Monday Poster Session
Category: Liver
P3854 - Alcoholic Hepatitis with Hepatic Encephalopathy Mimicking HLH: A Diagnostic Challenge in a Patient With HIV
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Brian Kim, MD
Rutgers New Jersey Medical School
Kearny, NJ
Presenting Author(s)
Brian Kim, MD1, Dhir Gala, MD2, Menna-Allah Elaskandrany, DO3, Mary Morgan, MD2
1Rutgers New Jersey Medical School, Kearny, NJ; 2Rutgers New Jersey Medical School, Newark, NJ; 3Lenox Hill Hospital, Northwell Health, New York, NY
Introduction: Alcohol-associated hepatitis can present with systemic inflammation and lab abnormalities that overlap with other critical conditions like hemophagocytic lymphohistiocytosis (HLH). The H-score is often used to assess the likelihood of HLH, but many of its components such as cytopenias, hyperferritinemia, and transaminitis can also be seen in advanced liver injury. This case highlights a scenario in which a high H-score prompted concern for HLH, but the underlying diagnosis was hepatic encephalopathy in the setting of alcoholic hepatitis.
Case Description/
Methods: A 41-year-old woman with a past medical history of HIV on ART, and alcohol use disorder presented with progressive jaundice, fatigue, and altered mental status. At presentation, she was febrile and encephalopathic with asterixis noted on physical exam. Labs showed AST 421, ALT 33, total bilirubin 27.0, INR 2.2, sodium 132, and creatinine 4.8. MELD-Na was 40. Imaging showed hepatomegaly with steatosis, splenomegaly, and mild gallbladder wall thickening.
Given the presence of fever, hyperferritinemia over 10,000, hypertriglyceridemia, splenomegaly, and borderline cytopenias, HLH was strongly considered. Her calculated H-score ranged from 202 to 226, depending on the inclusion of variables like bone marrow biopsy that were not performed. Hematology was consulted, and further workup including IL-2 receptor (2172), EBV PCR, and flow cytometry was sent. She was treated for alcohol-associated hepatitis with hepatic encephalopathy using NAC, lactulose, rifaximin, ursodiol, thiamine, zinc, and albumin. Steroids were deferred due to concern for infection. Despite the H-score high score, she remained afebrile after admission, and her labs trended down with supportive care alone. HLH-specific therapy was not started. Her mental status and renal function improved, and she was discharged on hospital day nine with a MELD-Na of 22.
Discussion: This case shows how alcohol-associated hepatitis with hepatic encephalopathy can closely mimic HLH, especially in a patient with HIV. While the H-score can be a helpful tool, it may be falsely elevated in liver conditions where systemic inflammation is already present. It’s important to interpret the score in the full clinical context. A careful look at the patient’s history, comorbidities, and response to treatment is essential to avoid unnecessary immunosuppression.
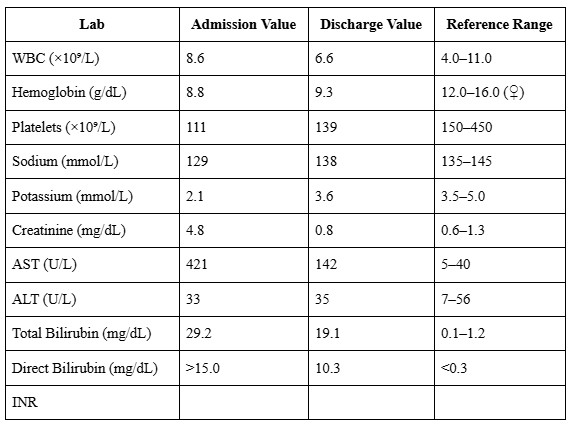
Figure: H-Score calculation demonstrating elevated risk for hemophagocytic lymphohistiocytosis (HLH) based on initial clinical and laboratory findings.
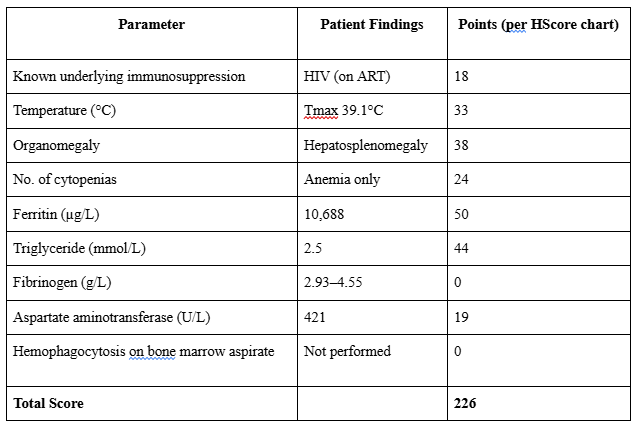
Figure: Comparison of selected laboratory values on admission vs discharge, illustrating clinical improvement with treatment for hepatic encephalopathy and alcohol-associated hepatitis.
Disclosures:
Brian Kim indicated no relevant financial relationships.
Dhir Gala indicated no relevant financial relationships.
Menna-Allah Elaskandrany indicated no relevant financial relationships.
Mary Morgan indicated no relevant financial relationships.
Brian Kim, MD1, Dhir Gala, MD2, Menna-Allah Elaskandrany, DO3, Mary Morgan, MD2. P3854 - Alcoholic Hepatitis with Hepatic Encephalopathy Mimicking HLH: A Diagnostic Challenge in a Patient With HIV, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Kearny, NJ; 2Rutgers New Jersey Medical School, Newark, NJ; 3Lenox Hill Hospital, Northwell Health, New York, NY
Introduction: Alcohol-associated hepatitis can present with systemic inflammation and lab abnormalities that overlap with other critical conditions like hemophagocytic lymphohistiocytosis (HLH). The H-score is often used to assess the likelihood of HLH, but many of its components such as cytopenias, hyperferritinemia, and transaminitis can also be seen in advanced liver injury. This case highlights a scenario in which a high H-score prompted concern for HLH, but the underlying diagnosis was hepatic encephalopathy in the setting of alcoholic hepatitis.
Case Description/
Methods: A 41-year-old woman with a past medical history of HIV on ART, and alcohol use disorder presented with progressive jaundice, fatigue, and altered mental status. At presentation, she was febrile and encephalopathic with asterixis noted on physical exam. Labs showed AST 421, ALT 33, total bilirubin 27.0, INR 2.2, sodium 132, and creatinine 4.8. MELD-Na was 40. Imaging showed hepatomegaly with steatosis, splenomegaly, and mild gallbladder wall thickening.
Given the presence of fever, hyperferritinemia over 10,000, hypertriglyceridemia, splenomegaly, and borderline cytopenias, HLH was strongly considered. Her calculated H-score ranged from 202 to 226, depending on the inclusion of variables like bone marrow biopsy that were not performed. Hematology was consulted, and further workup including IL-2 receptor (2172), EBV PCR, and flow cytometry was sent. She was treated for alcohol-associated hepatitis with hepatic encephalopathy using NAC, lactulose, rifaximin, ursodiol, thiamine, zinc, and albumin. Steroids were deferred due to concern for infection. Despite the H-score high score, she remained afebrile after admission, and her labs trended down with supportive care alone. HLH-specific therapy was not started. Her mental status and renal function improved, and she was discharged on hospital day nine with a MELD-Na of 22.
Discussion: This case shows how alcohol-associated hepatitis with hepatic encephalopathy can closely mimic HLH, especially in a patient with HIV. While the H-score can be a helpful tool, it may be falsely elevated in liver conditions where systemic inflammation is already present. It’s important to interpret the score in the full clinical context. A careful look at the patient’s history, comorbidities, and response to treatment is essential to avoid unnecessary immunosuppression.
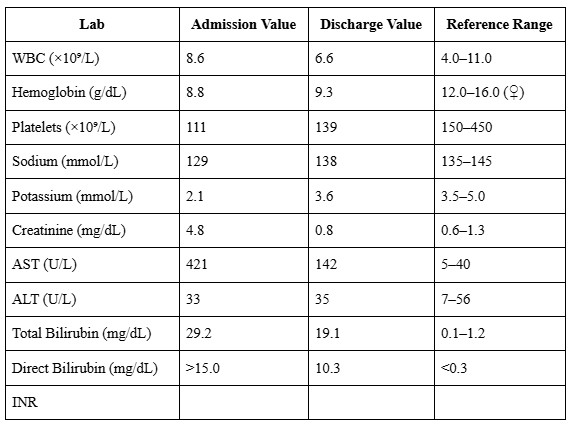
Figure: H-Score calculation demonstrating elevated risk for hemophagocytic lymphohistiocytosis (HLH) based on initial clinical and laboratory findings.
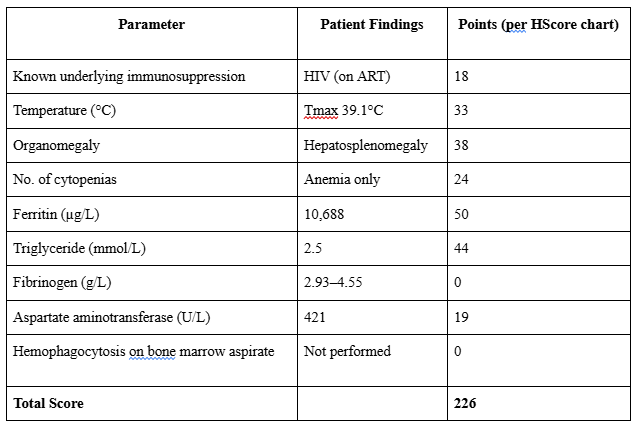
Figure: Comparison of selected laboratory values on admission vs discharge, illustrating clinical improvement with treatment for hepatic encephalopathy and alcohol-associated hepatitis.
Disclosures:
Brian Kim indicated no relevant financial relationships.
Dhir Gala indicated no relevant financial relationships.
Menna-Allah Elaskandrany indicated no relevant financial relationships.
Mary Morgan indicated no relevant financial relationships.
Brian Kim, MD1, Dhir Gala, MD2, Menna-Allah Elaskandrany, DO3, Mary Morgan, MD2. P3854 - Alcoholic Hepatitis with Hepatic Encephalopathy Mimicking HLH: A Diagnostic Challenge in a Patient With HIV, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
