Monday Poster Session
Category: Small Intestine
P4097 - Unmasking Primary Jejunal Angiosarcoma: A Rare and Lethal Small Bowel Tumor
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Amla Patel, MBBS (she/her/hers)
Creighton University, Phoenix
Phoenix, AZ
Presenting Author(s)
Amla Patel, MBBS1, Vishnu Yanamaladoddi, MD2, Sunny Kumar, MD3, Vikash Kumar, MD2, Indu Srinivasan, MD2
1Creighton University, Phoenix, Phoenix, AZ; 2Creighton University School of Medicine, Phoenix, AZ; 3Wright Center for Graduate Medical Education, Scranton, PA
Introduction: Small bowel angiosarcomas are exceedingly rare vascular neoplasms, with fewer than 65 cases reported in the literature. Their nonspecific clinical presentation, deep anatomic location, and aggressive behavior, attributable to their origin from vascular or lymphatic endothelium, often result in delayed diagnosis and early metastatic potential. We report a case of a 48 year old male who presented with melena and was ultimately diagnosed with biopsy proven primary jejunal angiosarcoma.
Case Description/
Methods: A 48-year-old male with no prior medical history was admitted following a motor vehicle collision with multiple traumatic injuries, including pelvic fractures, ureteral transection, and retroperitoneal/mesenteric hematomas. During hospitalization, he developed melena and acute anemia requiring transfusion. CT angiography of abdomen was negative, and EGD revealed chronic gastritis. Continued bleeding prompted colonoscopy, identifying a rectal ulcer likely from a rectal tube and push enteroscopy revealed a 1.5 cm ulcerated lesion in the proximal jejunum. Surgical resection of a 10 mm jejunal tumor was performed, 57 cm from the ligament of Treitz. Histopathology demonstrated poorly formed vascular channels lined by atypical endothelial cells, strongly positive for CD31 and negative for CD117, consistent with jejunal angiosarcoma. Oncology recommended surveillance imaging every 8-12 weeks for the first two years. The patient was briefly lost to follow-up but was recently seen, with repeat imaging showing no recurrence.
Discussion: Small bowel angiosarcomas are rare, aggressive vascular tumors, comprising less than 1–2% of all gastrointestinal malignancies. Typically affecting males in the 6th to 7th decade, they often present with nonspecific symptoms such as abdominal pain, melena, or hematochezia, contributing to delayed diagnosis. Risk factors may include prior radiation exposure and genetic predisposition. Metastasis commonly involves the liver, lungs, and peritoneum. Diagnosis relies on imaging (CT, MRI, PET) and histopathology, which shows anaplastic, atypical endothelial cells with anastomosing vasculature. Immunohistochemistry is critical, with CD31, CD34, and von Willebrand factor aiding in diagnosis. Localized tumors with negative margins may undergo surveillance or receive adjuvant paclitaxel due to high recurrence risk. Metastatic cases are managed with systemic chemotherapy. Due to its rarity, a multidisciplinary approach is essential for diagnosis, treatment, and follow-up.
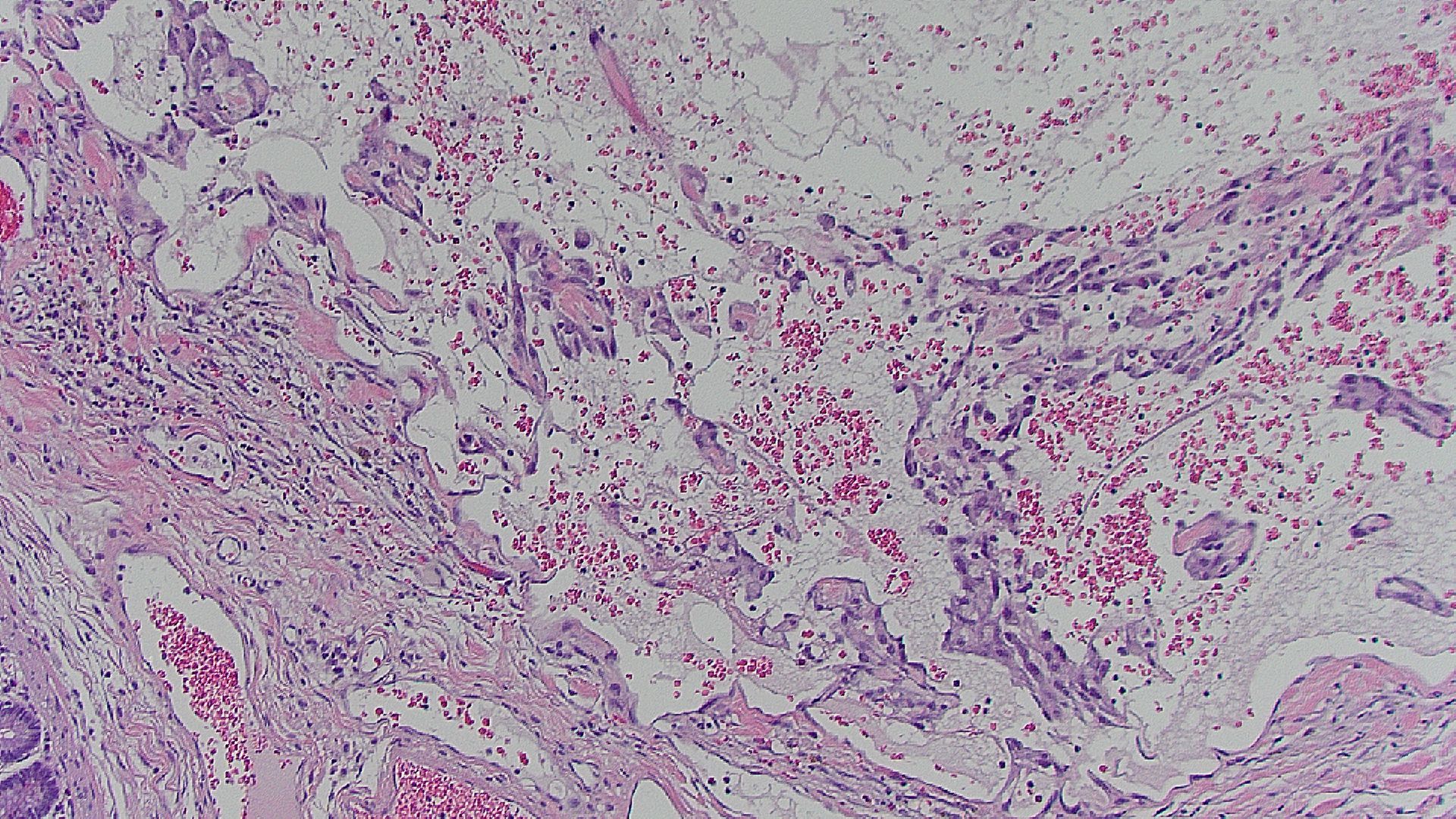
Figure: High power field histopathological slide of the jejunal angiosarcoma, with irregularly shaped anastomosing vascular channels and nuclear atypia
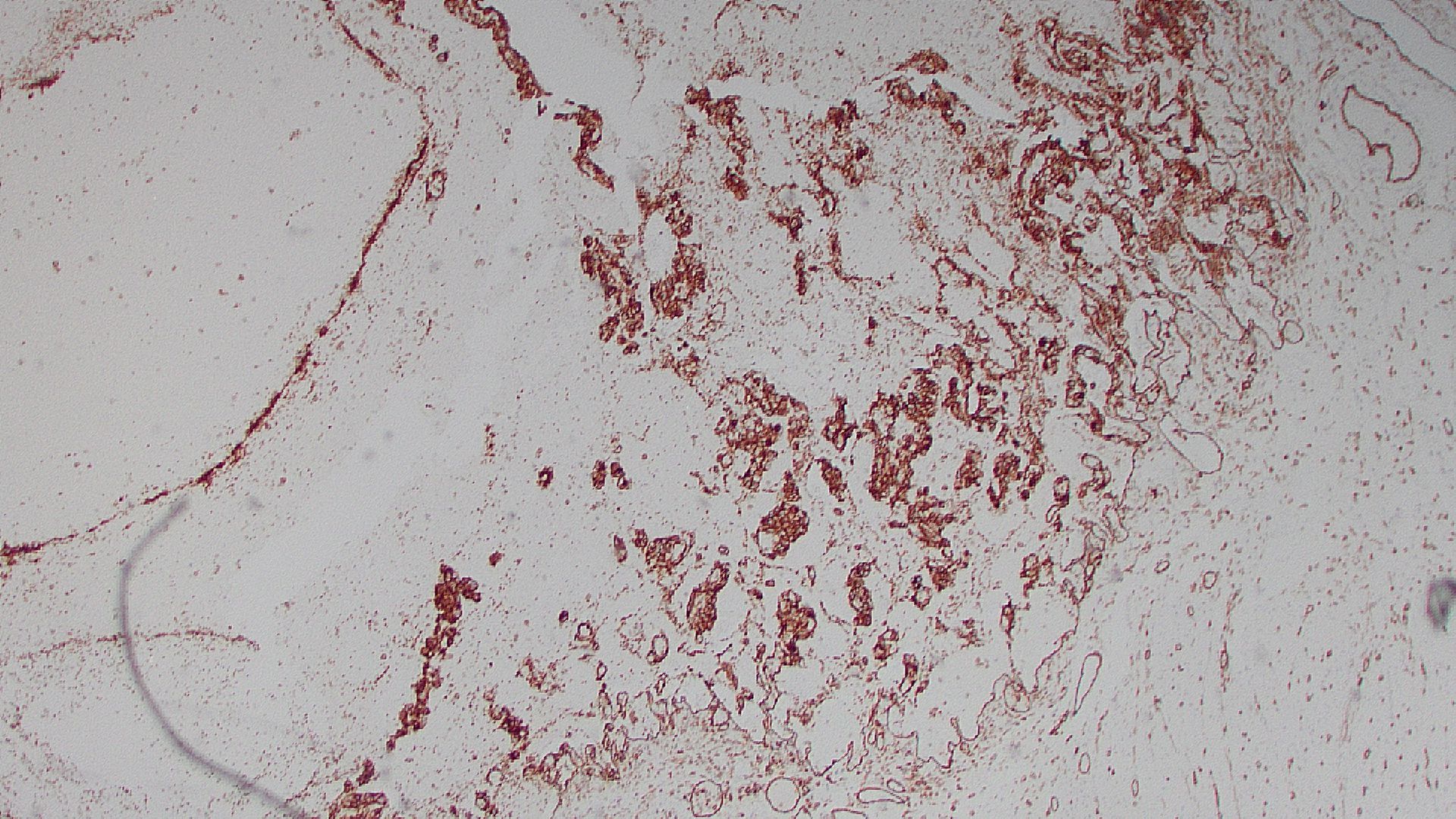
Figure: Immunohistochemistry showing positive CD31 staining in endothelial cells (seen as brown stain), classically seen in angiosarcomas, surrounded by intestinal tissue
Disclosures:
Amla Patel indicated no relevant financial relationships.
Vishnu Yanamaladoddi indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Indu Srinivasan indicated no relevant financial relationships.
Amla Patel, MBBS1, Vishnu Yanamaladoddi, MD2, Sunny Kumar, MD3, Vikash Kumar, MD2, Indu Srinivasan, MD2. P4097 - Unmasking Primary Jejunal Angiosarcoma: A Rare and Lethal Small Bowel Tumor, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Creighton University, Phoenix, Phoenix, AZ; 2Creighton University School of Medicine, Phoenix, AZ; 3Wright Center for Graduate Medical Education, Scranton, PA
Introduction: Small bowel angiosarcomas are exceedingly rare vascular neoplasms, with fewer than 65 cases reported in the literature. Their nonspecific clinical presentation, deep anatomic location, and aggressive behavior, attributable to their origin from vascular or lymphatic endothelium, often result in delayed diagnosis and early metastatic potential. We report a case of a 48 year old male who presented with melena and was ultimately diagnosed with biopsy proven primary jejunal angiosarcoma.
Case Description/
Methods: A 48-year-old male with no prior medical history was admitted following a motor vehicle collision with multiple traumatic injuries, including pelvic fractures, ureteral transection, and retroperitoneal/mesenteric hematomas. During hospitalization, he developed melena and acute anemia requiring transfusion. CT angiography of abdomen was negative, and EGD revealed chronic gastritis. Continued bleeding prompted colonoscopy, identifying a rectal ulcer likely from a rectal tube and push enteroscopy revealed a 1.5 cm ulcerated lesion in the proximal jejunum. Surgical resection of a 10 mm jejunal tumor was performed, 57 cm from the ligament of Treitz. Histopathology demonstrated poorly formed vascular channels lined by atypical endothelial cells, strongly positive for CD31 and negative for CD117, consistent with jejunal angiosarcoma. Oncology recommended surveillance imaging every 8-12 weeks for the first two years. The patient was briefly lost to follow-up but was recently seen, with repeat imaging showing no recurrence.
Discussion: Small bowel angiosarcomas are rare, aggressive vascular tumors, comprising less than 1–2% of all gastrointestinal malignancies. Typically affecting males in the 6th to 7th decade, they often present with nonspecific symptoms such as abdominal pain, melena, or hematochezia, contributing to delayed diagnosis. Risk factors may include prior radiation exposure and genetic predisposition. Metastasis commonly involves the liver, lungs, and peritoneum. Diagnosis relies on imaging (CT, MRI, PET) and histopathology, which shows anaplastic, atypical endothelial cells with anastomosing vasculature. Immunohistochemistry is critical, with CD31, CD34, and von Willebrand factor aiding in diagnosis. Localized tumors with negative margins may undergo surveillance or receive adjuvant paclitaxel due to high recurrence risk. Metastatic cases are managed with systemic chemotherapy. Due to its rarity, a multidisciplinary approach is essential for diagnosis, treatment, and follow-up.
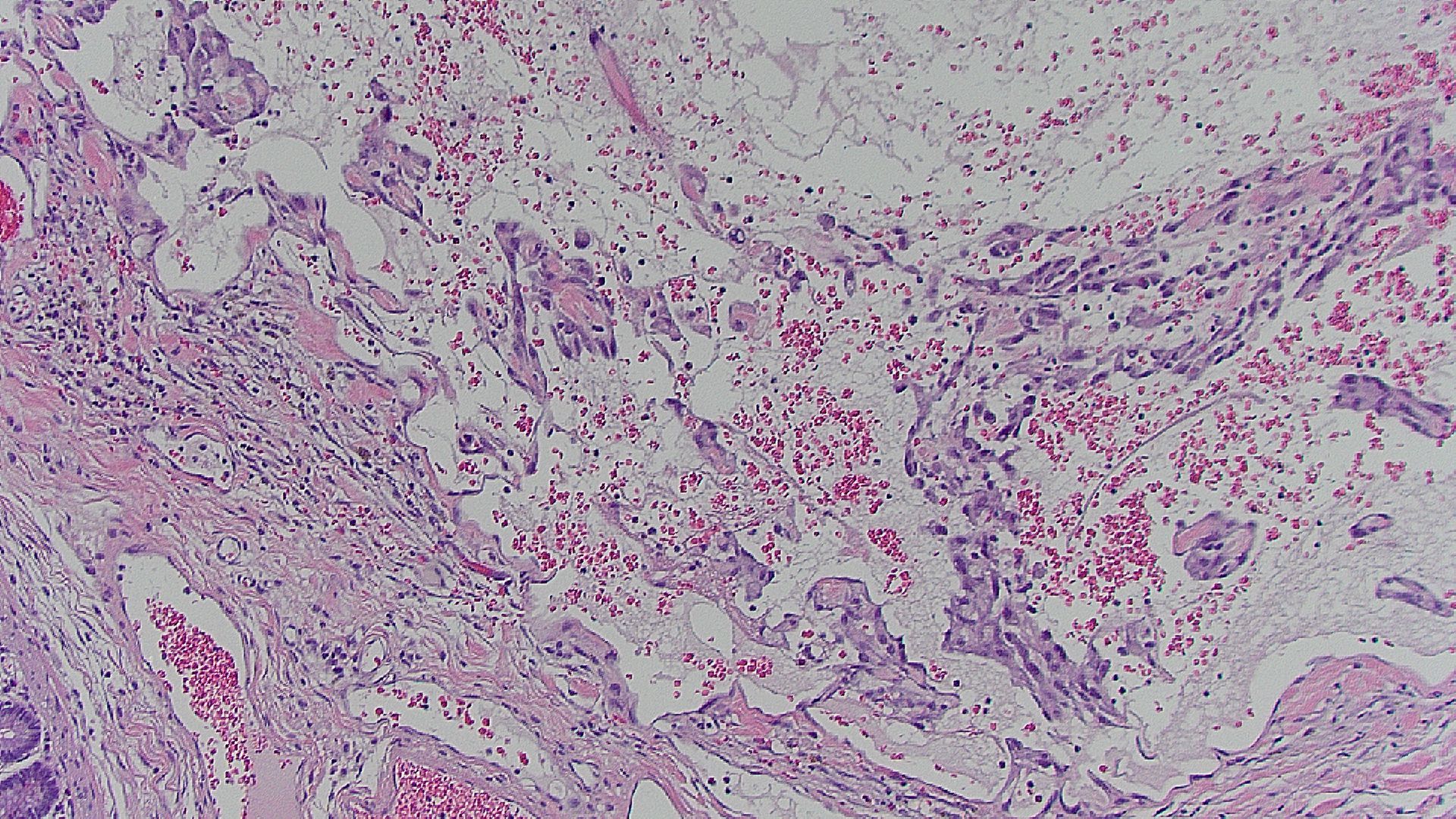
Figure: High power field histopathological slide of the jejunal angiosarcoma, with irregularly shaped anastomosing vascular channels and nuclear atypia
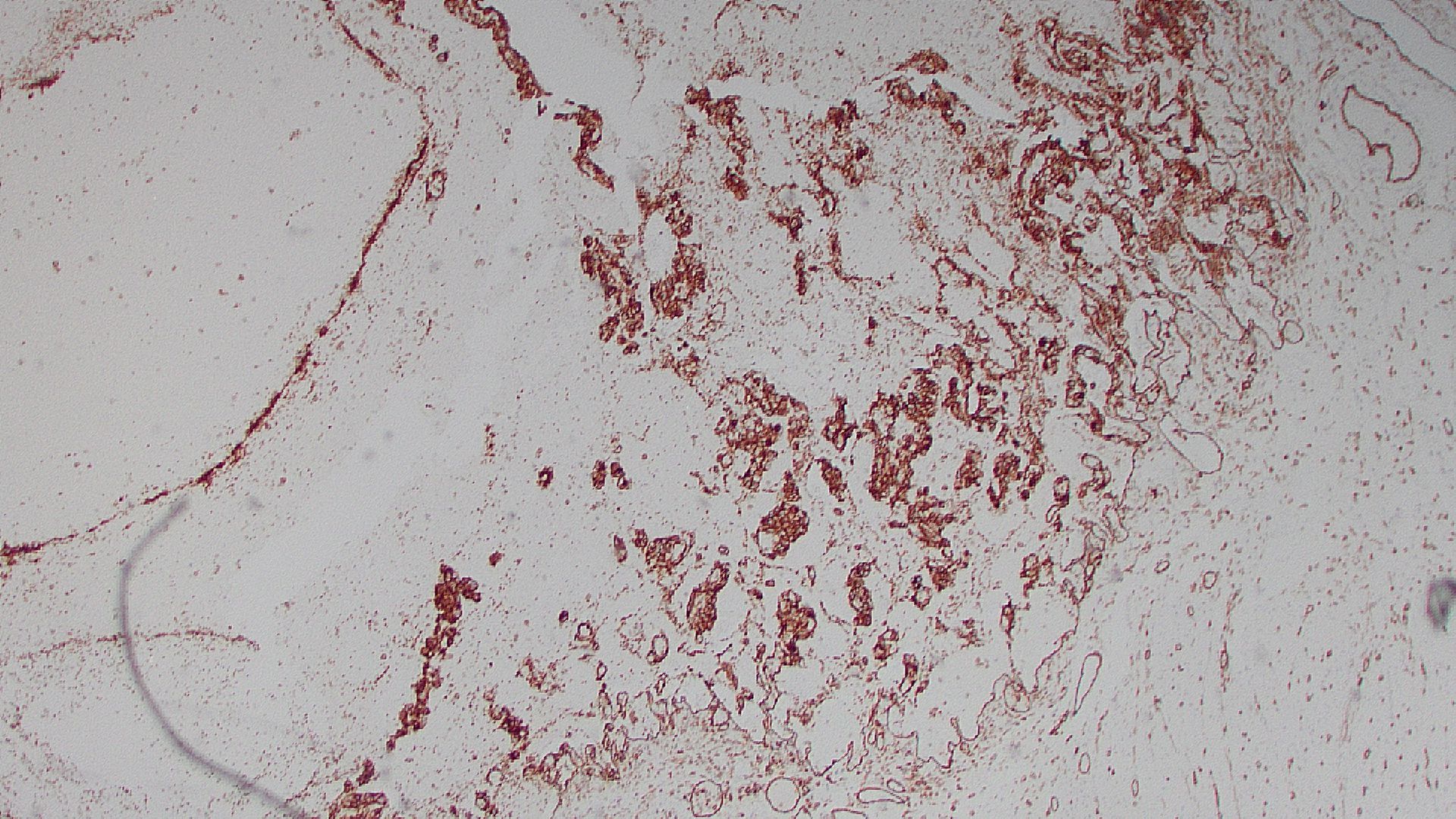
Figure: Immunohistochemistry showing positive CD31 staining in endothelial cells (seen as brown stain), classically seen in angiosarcomas, surrounded by intestinal tissue
Disclosures:
Amla Patel indicated no relevant financial relationships.
Vishnu Yanamaladoddi indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Indu Srinivasan indicated no relevant financial relationships.
Amla Patel, MBBS1, Vishnu Yanamaladoddi, MD2, Sunny Kumar, MD3, Vikash Kumar, MD2, Indu Srinivasan, MD2. P4097 - Unmasking Primary Jejunal Angiosarcoma: A Rare and Lethal Small Bowel Tumor, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
