Monday Poster Session
Category: Small Intestine
P4024 - Inpatient Enteroscopy in Celiac Disease: A Cross-Sectional Analysis of Utilization, Diagnostic Yield, and Clinical Outcomes From a Nationwide Dataset
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- RU
Rahat Uddin, MS
SUNY Downstate Health Sciences University
Brooklyn, NY
Presenting Author(s)
Anwar Uddin, MD, Rahat Uddin, MS, Madia Ahad, MD, Peter Lymberopoulos, MD, Savanna Thor, DO, MPH
SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Celiac disease (CD) is a chronic immune-mediated enteropathy that may warrant advanced small bowel evaluation in cases of refractory symptoms, alarm features, or suspected malignancy. Enteroscopy enables deep small bowel visualization and tissue diagnosis but is infrequently performed during hospitalization. Despite its utility, data on its inpatient use, diagnostic yield, and associated outcomes are limited. This study examined national trends, diagnostic performance, and short-term clinical outcomes of inpatient enteroscopy in hospitalized CD patients.
Methods: We performed a retrospective cross-sectional analysis of adult CD hospitalizations in HCUP-NIS (2016–2020). CD and enteroscopy were identified using ICD-10-CM code K90.0 and ICD-10-PCS codes, respectively. Primary outcomes: in-hospital mortality, LOS, and cost. Secondary outcomes: GIST, small bowel adenocarcinoma, and complications (bleeding, pancreatitis, ileus). Survey-weighted multivariable models estimated adjusted odds ratios (aOR), rate ratios, and costs, adjusting for age, sex, race, insurance, Charlson index, and hospital factors.
Results: Among 190,235 CD hospitalizations (2016–2020), only 55 (0.03%) involved inpatient enteroscopy, with no significant change in utilization over time (p = 0.7). Enteroscopy was associated with significantly longer LOS (13.6 ± 3.5 vs 4.6 ± 0.03 days; aRR 2.44, 95% CI: 1.45–4.12; p < 0.001) and higher hospitalization costs ($42,242 vs $14,156; aRR 2.74, 95% CI: 1.38–5.47; p = 0.004). In-hospital mortality was numerically higher (9.1% vs 1.4%) but not statistically significant (aOR 4.1, 95% CI: 0.36–46.7; p = 0.3). Diagnostic yield was notably elevated: small bowel adenocarcinoma and GIST were detected in 14.5% and 12.7% of enteroscopy patients vs 0.09% and 0.03% in controls (aOR 61.2 and 79.3; both p < 0.001). No major complications occurred. These findings suggest inpatient enteroscopy, though rarely used, is highly effective for malignancy detection in high-risk CD cases without observed harm.
Discussion: Inpatient enteroscopy is infrequently used in hospitalized celiac disease patients but is strongly associated with increased diagnostic yield for small bowel malignancies and higher resource utilization. These findings support its targeted use in selected high-risk populations and underscore the need for prospective studies to refine its inpatient role, optimize timing, and guide clinical decision-making.
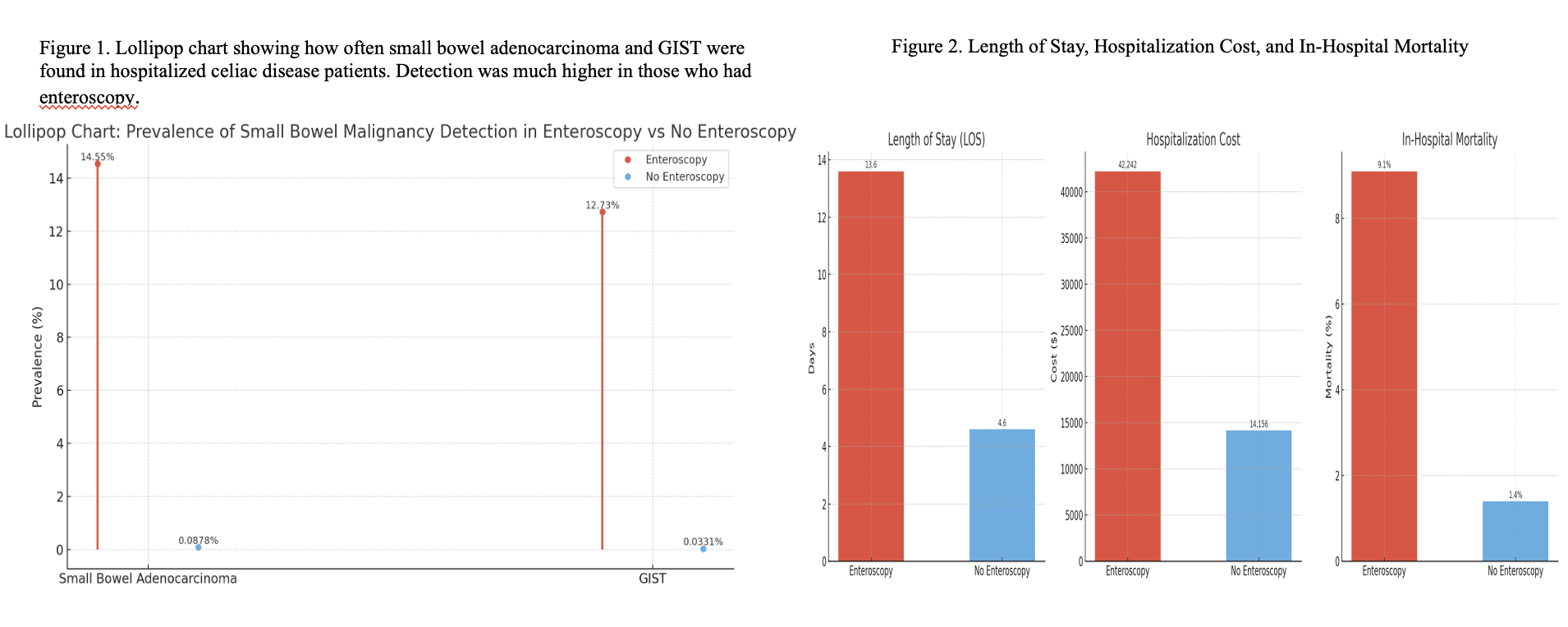
Figure: Table 1: Comparison of primary and secondary outcomes in celiac disease with and without enteroscopy
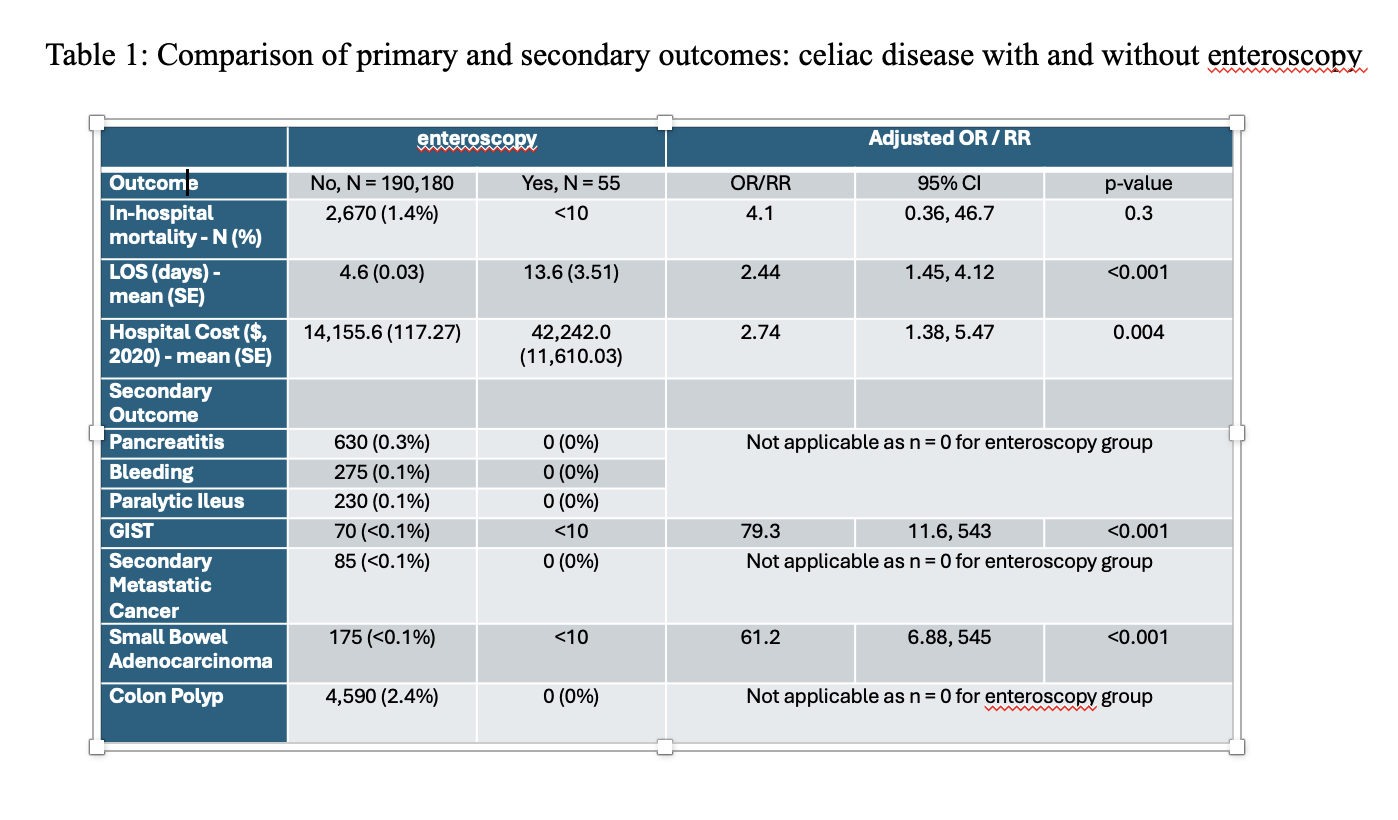
Figure: Figure 1 and Figure 2: Lollipop Chart and Bar Chart of Outcomes
Disclosures:
Anwar Uddin indicated no relevant financial relationships.
Rahat Uddin indicated no relevant financial relationships.
Madia Ahad indicated no relevant financial relationships.
Peter Lymberopoulos indicated no relevant financial relationships.
Savanna Thor indicated no relevant financial relationships.
Anwar Uddin, MD, Rahat Uddin, MS, Madia Ahad, MD, Peter Lymberopoulos, MD, Savanna Thor, DO, MPH. P4024 - Inpatient Enteroscopy in Celiac Disease: A Cross-Sectional Analysis of Utilization, Diagnostic Yield, and Clinical Outcomes From a Nationwide Dataset, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Celiac disease (CD) is a chronic immune-mediated enteropathy that may warrant advanced small bowel evaluation in cases of refractory symptoms, alarm features, or suspected malignancy. Enteroscopy enables deep small bowel visualization and tissue diagnosis but is infrequently performed during hospitalization. Despite its utility, data on its inpatient use, diagnostic yield, and associated outcomes are limited. This study examined national trends, diagnostic performance, and short-term clinical outcomes of inpatient enteroscopy in hospitalized CD patients.
Methods: We performed a retrospective cross-sectional analysis of adult CD hospitalizations in HCUP-NIS (2016–2020). CD and enteroscopy were identified using ICD-10-CM code K90.0 and ICD-10-PCS codes, respectively. Primary outcomes: in-hospital mortality, LOS, and cost. Secondary outcomes: GIST, small bowel adenocarcinoma, and complications (bleeding, pancreatitis, ileus). Survey-weighted multivariable models estimated adjusted odds ratios (aOR), rate ratios, and costs, adjusting for age, sex, race, insurance, Charlson index, and hospital factors.
Results: Among 190,235 CD hospitalizations (2016–2020), only 55 (0.03%) involved inpatient enteroscopy, with no significant change in utilization over time (p = 0.7). Enteroscopy was associated with significantly longer LOS (13.6 ± 3.5 vs 4.6 ± 0.03 days; aRR 2.44, 95% CI: 1.45–4.12; p < 0.001) and higher hospitalization costs ($42,242 vs $14,156; aRR 2.74, 95% CI: 1.38–5.47; p = 0.004). In-hospital mortality was numerically higher (9.1% vs 1.4%) but not statistically significant (aOR 4.1, 95% CI: 0.36–46.7; p = 0.3). Diagnostic yield was notably elevated: small bowel adenocarcinoma and GIST were detected in 14.5% and 12.7% of enteroscopy patients vs 0.09% and 0.03% in controls (aOR 61.2 and 79.3; both p < 0.001). No major complications occurred. These findings suggest inpatient enteroscopy, though rarely used, is highly effective for malignancy detection in high-risk CD cases without observed harm.
Discussion: Inpatient enteroscopy is infrequently used in hospitalized celiac disease patients but is strongly associated with increased diagnostic yield for small bowel malignancies and higher resource utilization. These findings support its targeted use in selected high-risk populations and underscore the need for prospective studies to refine its inpatient role, optimize timing, and guide clinical decision-making.
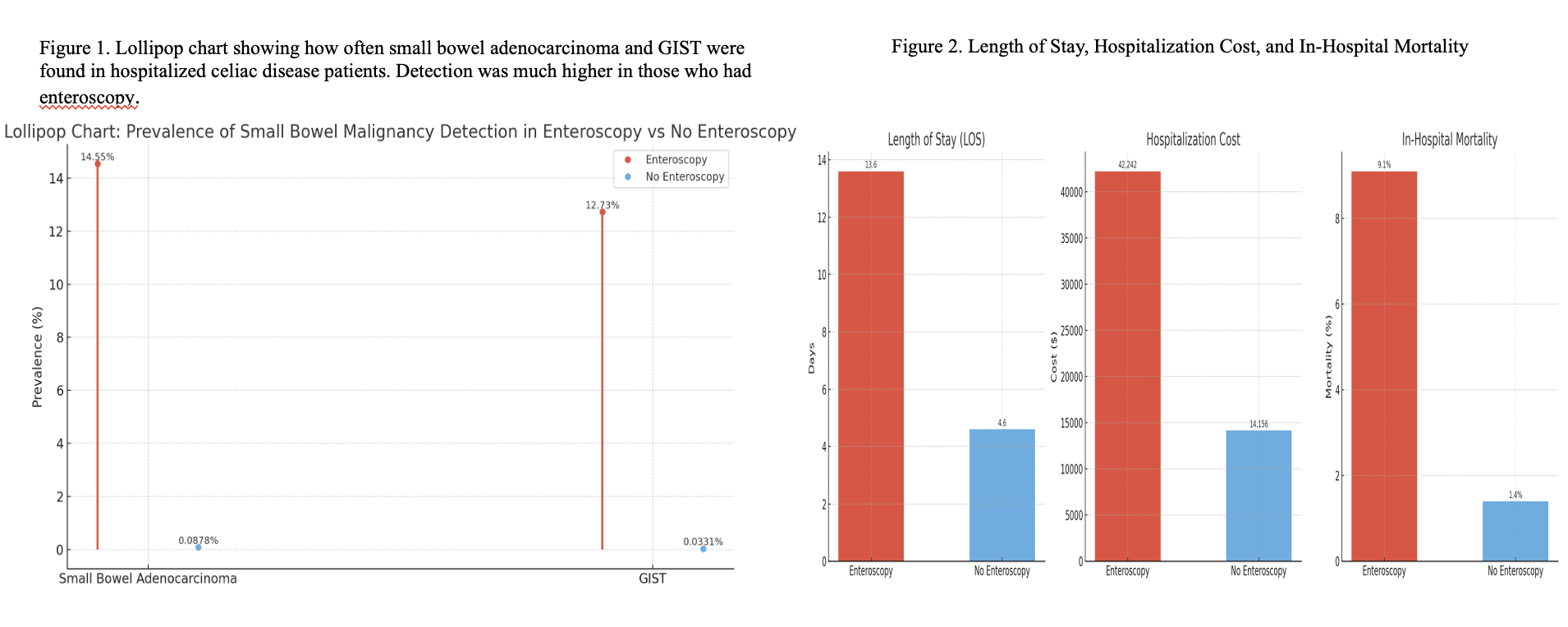
Figure: Table 1: Comparison of primary and secondary outcomes in celiac disease with and without enteroscopy
Figure: Figure 1 and Figure 2: Lollipop Chart and Bar Chart of Outcomes
Disclosures:
Anwar Uddin indicated no relevant financial relationships.
Rahat Uddin indicated no relevant financial relationships.
Madia Ahad indicated no relevant financial relationships.
Peter Lymberopoulos indicated no relevant financial relationships.
Savanna Thor indicated no relevant financial relationships.
Anwar Uddin, MD, Rahat Uddin, MS, Madia Ahad, MD, Peter Lymberopoulos, MD, Savanna Thor, DO, MPH. P4024 - Inpatient Enteroscopy in Celiac Disease: A Cross-Sectional Analysis of Utilization, Diagnostic Yield, and Clinical Outcomes From a Nationwide Dataset, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
