Monday Poster Session
Category: Small Intestine
P4091 - Mucinous Adenocarcinoma of the Jejunum: A Rare Cancer of the Gastrointestinal Tract
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- JJ
Jason John, MD
Orlando VA Medical Center and UCF/HCA Greater Orlando
Orlando, FL
Presenting Author(s)
Jason John, MD1, Jignesh Parikh, MD2, Amar Mandalia, MD3
1Orlando VA Medical Center and UCF/HCA Greater Orlando, Orlando, FL; 2Orlando VA Medical Center and UCF/HCA Greater Orlando, Kissimmee, FL; 3Orlando VA Healthcare System, Orlando, FL
Introduction: Small bowel malignancies are rare, accounting for around 3-5% of all gastrointestinal (GI) malignancies even though the small bowel comprises 75% of the length of the entire GI tract. The most frequent location is the duodenum followed by the jejunum.
Case Description/
Methods: A 49-year-old male with past medical history of DM2, HLD, OSA, CAD presented to clinic for workup of iron deficiency anemia. He denied overt GI bleeding, dysphagia, abdominal pain, diarrhea. There was no family history of GI cancers. His baseline Hgb was 13.5, however, a year later, his hemoglobin was 7.9 with MCV of 73. EGD and colonoscopy were performed. The colonoscopy was normal, however, the EGD revealed a non-bleeding 1.2 cm jejunal ulcer (Figure 1) with no stigmata of bleeding. Biopsies revealed possible dysplastic cells but no clear evidence of malignancy. Double balloon enteroscopy was thus performed and biopsies were taken again which then revealed jejunal adenocarcinoma with mucinous features (Figure 2). PET and CT thorax, abdomen, pelvis revealed no evidence of distant metastasis. CEA was 14.5. A multidisciplinary board reviewed the case and recommended surgical resection. Complete resection was performed and final surgical pathology revealed T4N0 moderately differentiated mucinous adenocarcinoma with clear margins. The patient was started and is currently undergoing chemotherapy with 5-fluorouracil/leucovorin/oxaliplatin (FOLFOX).
Discussion: Jejunal adenocarcinomas (JA) are rare and most commonly occur around the age of 60. The histological variant, jejunal mucinous adenocarcinoma (JMA), is rarer with only a few cases having been reported in the literature. The environment of the small bowel is typically anti-neoplastic. JA’s can present asymptomatically with microcytic anemia as the only sign of development like in our patient. If symptomatic, patients present with symptoms of abdominal discomfort, nausea, vomiting, and bleeding. The diagnosis is often delayed due to non-specific symptoms, poorly defined diagnostic modalities, and rare prevalence. Reports indicate over 80% of JAs being diagnosed at stage III or stage IV disease. The treatment of choice remains complete resection, with complete tumor removal with clear margins offering the best overall survival. The role and efficacy of chemotherapy remain unclear. To date, no standard adjuvant regimen has been rendered truly effective against SBA. Physicians should consider JA’s for patients presenting with non-specific GI complaints and microcytic anemia.
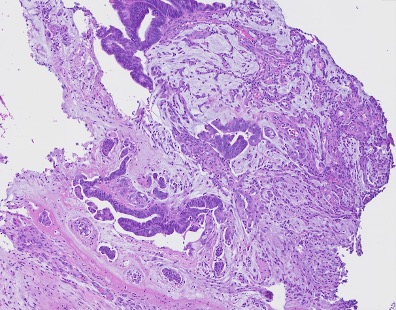
Figure: Figure 1: jejunal ulcer
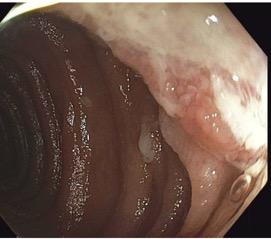
Figure: Figure 2: malignant glands floating and surrounded by mucin pool, findings are consistent with mucinous adenocarcinoma
Disclosures:
Jason John indicated no relevant financial relationships.
Jignesh Parikh indicated no relevant financial relationships.
Amar Mandalia indicated no relevant financial relationships.
Jason John, MD1, Jignesh Parikh, MD2, Amar Mandalia, MD3. P4091 - Mucinous Adenocarcinoma of the Jejunum: A Rare Cancer of the Gastrointestinal Tract, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Orlando VA Medical Center and UCF/HCA Greater Orlando, Orlando, FL; 2Orlando VA Medical Center and UCF/HCA Greater Orlando, Kissimmee, FL; 3Orlando VA Healthcare System, Orlando, FL
Introduction: Small bowel malignancies are rare, accounting for around 3-5% of all gastrointestinal (GI) malignancies even though the small bowel comprises 75% of the length of the entire GI tract. The most frequent location is the duodenum followed by the jejunum.
Case Description/
Methods: A 49-year-old male with past medical history of DM2, HLD, OSA, CAD presented to clinic for workup of iron deficiency anemia. He denied overt GI bleeding, dysphagia, abdominal pain, diarrhea. There was no family history of GI cancers. His baseline Hgb was 13.5, however, a year later, his hemoglobin was 7.9 with MCV of 73. EGD and colonoscopy were performed. The colonoscopy was normal, however, the EGD revealed a non-bleeding 1.2 cm jejunal ulcer (Figure 1) with no stigmata of bleeding. Biopsies revealed possible dysplastic cells but no clear evidence of malignancy. Double balloon enteroscopy was thus performed and biopsies were taken again which then revealed jejunal adenocarcinoma with mucinous features (Figure 2). PET and CT thorax, abdomen, pelvis revealed no evidence of distant metastasis. CEA was 14.5. A multidisciplinary board reviewed the case and recommended surgical resection. Complete resection was performed and final surgical pathology revealed T4N0 moderately differentiated mucinous adenocarcinoma with clear margins. The patient was started and is currently undergoing chemotherapy with 5-fluorouracil/leucovorin/oxaliplatin (FOLFOX).
Discussion: Jejunal adenocarcinomas (JA) are rare and most commonly occur around the age of 60. The histological variant, jejunal mucinous adenocarcinoma (JMA), is rarer with only a few cases having been reported in the literature. The environment of the small bowel is typically anti-neoplastic. JA’s can present asymptomatically with microcytic anemia as the only sign of development like in our patient. If symptomatic, patients present with symptoms of abdominal discomfort, nausea, vomiting, and bleeding. The diagnosis is often delayed due to non-specific symptoms, poorly defined diagnostic modalities, and rare prevalence. Reports indicate over 80% of JAs being diagnosed at stage III or stage IV disease. The treatment of choice remains complete resection, with complete tumor removal with clear margins offering the best overall survival. The role and efficacy of chemotherapy remain unclear. To date, no standard adjuvant regimen has been rendered truly effective against SBA. Physicians should consider JA’s for patients presenting with non-specific GI complaints and microcytic anemia.
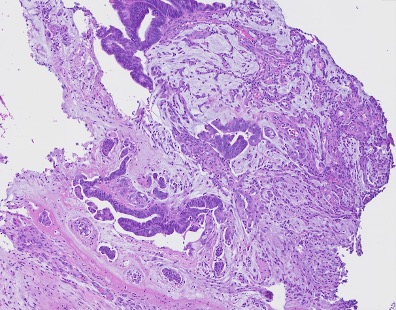
Figure: Figure 1: jejunal ulcer
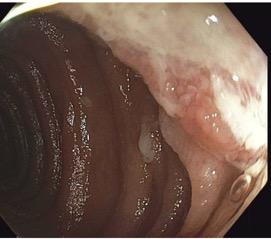
Figure: Figure 2: malignant glands floating and surrounded by mucin pool, findings are consistent with mucinous adenocarcinoma
Disclosures:
Jason John indicated no relevant financial relationships.
Jignesh Parikh indicated no relevant financial relationships.
Amar Mandalia indicated no relevant financial relationships.
Jason John, MD1, Jignesh Parikh, MD2, Amar Mandalia, MD3. P4091 - Mucinous Adenocarcinoma of the Jejunum: A Rare Cancer of the Gastrointestinal Tract, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
