Monday Poster Session
Category: Liver
P3954 - Simultaneous Orthotopic Liver and Heart Transplantation in a Patient With Propionic Acidemia and Cardiomyopathy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

M Housam Nanah, MD
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
M Housam Nanah, MD1, Anh Bui, DO2, Tesfaye Yadete, MD3, Abdullah Hafeez, MD4, Jamile Wakim-Fleming, MD1
1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland Heights, OH; 3Cleveland Clinic Foundation, Cleveland, OH; 4Landmark Medical Center, Woonsocket, RI
Introduction: Propionic acidemia (PA) is a rare, autosomal recessive metabolic disorder caused by propionyl-CoA carboxylase deficiency, resulting in impaired amino acid and lipid metabolism. Severe complications may include cardiomyopathy, liver dysfunction, and neurologic impairment. While liver transplantation (LT) for PA has been documented to improve metabolic control, simultaneous liver and heart transplantation remains rare and less well-established.
Case Description/
Methods: An 18-year-old male with PA, diagnosed via newborn screening with the common Amish variant, presented to our tertiary care center with nausea, dry heaving, and shortness of breath. He developed progressive cardiomyopathy, and echocardiography revealed an ejection fraction of 17% and a severely dilated left ventricle, consistent with end-stage heart failure. He was referred for management and transplant evaluation. An Impella 5.5 device was placed for temporary hemodynamic support. Following a 63-day inpatient course, the patient underwent successful simultaneous orthotopic liver and heart transplantation. His postoperative course was uneventful, and he was discharged in stable condition. At four-month follow-up, echocardiogram showed an EF of 58%, and he remained clinically stable without hospital readmissions or metabolic decompensations.
Discussion: Propionic acidemia is part of a broader group of organic acidemias with an incidence ranging from 1 in 10,000 to 1 in 1,000,000 live births. It results in the multisystemic accumulation of toxic metabolites due to defective propionyl-CoA carboxylase activity. Our case involves severe cardiac involvement due to PA thereby liver and heart transplant were necessary. This case illustrates the feasibility and potential benefits of simultaneous liver-heart transplantation in patients with irreversible cardiac dysfunction due to PA. It also underscores the importance of early cardiac surveillance in this population. At follow-up, the patient demonstrated both metabolic and cardiac recovery, highlighting the possible reversal of cardiac dysfunction with appropriate surgical intervention.
Future directions include the need for longitudinal studies and registry data to evaluate long-term graft outcomes, quality of life, and metabolic control in patients undergoing combined organ transplantation. Additionally, investigating genotype–phenotype correlations, such as the impact of the Amish variant on cardiac involvement, may aid in earlier identification of transplant candidates.
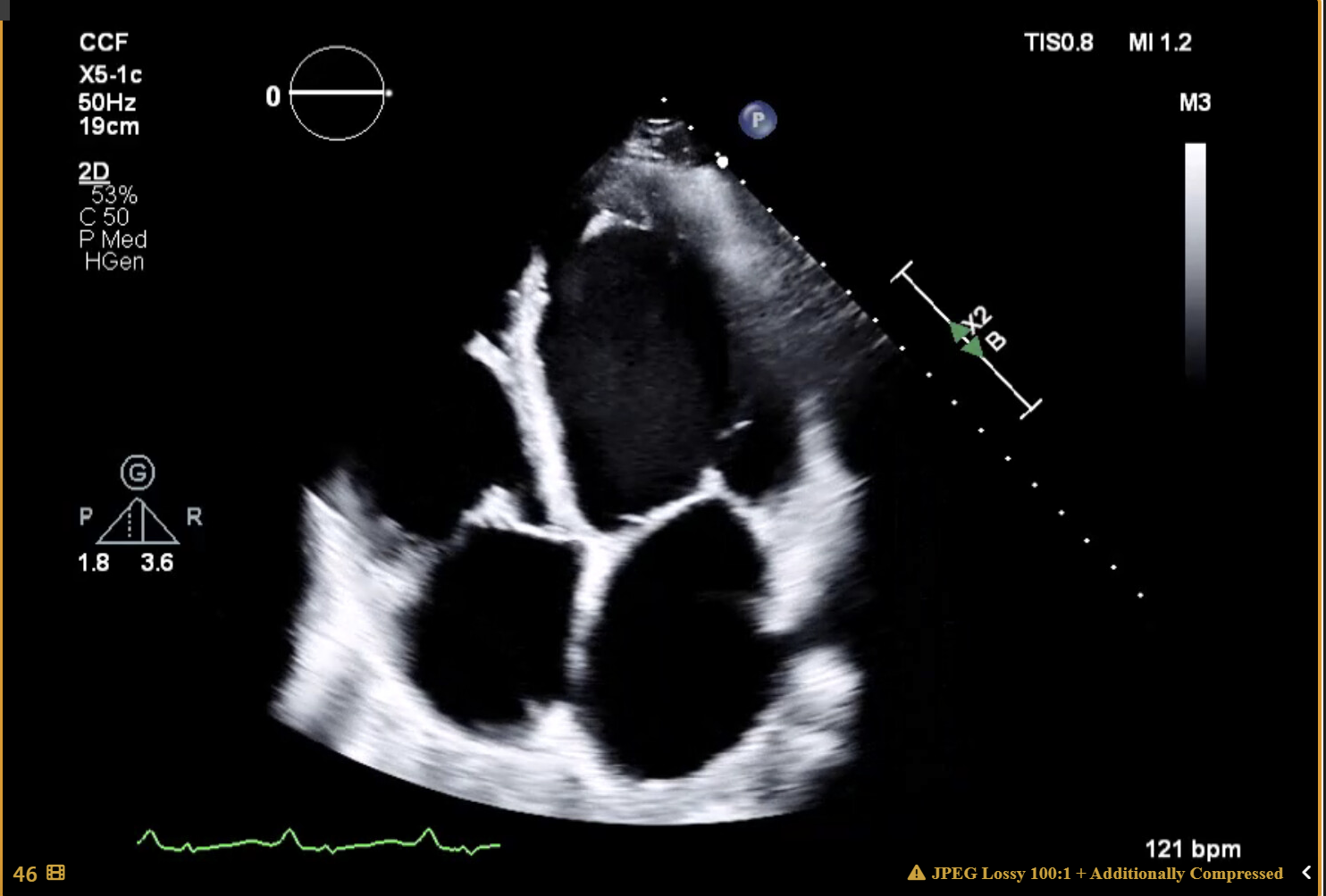
Figure: The left ventricle is severely dilated. Left ventricular systolic function is
severely decreased. EF = 17 ± 5% (2D 4-ch.)
Disclosures:
M Housam Nanah indicated no relevant financial relationships.
Anh Bui indicated no relevant financial relationships.
Tesfaye Yadete indicated no relevant financial relationships.
Abdullah Hafeez indicated no relevant financial relationships.
Jamile Wakim-Fleming indicated no relevant financial relationships.
M Housam Nanah, MD1, Anh Bui, DO2, Tesfaye Yadete, MD3, Abdullah Hafeez, MD4, Jamile Wakim-Fleming, MD1. P3954 - Simultaneous Orthotopic Liver and Heart Transplantation in a Patient With Propionic Acidemia and Cardiomyopathy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland Heights, OH; 3Cleveland Clinic Foundation, Cleveland, OH; 4Landmark Medical Center, Woonsocket, RI
Introduction: Propionic acidemia (PA) is a rare, autosomal recessive metabolic disorder caused by propionyl-CoA carboxylase deficiency, resulting in impaired amino acid and lipid metabolism. Severe complications may include cardiomyopathy, liver dysfunction, and neurologic impairment. While liver transplantation (LT) for PA has been documented to improve metabolic control, simultaneous liver and heart transplantation remains rare and less well-established.
Case Description/
Methods: An 18-year-old male with PA, diagnosed via newborn screening with the common Amish variant, presented to our tertiary care center with nausea, dry heaving, and shortness of breath. He developed progressive cardiomyopathy, and echocardiography revealed an ejection fraction of 17% and a severely dilated left ventricle, consistent with end-stage heart failure. He was referred for management and transplant evaluation. An Impella 5.5 device was placed for temporary hemodynamic support. Following a 63-day inpatient course, the patient underwent successful simultaneous orthotopic liver and heart transplantation. His postoperative course was uneventful, and he was discharged in stable condition. At four-month follow-up, echocardiogram showed an EF of 58%, and he remained clinically stable without hospital readmissions or metabolic decompensations.
Discussion: Propionic acidemia is part of a broader group of organic acidemias with an incidence ranging from 1 in 10,000 to 1 in 1,000,000 live births. It results in the multisystemic accumulation of toxic metabolites due to defective propionyl-CoA carboxylase activity. Our case involves severe cardiac involvement due to PA thereby liver and heart transplant were necessary. This case illustrates the feasibility and potential benefits of simultaneous liver-heart transplantation in patients with irreversible cardiac dysfunction due to PA. It also underscores the importance of early cardiac surveillance in this population. At follow-up, the patient demonstrated both metabolic and cardiac recovery, highlighting the possible reversal of cardiac dysfunction with appropriate surgical intervention.
Future directions include the need for longitudinal studies and registry data to evaluate long-term graft outcomes, quality of life, and metabolic control in patients undergoing combined organ transplantation. Additionally, investigating genotype–phenotype correlations, such as the impact of the Amish variant on cardiac involvement, may aid in earlier identification of transplant candidates.
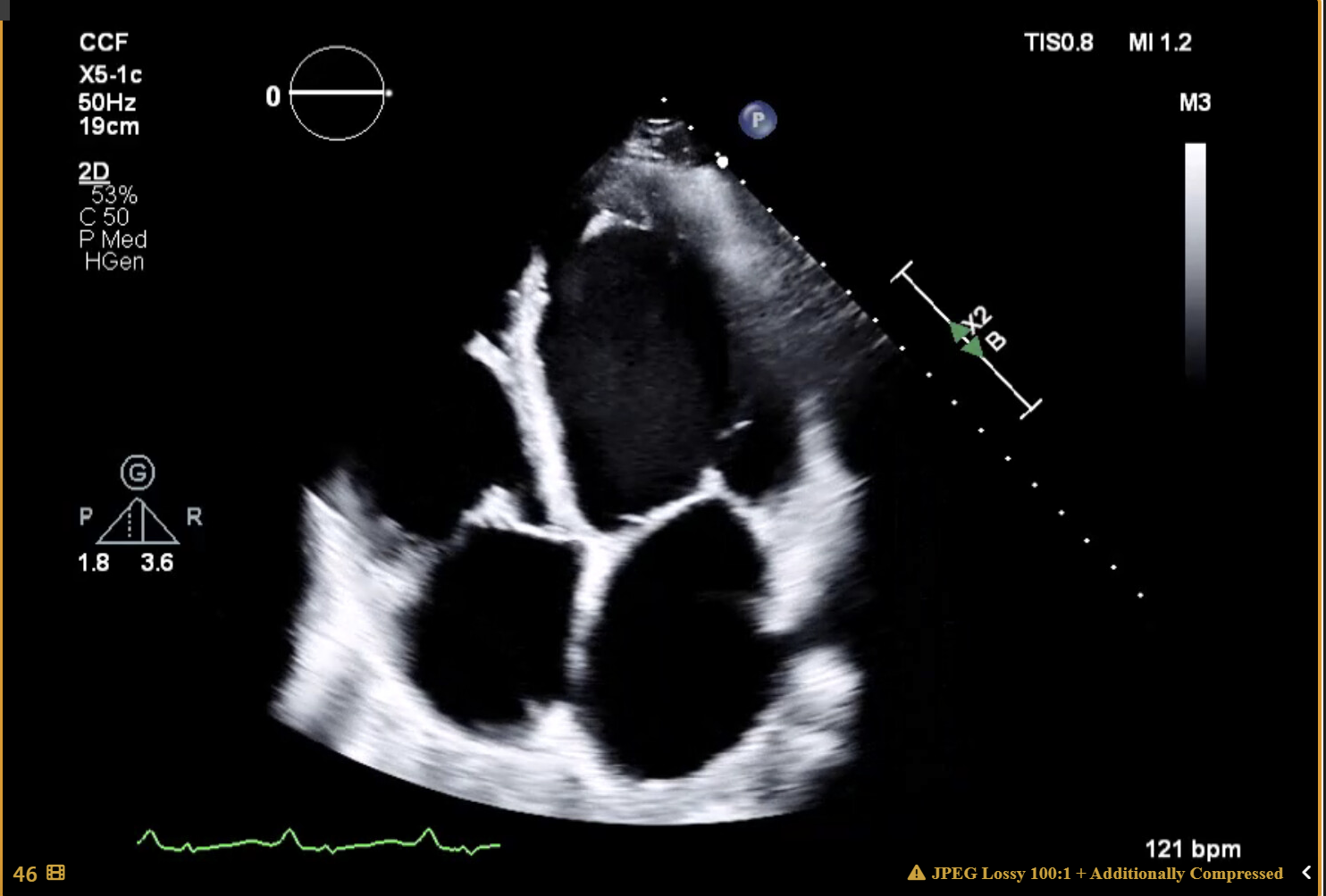
Figure: The left ventricle is severely dilated. Left ventricular systolic function is
severely decreased. EF = 17 ± 5% (2D 4-ch.)
Disclosures:
M Housam Nanah indicated no relevant financial relationships.
Anh Bui indicated no relevant financial relationships.
Tesfaye Yadete indicated no relevant financial relationships.
Abdullah Hafeez indicated no relevant financial relationships.
Jamile Wakim-Fleming indicated no relevant financial relationships.
M Housam Nanah, MD1, Anh Bui, DO2, Tesfaye Yadete, MD3, Abdullah Hafeez, MD4, Jamile Wakim-Fleming, MD1. P3954 - Simultaneous Orthotopic Liver and Heart Transplantation in a Patient With Propionic Acidemia and Cardiomyopathy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
