Monday Poster Session
Category: Small Intestine
P4023 - Systemic Sclerosis and Small Bowel Obstruction: A Comprehensive Analysis of Outcomes Using the TriNetX Global Health Database
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Cherechi Nwabueze, MBBS, MPH (she/her/hers)
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Cherechi Nwabueze, MBBS, MPH1, Justin Lam, MD2, Chukwuemelie D. Okeke, MD3, Munachimso Queen. Amadi, MBBS4, Almurtada Razok, MD, MRCP5, Eunice Omeludike, MD6, Favour C. Ezem, MBBS7
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Thomas Jefferson University, Philadelphia, PA; 3Maimonides Medical Center, Brooklyn, NY; 4Northampton General Hospital, Northampton, England, United Kingdom; 5MacNeal Hospital Loyola Medicine, Chicago, IL; 6Piedmont Athens Regional Medical Centre, Athens, GA; 7University of Nigeria teaching hospital Ituku Ozalla, Lagos, Lagos, Nigeria
Introduction: Systemic sclerosis (SSc) causes small bowel obstruction (SBO) through progressive smooth muscle atrophy and fibrosis, leading to hypoperistalsis and significant morbidity/mortality. Despite its clinical relevance, data on SBO outcomes in SSc remain limited. This study compares these outcomes using a large multi-institutional database.
Methods: This retrospective cohort study utilized TriNetX global research network from 146 healthcare organizations. Two cohorts were defined: adults ≥ 18years with both SBO and SSc (Cohort A) and adults with only SBO (Cohort B). A comparative outcome analysis was performed evaluating all-cause mortality, sepsis, malnutrition, DVT/PE, GI bleeding, bowel perforation, small intestinal bacterial overgrowth (SIBO), inpatient hospitalizations, and use of total parenteral nutrition (TPN), over a 20-year follow-up period (2005- 2025). Propensity score matching was used to balance baseline demographic and clinical characteristics.
Results: The study included 2,455 patients with both SSc and SBO (Cohort A) and 620,485 patients with only SBO (Cohort B). After 1:1 propensity score matching, 2,323 patients from each cohort were compared. Patients in Cohort A had higher all-cause mortality risk (30% vs. 20%; RR 1.46, p < 0.001), and poorer survival (61% vs. 73%; χ² = 52.58, p< 0.001). Patients in Cohort A were 64% more likely to become malnourished (RR 1.64, p< 0.0001), with 71% remaining malnutrition-free compared to 83% in Cohort B by the end of the study period (χ² = 42.75, p< 0.001). Patients with SSc were 24% more likely to develop sepsis (RR 1.24, p < 0.001), with 79% remaining sepsis-free compared to 84% in Cohort B at the end of the study period (χ² = 7.99, p = 0.005). Although absolute risks of DVT/PE and GI bleeding were similar between cohorts, cumulative incidence of these events was significantly higher in Cohort A (for DVT/PE: χ² = 4.74, p = 0.03; for GI bleeding: χ² = 4.77, p = 0.03). No significant differences were observed in the risk of bowel perforation, SIBO, or need for TPN between the two groups, and survival probabilities at the end of follow-up were similar. Patients with SSc had more inpatient hospitalizations (mean 8, SD =13 vs.7, SD =11; t =2.96, p =0.003).
Discussion: SSc patients with SBO had worse outcomes than non-SSc patients, including higher risks of death, malnutrition, sepsis, and more frequent hospitalizations. This highlights need for close monitoring and proactive management. Further research is needed to explore these associations.
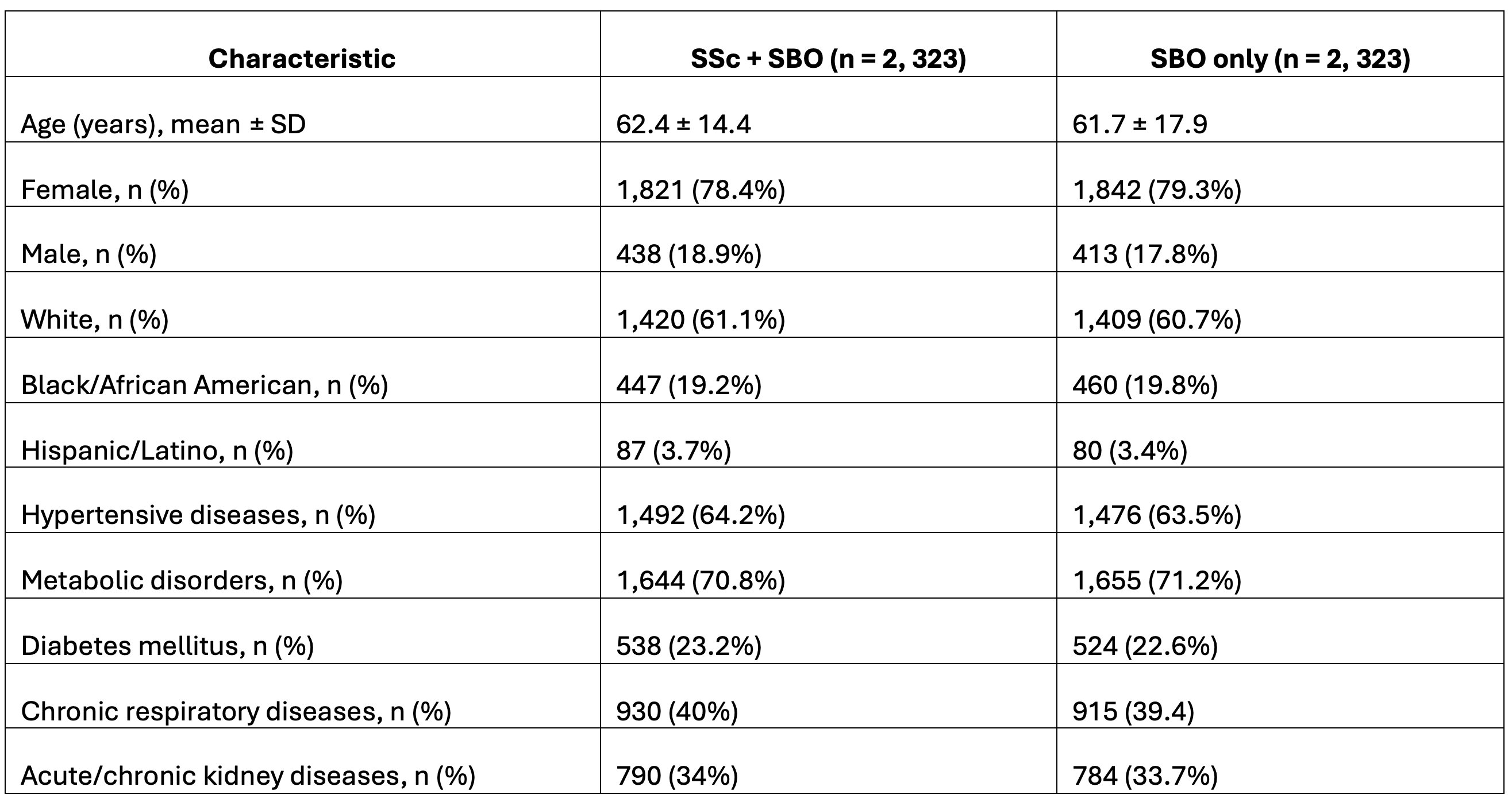
Figure: Table 1: Baseline Characteristics of Patients with Small Bowel Obstruction (SBO), with and without Systemic Sclerosis (SSc) after Propensity Score Matching
Disclosures:
Cherechi Nwabueze indicated no relevant financial relationships.
Justin Lam indicated no relevant financial relationships.
Chukwuemelie Okeke indicated no relevant financial relationships.
Munachimso Amadi indicated no relevant financial relationships.
Almurtada Razok indicated no relevant financial relationships.
Eunice Omeludike indicated no relevant financial relationships.
Favour Ezem indicated no relevant financial relationships.
Cherechi Nwabueze, MBBS, MPH1, Justin Lam, MD2, Chukwuemelie D. Okeke, MD3, Munachimso Queen. Amadi, MBBS4, Almurtada Razok, MD, MRCP5, Eunice Omeludike, MD6, Favour C. Ezem, MBBS7. P4023 - Systemic Sclerosis and Small Bowel Obstruction: A Comprehensive Analysis of Outcomes Using the TriNetX Global Health Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Thomas Jefferson University, Philadelphia, PA; 3Maimonides Medical Center, Brooklyn, NY; 4Northampton General Hospital, Northampton, England, United Kingdom; 5MacNeal Hospital Loyola Medicine, Chicago, IL; 6Piedmont Athens Regional Medical Centre, Athens, GA; 7University of Nigeria teaching hospital Ituku Ozalla, Lagos, Lagos, Nigeria
Introduction: Systemic sclerosis (SSc) causes small bowel obstruction (SBO) through progressive smooth muscle atrophy and fibrosis, leading to hypoperistalsis and significant morbidity/mortality. Despite its clinical relevance, data on SBO outcomes in SSc remain limited. This study compares these outcomes using a large multi-institutional database.
Methods: This retrospective cohort study utilized TriNetX global research network from 146 healthcare organizations. Two cohorts were defined: adults ≥ 18years with both SBO and SSc (Cohort A) and adults with only SBO (Cohort B). A comparative outcome analysis was performed evaluating all-cause mortality, sepsis, malnutrition, DVT/PE, GI bleeding, bowel perforation, small intestinal bacterial overgrowth (SIBO), inpatient hospitalizations, and use of total parenteral nutrition (TPN), over a 20-year follow-up period (2005- 2025). Propensity score matching was used to balance baseline demographic and clinical characteristics.
Results: The study included 2,455 patients with both SSc and SBO (Cohort A) and 620,485 patients with only SBO (Cohort B). After 1:1 propensity score matching, 2,323 patients from each cohort were compared. Patients in Cohort A had higher all-cause mortality risk (30% vs. 20%; RR 1.46, p < 0.001), and poorer survival (61% vs. 73%; χ² = 52.58, p< 0.001). Patients in Cohort A were 64% more likely to become malnourished (RR 1.64, p< 0.0001), with 71% remaining malnutrition-free compared to 83% in Cohort B by the end of the study period (χ² = 42.75, p< 0.001). Patients with SSc were 24% more likely to develop sepsis (RR 1.24, p < 0.001), with 79% remaining sepsis-free compared to 84% in Cohort B at the end of the study period (χ² = 7.99, p = 0.005). Although absolute risks of DVT/PE and GI bleeding were similar between cohorts, cumulative incidence of these events was significantly higher in Cohort A (for DVT/PE: χ² = 4.74, p = 0.03; for GI bleeding: χ² = 4.77, p = 0.03). No significant differences were observed in the risk of bowel perforation, SIBO, or need for TPN between the two groups, and survival probabilities at the end of follow-up were similar. Patients with SSc had more inpatient hospitalizations (mean 8, SD =13 vs.7, SD =11; t =2.96, p =0.003).
Discussion: SSc patients with SBO had worse outcomes than non-SSc patients, including higher risks of death, malnutrition, sepsis, and more frequent hospitalizations. This highlights need for close monitoring and proactive management. Further research is needed to explore these associations.
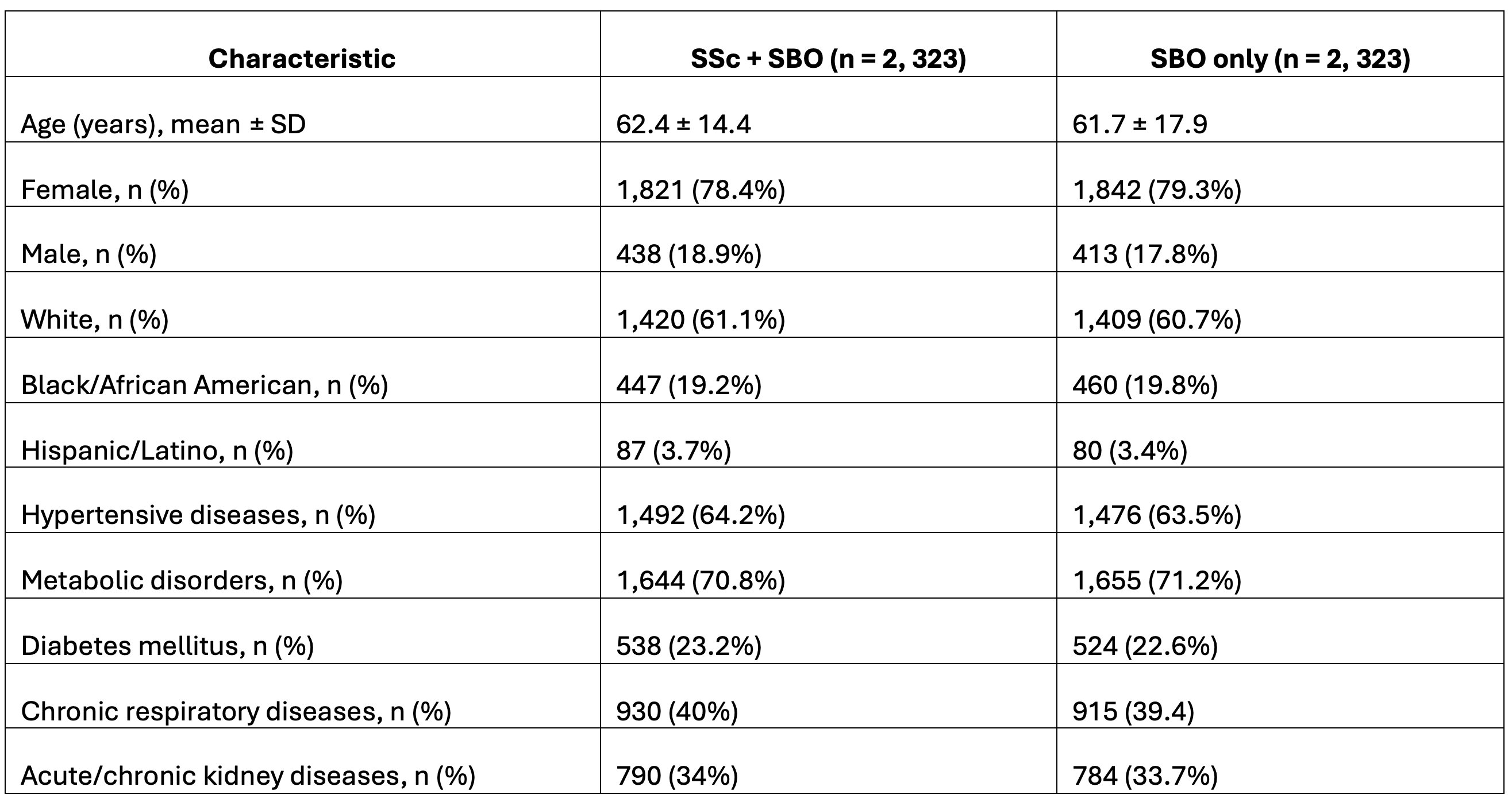
Figure: Table 1: Baseline Characteristics of Patients with Small Bowel Obstruction (SBO), with and without Systemic Sclerosis (SSc) after Propensity Score Matching
Disclosures:
Cherechi Nwabueze indicated no relevant financial relationships.
Justin Lam indicated no relevant financial relationships.
Chukwuemelie Okeke indicated no relevant financial relationships.
Munachimso Amadi indicated no relevant financial relationships.
Almurtada Razok indicated no relevant financial relationships.
Eunice Omeludike indicated no relevant financial relationships.
Favour Ezem indicated no relevant financial relationships.
Cherechi Nwabueze, MBBS, MPH1, Justin Lam, MD2, Chukwuemelie D. Okeke, MD3, Munachimso Queen. Amadi, MBBS4, Almurtada Razok, MD, MRCP5, Eunice Omeludike, MD6, Favour C. Ezem, MBBS7. P4023 - Systemic Sclerosis and Small Bowel Obstruction: A Comprehensive Analysis of Outcomes Using the TriNetX Global Health Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
