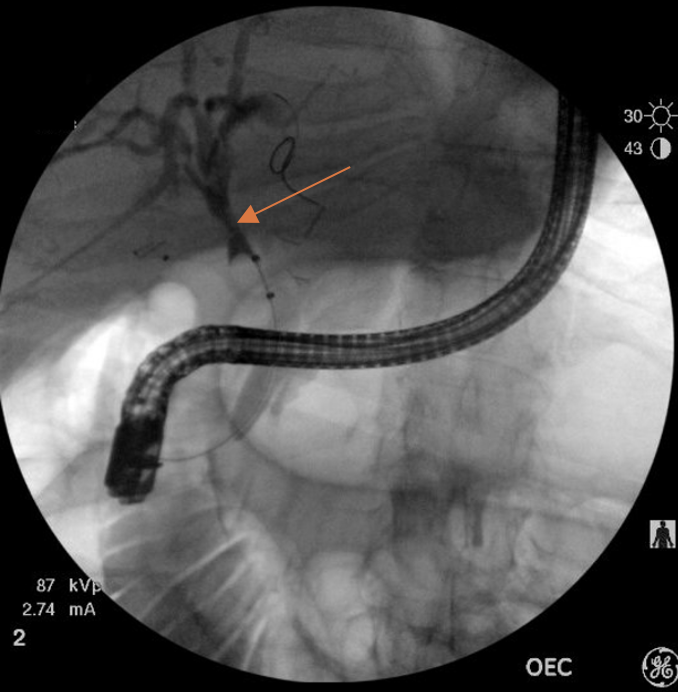
Figure: Image 2. Very tight choledocho-choledochostomy anastomotic stricture (red arrow) noted on ERCP
Disclosures:
Namrata Paladugu indicated no relevant financial relationships.
Anna Lauren Winter indicated no relevant financial relationships.
Aneeq Muhammad Yousuf indicated no relevant financial relationships.
Klara Missling indicated no relevant financial relationships.
Yassmin Hegazy indicated no relevant financial relationships.
Laura Smart indicated no relevant financial relationships.
Faisal Bukeirat indicated no relevant financial relationships.
Joydeep Chakraborty indicated no relevant financial relationships.
Namrata Paladugu, MD, Anna Lauren G. Winter, MD, Aneeq Muhammad Yousuf, MD, Klara Missling, BA, Yassmin Hegazy, MD, Laura Smart, MD, Faisal A. Bukeirat, MD, Joydeep Chakraborty, MD. P3864 - A Double Challenge: Acute Liver Rejection and Subsequent Biliary Stricture After Transplantation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Mississippi Medical Center, Jackson, MS
Introduction: Both acute liver allograft rejection and biliary obstruction can present with elevated liver enzymes and cholestasis. Though biliary obstruction is not typically directly associated with acute liver allograft rejection, they can rarely coexist and distinguishing between them is critical for management.
Case Description/
Methods: A 67-year-old female with history of decompensated cirrhosis due to metabolic-dysfunction associated steatohepatitis underwent orthotopic deceased donor liver transplant with choledocho-choledochostomy anastomosis 3 years prior. She had no previous history of rejection or biliary issues. On admission, labs showed a mixed pattern of liver injury with R-factor of 2.9, alanine transaminase (ALT) of 438 U/L, alkaline phosphatase (ALP) of 461 U/L, total bilirubin (Tbil) level of 2.1 mg/dL, predominantly direct. Immunosuppression included Tacrolimus within therapeutic goal and mycophenolate mofetil. Infectious and viral workup was negative. Liver ultrasound (US) had patent hepatic vasculature and no biliary dilation. Liver biopsy showed severe acute cellular rejection (ACR) with a Banff Rejection Activity Index (RAI) of 8/9. A total of 3g of methylprednisolone was given, followed by a total of 9 mg/kg of anti-thymocyte globulin (ATG) due to steroid-refractory rejection. ALT improved but ALP and Tbil worsened to a cholestatic pattern with R-factor of 0.7. Repeat liver biopsy revealed resolution of rejection but suspicion of biliary outflow obstruction. Magnetic resonance imaging with magnetic resonance cholangiopancreatography (MRCP) (Image 1) showed mild intrahepatic biliary dilation and choledocholithiasis proximal to the biliary anastomosis. Endoscopic retrograde cholangiopancreatography confirmed a tight biliary anastomotic stricture and small biliary stones (Image 2). After balloon dilation, stone extraction, and plastic stent placement, liver enzymes and Tbil remarkably improved.
Discussion: Our case exemplifies a patient presenting initially with biopsy proven severe ACR but subsequent worsening cholestasis despite appropriate therapy and resolution of ACR on biopsy lead to further evaluation, diagnosis and successful management of biliary anastomotic stricture, leading to clinical recovery. Studies have reported history of graft rejection as a risk factor for biliary anastomotic stricture. US abdomen has lower sensitivity in diagnosing biliary obstruction in post liver transplant patients, therefore MRCP should be utilized for initial evaluation in such cases.

Figure: Image 1. MRCP with evidence of biliary anastomotic stricture (red arrow)
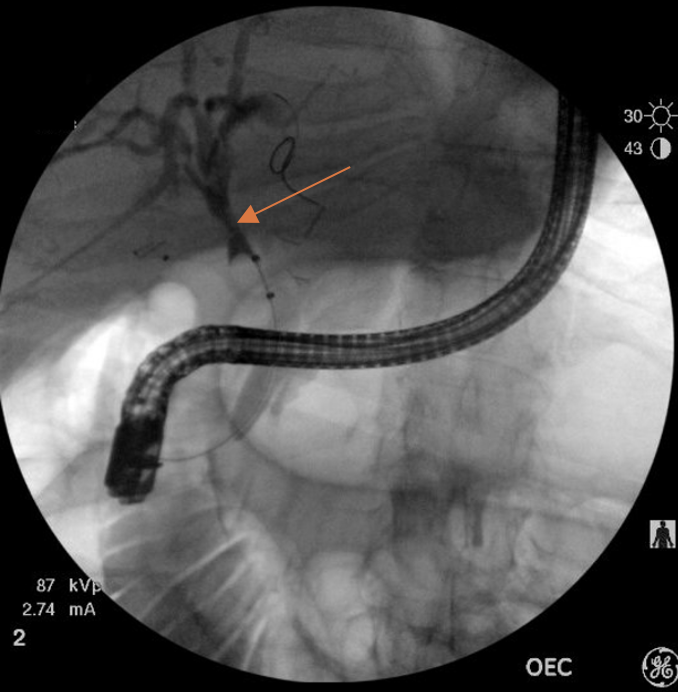
Figure: Image 2. Very tight choledocho-choledochostomy anastomotic stricture (red arrow) noted on ERCP
Disclosures:
Namrata Paladugu indicated no relevant financial relationships.
Anna Lauren Winter indicated no relevant financial relationships.
Aneeq Muhammad Yousuf indicated no relevant financial relationships.
Klara Missling indicated no relevant financial relationships.
Yassmin Hegazy indicated no relevant financial relationships.
Laura Smart indicated no relevant financial relationships.
Faisal Bukeirat indicated no relevant financial relationships.
Joydeep Chakraborty indicated no relevant financial relationships.
Namrata Paladugu, MD, Anna Lauren G. Winter, MD, Aneeq Muhammad Yousuf, MD, Klara Missling, BA, Yassmin Hegazy, MD, Laura Smart, MD, Faisal A. Bukeirat, MD, Joydeep Chakraborty, MD. P3864 - A Double Challenge: Acute Liver Rejection and Subsequent Biliary Stricture After Transplantation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
